Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 2 by Bruce Ren and Version 1 by Zou Xiaofeng.
Pressure ulcers (PU) are one of the most frequent hazards of long-term bedridden patients. With the continuous increase of aging, the number of long-term bedridden disabled and semi-disabled elderly people is increasing. At the same time, there is a serious shortage of professional pressure ulcer nursing staff.
- pressure ulcer prevention
- automatic repositioning
- temperature monitoring
- support airbag
- flexible turning
1. Introduction
With the growth of the aging population, the number of disabled and semi-disabled elderly people is increasing [1]. Pressure ulcers (PU) are one of the most frequent hazards for patients who are bedridden for a long time [2,3][2][3]. These people need the intervention of nurses to assist in turning over to improve the pressure distribution and achieve the purpose of PU prevention [4,5][4][5]. However, many problems are present such as the shortage of caregivers, the high average age of caregivers, and the low professional quality of caregivers. It is difficult to meet the patient’s turnover care needs.
It is generally believed that the combined effect of pressure, friction and shear force on the human body caused by elderly patients lying in bed is the main cause of PU. Urinary incontinence, excessive sweating, and hot and humid local environment are also important causes of PU. Therefore, clinically, patient repositioning is usually the main means to prevent PU in nursing settings. Turning over care for patients once every two hours is stressful not only for the nursing staff in nursing institutions and hospitals, but also for the nursing staff at home [6].
There is a serious shortage of nursing professionals all over the world. According to the Federation of Nurses and Health Care Professionals, there are more than 20,000 elderly care workers in China, but the demand is about 10 million, and the gap is huge. Coupled with the high rate of nursing staff, long shifts, back and shoulder injuries and other groups of poor health conditions, hospitals and elderly care institutions are facing increasing pressure in attracting and retaining nursing staff [7,8][7][8]. According to the survey results, the age of some nursing staff in some elderly care institutions is generally over 65, and the level of cultural literacy is generally low. The elderly and infirm are unable to meet the mental and physical needs of nursing, and cannot perform scientific nursing work in daily nursing care. For elderly patients with PU, there are phenomena such as irregular operation, and there is a risk of secondary injury to vulnerable elderly patients [9].
The products on the market for pressure ulcer prevention are mainly anti-decubitus mattresses [10], which disperse the pressure of the patient when lying in bed by using static latex, and other material mattresses or dynamic pneumatic mattresses to achieve a certain pressure ulcer prevention [11,12][11][12]. Related research designed to use pressure sensors, temperature and humidity sensors to monitor the local state of the patient’s body in bed, and then feedback control is performed by multiple independent execution units to improve the pressure distribution of the human body [13,14][13][14]. Among them, the “Taiatsu Bunsan” mattress developed by Japanese institutions is representative. The mattress is composed of 108 independent stacked airbags. The self-made rubber pressure sensor is used to perform real-time pressure detection on bedridden patients. The surface of the mattress will be based on the patient’s body posture and pressure distribution automatically adjust the air pressure of the corresponding position of the airbags to maintain a relatively even distribution of body pressure [15].
In addition, Yousefi et al. [16] adopted a mechanical-pneumatic hybrid method to develop a new type of mattress for PU prevention, which can realize the function of turning on the basis of monitoring pressure. However, the above-mentioned smart mattresses often have insurmountable defects, such as complex structures and cost constraints, which are difficult to use widely. In daily nursing care, the turning-over method is the main manual intervention method for PU prevention. It must be matched with a suitable decompression support mattress to achieve a good pressure ulcer prevention effect.
According to the international “Pressure Ulcer Prevention and Treatment: Clinical Practice Guidelines”, the key prevention strategies of pressure ulcer include risk assessment, the use of support surfaces, regular posture adjustment, skin care and nutritional care. Pressure ulcer prevention products at home and abroad mainly focus on the purpose of “sharing body pressure on support surface”, including static flexible support material, pneumatic alternating pressure relief mattresses, etc. [17]. Some studies expect to replace or partially replace manual intervention by equipment for turning over operation, but the equipment often has insurmountable defects, which makes it difficult to apply them in a short time. Pressure ulcer is the most likely to occur on the back, elbows, ankles, heels, hips, buttocks, shoulders and head [4]. In daily care, two hours-per-time-turnover-operation is the main manual intervention method for pressure ulcer prevention, and it should be combined with a suitable decompression support mattress to achieve a good pressure ulcer prevention effect. Regular turning over is still the main method to prevent PU [18,19][18][19].
