Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Amir Naeh and Version 2 by Amina Yu.
Gestational diabetes mellitus (GDM) complicates between 5 and 12% of pregnancies, with
associated maternal, fetal, and neonatal complications. The ideal screening and diagnostic criteria
to diagnose and treat GDM have not been established, and in recent years, significant research has been undertaken to identify a first-trimester biomarker that can predict GDM later in pregnancy, enable early intervention, and reduce GDM-related adverse outcomes. This review summarizes current data on first-trimester biomarkers, the advantages, and the
limitations.
- gestational diabetes
- biomarkers
- early prediction
- pregnancy complications
1. Predicting GDM by Maternal Risk Factors
Table 1. Clinical risk factors with corresponding odds ratios for gestational diabetes mellitus.
| Risk Factor | Odds Ratio | |||||
|---|---|---|---|---|---|---|
| Suggested Involvement in GDM Pathophysiology | ||||||
| 1. Ethnicity: Asian, Middle Eastern, Hispanic, Latino, African American, and Indigenous | 2.32 [1] | 2.32 [26] | ||||
| 2. Maternal age ≥35 years | 3.54 [ | |||||
| Adiponectin | Modulation of glucose and fatty acid metabolism. Involvement in inflammation, apoptosis, and angiogenesis. | Low levels associated with decreased insulin sensitivity and GDM | ||||
| 2 | ] | 3.54 [27] | ||||
| Leptin | Regulation of energy balance and expenditure. Role in hormone regulation and immunity. | High leptin levels cause hyperinsulinemia and increase insulin resistance | 3. Pre-pregnancy BMI >25 kg/m | 2 | 2.14 [3] | 2.14 [28] |
| 4. Polycystic ovary syndrome | ||||||
| PAPP-A | Increase bioavailability of IGF-1 and promotes somatic growth. Involvement in wound healing and bone remodelling. | Decreased levels contribute to an increase in insulin resistance | 2.32 [4] | 2.32 [29] | ||
| PLGF | Vascular endothelial growth factor-like protein. Role in angiogenesis and placentation. | High PLGF levels promote the abnormal vascular network in placentas of GDM pregnancies | 5. GDM in a previous pregnancy | 5.9 [1] | 5.9 [26] | |
| TNF-α | Inflammatory cytokine involved in the regulation of immune cells, inflammation, and autoimmune diseases. | Increased levels impair insulin signalling and beta-cell function, leading to insulin resistance and GDM | 6. Previous delivery of macrocosmic baby (birth weight >4000 gr or >90th centile) | 1.54 [1] | 1.54 [26] | |
| CRP | Acute-phase reactant. Role in tissue injury, inflammation, and infection. | High levels associated with insulin resistance and systemic inflammation | 7. Family history of diabetes (1st-degree relative) | 1.36 [1] | 1.36 [26] | |
| IL-6 | 8. Multiple pregnancy | 1.13 [5] | 1.13 [30] | |||
| 9. Assisted reproductive technology | 1.26 [6] | 1.26 [31] |
BMI—body mass index and GDM—gestational diabetes mellitus.
2. Predicting GDM Using Individual Biomarkers
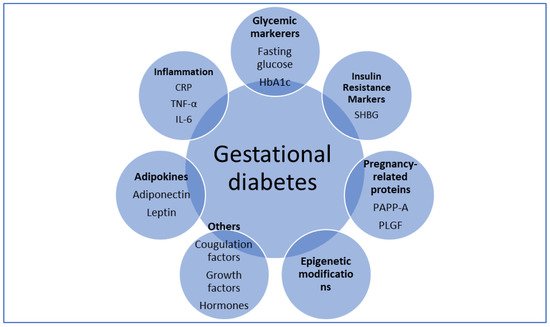
Figure 1. Overview of tested biomarkers. CRP—C-reactive protein; IL-6—interleukin 6; PAPP-A—pregnancy-associated plasma protein A; PLGF—placental growth factor; SHBG—sex hormone-binding globulin; and TNF-α—tumor necrosis factor α.
Table 2. Potential biomarkers for gestational diabetes mellitus.
| Biomarker | Function |
|---|---|
| Circulating inflammatory cytokine. Role in immune response regulation, inflammation, and hematopoiesis. | |
| Increased secretion by adipocytes and placental cells, leading to a chronic inflammatory process and insulin resistance | |
| SHBG | |
| Glycoprotein that binds androgen and estrogen. | Decrease SHBG levels associated with hyperinsulinemia and GDM |
3. Predicting GDM by Early Glycemic Markers
3.1. Fasting Glucose
In 2010, the International Association of Diabetes and Pregnancy Study Group recommended different thresholds for diagnosis and classification of hyperglycemia in pregnancy based on the results of the HAPO study [7][39]. The panel recommended the use of first-trimester fasting glucose above 92 mg/dL to diagnose early GDM; however, this approach was criticized due to a lack of evidence [8][9][38,40]. Although not established as a diagnostic marker, several studies have demonstrated an association between first-trimester fasting glucose and GDM development in late pregnancy. Mashiah et al. showed strong, graded associations between fasting glucose levels in the first trimester and GDM development, macrosomia, and cesarean section [10][41]. Other studies have shown that elevated first-trimester fasting glucose levels have sensitivities of 47–75% and specificities of 52–77% for the prediction of GDM later in pregnancy [11][12][42,43], making the predictive value of fasting glucose similar to the risk factor of BMI [11][42]. Nevertheless, a definitive clinically useful cut-off for first-trimester fasting glucose has not been established and results show an insufficient predictive value for this marker.