In recent years, with the development of technologies in computers and Internet of Things, sensor technology has been rationally applied in the field of PU prevention, and the equipment shows a trend of intelligent development [20]. In addition, research on the real-time monitoring of the pressure and various physiological parameters of bedridden patients is underway [21]. With the continuous deepening of the application of digitalization in medical care, PU prevention can be used as an independent functional module of the digital cloud platform [22]. Real-time monitoring of patient signs and intelligent equipment instead of nursing staff to perform nursing operations such as turning over, this is the future of pressure ulcer prevention of smart medical care [23,24,25][23][24][25]. Since the COVID-19 epidemic spread, temperature measurement is one of the effective means of epidemic prevention. Based on actual needs, we propose that the temperature sensor is applied to the turning mattress to monitor the condition of bedridden patients. As shown in Figure 1, we developed a flexible turning and sensing system for pressure ulcer prevention, which is mainly composed of turning mattresses and monitoring equipment. The mattress is driven by a flexible material to turn over, and a reasonable turning method is designed to prevent pressure sores and increase the safety and comfort of the process. We applied the non-contact temperature sensor based on infrared reflection principle to the mattress, and measured the bed temperature of the elderly by measuring the forehead temperature. For this reason, we designed a calibration method to improve the accuracy of the sensor. Through real-time temperature monitoring, body temperature detection, monitoring of getting out of bed, and status monitoring of the process of turning over are realized.

Figure 1. Human body turnover process monitoring and controlling system.
2. Mattress Turnover Test
The experimenter imitated the disabled elderly lying on a mattress. First, the support airbags were inflated with a constant maximum power. After about 50 s, the support surface reached a predetermined angle. Then turning airbags started to inflate with a constant maximum power, and the support airbags began to deflate with dynamic changes. After about 150 s, the supporting surface and the turning surface reached a predetermined angle, as is shown in Figure 2. The value of the entire pressure sensor is much smaller than the maximum pressure resistance of the airbags, so the subsequent work does not monitor the air pressure. According to the feedback of the experimenter, the comfort of the pneumatic turnover mattress is better than that of the conventional one-side turnover bed.
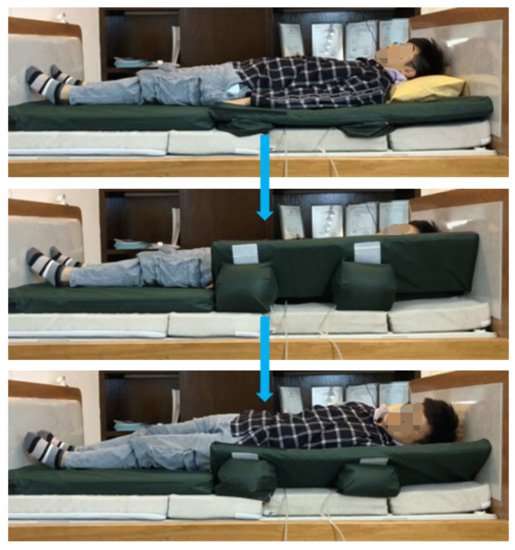
Figure 2. Three steps in the process of turnover.
3. Temperature Sensor Monitors the State of Bed Rest
3.1. Real-Time Forehead Temperature Measurement
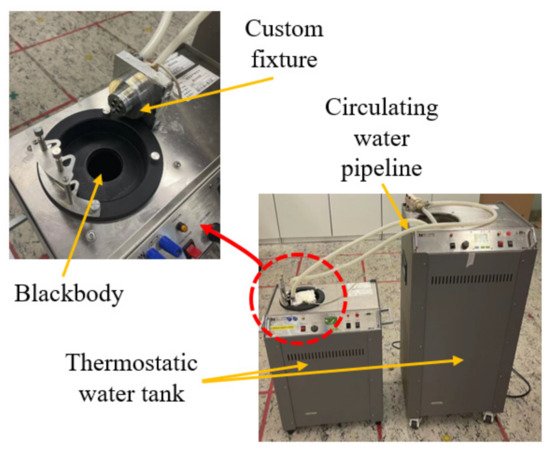
The sensor we use uses a Negative Temperature Coefficient (NTC) thermistor as ambient temperature compensation. When the patient is not turning over, take the temperature of the patient’s forehead. Ambient temperature is an important factor in infrared temperature measurement. The output voltage of the thermopile is different under different ambient temperatures. In this scenario, the accuracy requirements are high. Therefore, we calibrate the temperature sensor. The calibration of the sensor needs to provide two conditions: one is to provide an accurate ambient temperature for the sensor; the other is to provide a standard target temperature.
We have customized a set of fixtures and assembled the sensor on the fixtures. The fixtures are filled with circulating water at a set temperature, which is controlled by a thermostatic water tank. The advantage of this is that the temperature control is accurate and is not affected by the environment in which the experimental equipment is located. Another thermostatic water tank equipped with a standard blackbody provides the target temperature. The blackbody penetrates in the water tank, and the temperature of the blackbody can be adjusted by controlling the temperature of the water tank. We aligned the fixture with the sensor to the black body and measured and recorded the value of the temperature sensor. The calibration equipment is shown in Figure 3.
Figure 3. Temperature sensor calibration tool diagram.
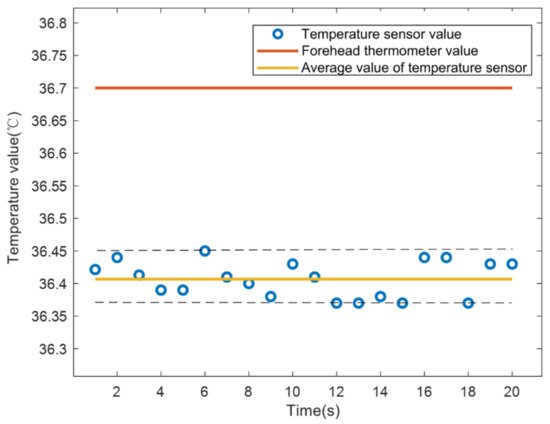
In order to improve the measurement accuracy, the measured value and the true value of the thermopile output voltage and the ambient temperature were obtained through the calibration experiment, and then the segmented interpolation was used for temperature compensation to obtain a relatively accurate measurement value. The larger value measured by the two sensors is the final measured temperature.
As shown in Figure 3, at a room temperature of about 28 °C, the sensor was used to record the temperature data of the experimenter once per second for 20 s. The temperature measured by the medical forehead gun is 36.7 °C, the average temperature measured by the sensor is 36.41 °C, and the temperature difference is about 0.3 °C, which has clinical significance.
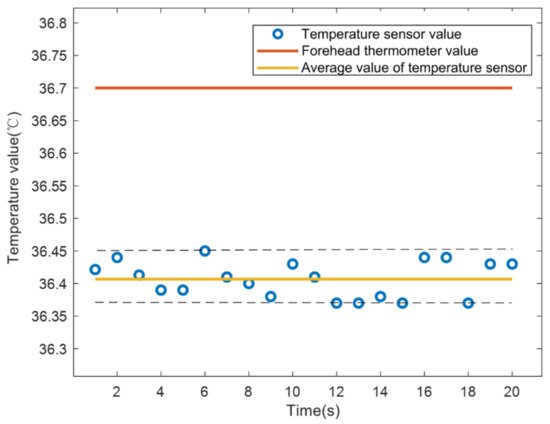
Figure 3. Comparison of temperature measurement between infrared temperature sensor and medical forehead thermometer.
3.2. Out-of-Bed Monitoring and Position Monitoring
Turning over this mattress is the core function. The airbag drives the mattress to tilt the patient’s body by about 30–45°, and the bedridden patient can automatically complete the turning over without the cooperation of the nurse, so as to improve the compression area of the body to prevent PU. This requires that the patient must lie in a prescribed position. The temperature sensor is now used for threshold monitoring to identify the position of the patient on the bed.
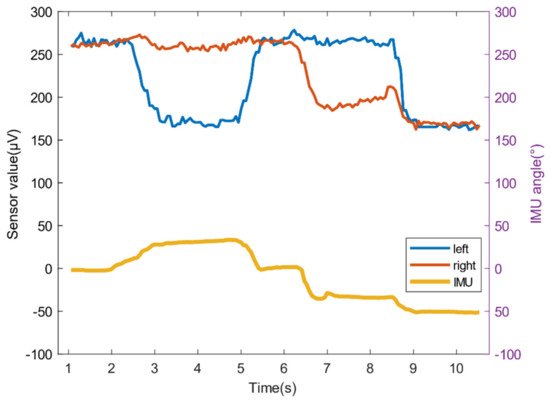
We use an inertial measurement unit (IMU) to measure the head swing angle, and at the same time use the left and right sensors to record changes in forehead temperature. As shown in Figure 4, the head is in the middle position from 0 to 2 s, and both sensors can collect facial temperature data, the value is above 250 μV; 3 to 5 s, the head is offset to the right by about 30°, and the measurement area of the left sensor is Mattress pillow, the value is about 175 μV; 5 to 7 s, the head returns to the center position; 7 to 9 s, the head is about 30° to the left, at this time the right sensor measuring area is the pillow, the value is about 180 μV; 9 to 11 s, the head is left Offset 50°, at this time the face is completely out of the measurement range, the value is about 170 μV.