3.2. HbA1c
HbA1c is used to estimate average blood glucose over the lifespan of a red blood cell (~120 days). HbA1c does not require fasting and is used in non-pregnant populations to diagnose and monitor both pre-diabetes and diabetes [13][44]. Several studies demonstrated that a first-trimester HbA1c in the pre-diabetic values (5.7–6.4%) is correlated with GDM manifestation in late pregnancy and associated with adverse pregnancy outcomes [14][15][16][45,46,47]. Although a significant risk factor for GDM, the low sensitivity of HbA1c in this range makes it a poor test to identify women who will develop GDM [15][46]. HbA1c levels are also subjected to pregnancy changes and possibly require pregnancy-specific reference ranges [17][48]. Finally, Osmundson et al. conducted a randomized control trial which showed that treatment of women with early (before 14 weeks’ gestation) pre-diabetic HbA1c (5.7–6.4%) did not reduce the risk of GDM later in pregnancy, except in non-obese women [18][49]. In summary, current evidence does not support the use of HbA1c as an effective early predictor for GDM.
4. Predicting GDM by Adipokines
4.1. Adiponectin
Adiponectin is a protein secreted primarily by the adipose tissue but also by the brain, skeletal muscle, and placenta [19][55]. Adiponectin augments insulin sensitivity and low levels of adiponectin are associated with obesity, T2DM, hypertension, and coronary artery disease [20][21][56,57]. In normal pregnancy, maternal adiponectin secretion progressively declines probably due to decreased insulin sensitivity [22][58].
Previous studies have demonstrated that low levels of adiponectin in the first trimester are associated with GDM development later in pregnancy [23][24][25][53,59,60]. A metanalysis by Iliodromiti et al. suggested that early pregnancy adiponectin levels have a moderate predictive value for GDM, similar to that of clinical risk factors [26][61]. In summary, adiponectin may play a role in the pathophysiology of GDM and has the potential for a promising predictive biomarker. Further research is needed to further establish the true value of adiponectin in GDM prediction.
4.2. Leptin
Leptin regulates energy intake, suppresses appetite, and enhances the insulin effect with both central and peripheral effects [27][62]. Leptin is also expressed by placental cells and levels increase up to three-folds in pregnancy likely due to placental secretion and an increase in fat tissue; however, its exact role in pregnancy remains unclear [28][29][63,64]. Evidence regarding the association between leptin levels and GDM is inconsistent, with some studies demonstrating higher leptin levels in women who subsequently develop GDM [30][31][50,65], whereas others showed no difference [32][33][66,67]. Future prospective studies are required to determine leptin predictive ability in GDM while adequately addressing the confounding influence of BMI and gestational weight gain on leptin levels in pregnancy.
5. Predicting GDM by Pregnancy-Related Proteins
5.1. Pregnancy Associated Plasma Protein A (PAPP-A)
PAPP-A is a metalloproteinase that increases the bioavailability of insulin-like growth factor 1 (IGF-1) by its cleavage from IGF binding protein-4 [34][68]. In pregnancy, PAPP-A is secreted by trophoblast cells and used as a first-trimester screening test for aneuploidy, as well as a predictor of placental disorders such as preeclampsia and fetal growth restriction [35][69]. It has been hypothesized that PAPP-A has a role in regulating glucose levels in pregnancy, with low levels associated with insulin resistance and GDM.
Nonetheless, previous studies have yielded conflicting results. A number of studies reported low first-trimester PAPP-A levels in women who eventually developed GDM [36][37][38][39][70,71,72,73]. Additionally, a large systematic review and meta-analysis by Donovan et al. concluded that women who are diagnosed with GDM have lower first-trimester levels of PAPP-A, even though a high degree of between-study heterogeneity was noted [40][74]. Other studies failed to demonstrate differences in PAPP-A levels in pregnancies with GDM compared to normal pregnancies [41][42][75,76] and Syngelaki et al. showed that the performance of screening for GDM by maternal factors was not improved by the addition of PAPP-A [43][77]. Future prospective studies are required to establish the clinical utility of this biomarker.
5.2. Placental Growth Factor (PLGF)
PLGF is an angiogenic protein highly expressed in the placenta [44][78]. PLGF is widely used in aneuploidy screening in the first trimester, with low levels associated with placental-mediated disorders, mainly preeclampsia and fetal growth restriction [45][79].