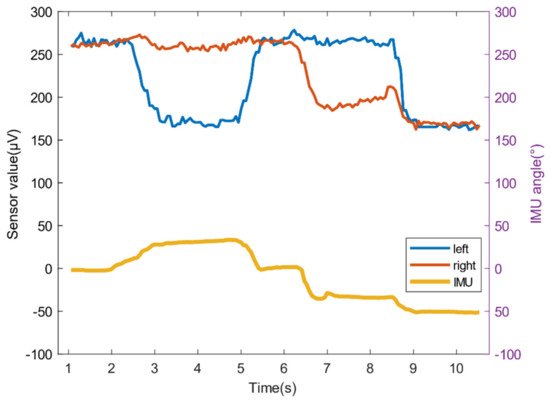
Figure 4. The relationship between the head swing angle and the sensor value change.
When the values of the left and right sensors are less than the threshold value for more than a certain period of time, the elderly may be in an improper position or even get out of bed, and an alarm will be activated; when the voltage value is greater than or equal to the threshold value, it shows that the elderly position is normal and can be turned over through mattress.
3.3. Real-Time Monitoring of the Turning Process
Turning over is the process of placing the patient’s body at an angle, which is unpredictable. The infrared temperature sensor monitors the change of the thermopile output voltage value during the patient’s turning over to realize the monitoring of the whole process. When the monitoring value is abnormal, the system will immediately stop turning and give an alarm.
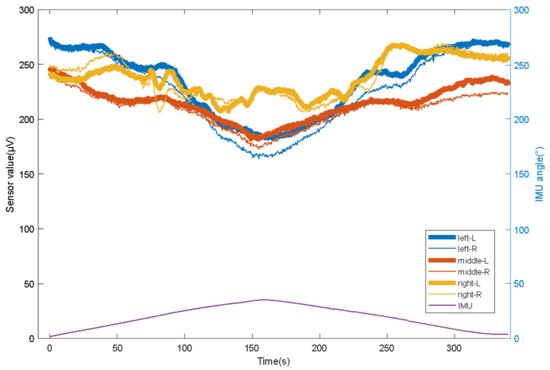
In the experiment, we asked the experimenter to lie in the middle, left, and right of the mattress (the offset distance is 8 cm), and use the left and right sensors above the forehead to measure the temperature data during the entire turning-flattening process, and an IMU was used to record the changes in the inclination angle of the experimenter’s body during the turnover process in real time.
As shown in Figure 4, the temperature value and angle value trend can be captured by the sensor value changes at the three state nodes of the beginning and end to ensure that the experimenter completes the entire turn over care process through the mattress.
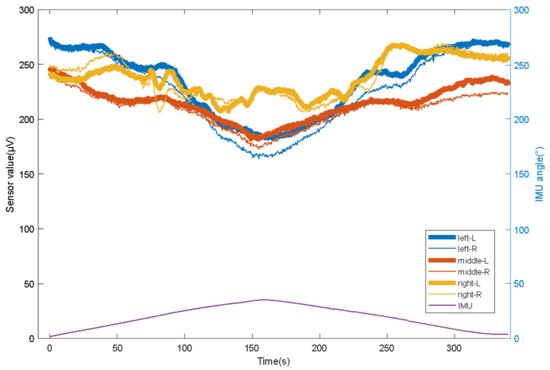
Figure 4. The relationship between the head swing angle and the sensor value change.