Several studies have shown that elevated PLGF levels in early pregnancy are associated with GDM development [46][47][80,81]. However, other studies have demonstrated no differences in PLGF levels between women who developed GDM and controls [48][49][82,83]. Additionally, a large prospective cohort study from the UK showed that even though early PLGF levels were higher in women with GDM, the addition of PLGF to a prediction model that includes maternal factors did not improve the predictive ability [43][77]. Therefore, current evidence does not support the use of PLGF as an effective biomarker for GDM.
5.3. First-Trimester Combined Test (FTCT)
The FTCT is an effective screening tool for fetal aneuploidy, which includes the combination of maternal age, ultrasound measurement of fetal nuchal translucency, and the serum markers-free β-human chorionic gonadotropin and PAPP-A. As an early, routinely implemented test, which includes pregnancy-related proteins, the FTCT has the potential to be used as a tool for the prediction of GDM. Visconti et al. showed that an FTCT result of <1:10,000 was significantly associated with GDM development later in pregnancy, but with low accuracy [50][84], and other studies failed to demonstrate this association [42][51][76,85]. Based on current evidence, it is unclear whether the use of low PAPP-A solely (in absolute levels or in multiples of the median) contributes to GDM prediction better than the entire FTCT.
6. Predicting GDM by Inflammatory Markers
6.1. Tumor Necrosis Factor-α (TNF-α)
TNF-α is an inflammatory cytokine that is produced by placental cells and has been suggested as a mediator for insulin resistance in pregnancy [52][86]. While some studies showed an association between elevated levels of TNF-α in the first trimester and GDM development later in pregnancy [53][54][87,88], others failed to demonstrate this effect [33][55][67,89]. Furthermore, adding TNF-α to a screening model did not improve the prediction of GDM over maternal clinical characteristics [56][90]. In summary, even though TNF-α probably has a role in the pathogenesis of insulin resistance and GDM, the actual predictive value of this biomarker is yet to be established.
6.2. C-Reactive Protein (CRP)
CRP is an acute-phase protein secreted and released in response to tissue injury, inflammation, and infection [57][91]. Evidence regarding the association between levels of CRP or high-sensitivity CRP and GDM is inconsistent, with multiple studies showing high first-trimester levels in women who eventually develop GDM [58][59][60][61][92,93,94,95] and some studies not [56][62][90,96]. A possible confounder is the fact that CRP levels in pregnancy correlate with BMI and a prospective study by Wolf et al. concluded that the association between increased CRP and GDM was attenuated when BMI was included in the model [63][97]; the same effect was reported by others as well [64][65][98,99]. A recent systematic review by Amirian et al. discussed conflicting evidence and concluded that more studies are needed for CRP to be used as an indicator for GDM [66][100].
6.3. Interleukin 6 (IL-6)
IL-6 is a circulating inflammatory cytokine secreted by adipocytes as well as by macrophages, endothelial cells, pancreatic cells, and placenta cells [67][101]. IL-6 is involved in the regulation of immune response regulation, inflammation, and hematopoiesis [68][102], but also has a significant role in obesity and insulin resistance [69][103]. A systematic review and meta-analysis by Wang et al. concluded that IL-6 is a strong predictor of developing T2DM [70][104].
Previous studies showed an association between high levels of IL-6 and GDM [71][72][73][105,106,107]; however, these studies were limited by the gestational age at which IL-6 levels were measured, the population assessed, and by controlling for confounders such as BMI. Other studies failed to demonstrate a difference in IL-6 levels between GDM and normal pregnancies [74][75][108,109]. Nevertheless, a study by Hassiakos et al. showed that first-trimester IL-6 levels were a significant predictor of GDM development later in pregnancy and adding IL-6 to a prediction model that included maternal characteristics yielded an improved prediction [76][110]. A systematic review by Amirian et al. concluded that IL-6 levels are significantly higher in pregnant women with GDM than in healthy pregnant women and therefore the evaluation of this marker as a GDM predictor can be investigated [77][111]. In summary, although IL-6 has the potential to be a good biomarker for GDM in the future as demonstrated in T2DM, current evidence does not support it as such. Larger prospective studies are needed to assess IL-6 function in GDM as well as to adjust for obesity as a confounder and to obtain serial IL-6 measurements for the identification of trimester-specific ranges.
7. Predicting GDM by Insulin Resistance Markers
SHBG
SHBG is a glycoprotein produced mainly by the liver, binds androgen and estrogen, and has an inverse relationship with insulin levels [78][116]. Low levels of SHBG prior to pregnancy [79][80][117,118] and in the first trimester [58][81][82][92,119,120] were found to be correlated with GDM development later in pregnancy. Nanda et al. showed that adding SHBG to a clinical risk prediction model improved its accuracy [83][121]. However, in other studies, this association was not found [84][122] or was no longer significant after adjusting for BMI, ethnicity, and family history [62][96]. Hence, even though SHBG is a very promising marker for early diagnosis of GDM, with even pre-pregnancy predictability, further studies are required to establish its role.