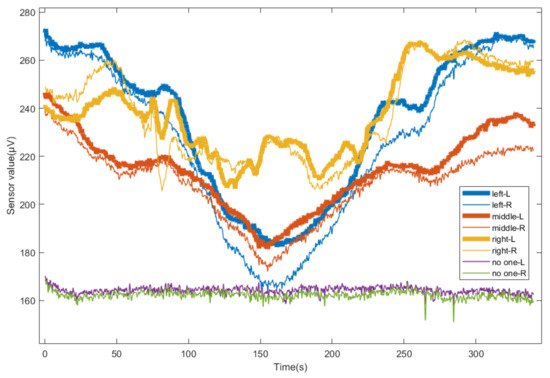
Figure 5 shows the detection values of the whole process of the left turning over of the mattress when the experimenter lies in the middle, left and right of the mattress, and when there was no one on the bed. When the experimenter lies in the middle position, with the increase of the left turning angle of the mattress, the right sensor loses the human body temperature. At this time, its value is close to that when there is no one, and the value of the left sensor is always more than 20% higher than that when there is no one. When the experimenter lies in the left leaning position, with the increase of the left inclination angle of the mattress, there is a loss of human body temperature on the right side. At this time, its value is close to that when there is no one, and the value of the left sensor is always more than 10% higher than that when there is no one. When the experimenter lies in the right deviation position, the left and right sensor values are always more than 20% higher than when there are no patients. Therefore, the temperature sensor can clearly distinguish whether there are people in the measurement area, which can alarm in time when the patient falls into bed and other accidents.
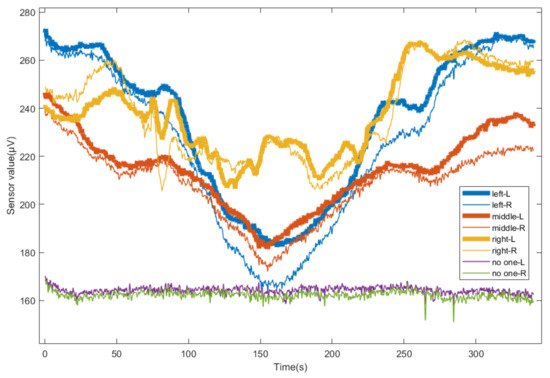
Figure 5. Change of sensor value during turning down in different positions.
References
- Gaspar, S.; Peralta, M.; Marques, A.; Budri, A.; De Matos, M.G. Effectiveness on hospital-acquired pressure ulcers prevention: A systematic review. Int. Wound J. 2019, 16, 1087–1102.
- Serraes, B.; Van Leen, M.; Schols, J.; Van Hecke, A.; Verhaeghe, S.; Beeckman, D. Prevention of pressure ulcers with a static air support surface: A systematic review. Int. Wound J. 2018, 15, 333–343.
- Li, T.; Wang, L.; Yi, J.A.F.T.; Li, Q.; Liu, T. Reconstructing Walking Dynamics from Two Shank-Mounted Inertial Measurement Units (IMUs). IEEE/ASME Trans. Mechatron. 2021, 1.
- Zhong, Z.; Chen, F.; Zhai, Q.; Fu, Z.; Ferreira, J.; Liu, Y.; Yi, J.; Liu, T. A real-time pre-impact fall detection and protection system. In Proceedings of the 2018 IEEE/ASME International Conference on Advanced Intelligent Mechatronics (AIM), Auckland, New Zealand, 9–12 June 2018; pp. 1039–1044.
- Nageswaran, S.; Vijayakumar, R.; Sivarasu, S. Design of mechanical interface to re-distribute excess pressure to prevent the formation of decubitus ulcers in bed ridden patients. In Proceedings of the 2015 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Milan, Italy, 25–29 August 2015; pp. 1021–1024.
- Demarré, L.; Van Lancker, A.; Van Hecke, A.; Verhaeghe, S.; Grypdonck, M.; Lemey, J.; Annemans, L.; Beeckman, D. The cost of prevention and treatment of pressure ulcers: A systematic review. Int. J. Nurs. Stud. 2015, 52, 1754–1774.
- Nair, P.; Mathur, S.; Bhandare, R.; Narayanan, G. Bed sore Prevention using Pneumatic controls. In Proceedings of the 2020 IEEE International Conference on Electronics, Computing and Communication Technologies (CONECCT), Bangalore, India, 2–4 July 2020; pp. 1–5.
- Guo, S.; Kato, Y.; Ito, H.; Mukai, T. Development of rubber-based flexible sensor sheet for care-related apparatus. SEI Tech. Rev. 2012, 75, 125–131.
- Meaume, S.; Marty, M. Pressure ulcer prevention using an alternating-pressure mattress overlay: The MATCARP project. J. Wound Care 2020, 29 (Suppl. 9a), S32–S38.
- Misaki, A.; Imanishi, K.; Takasugi, S.I.; Wada, M.; Fukagawa, S.; Furue, M. Body pressure sensing mattress for bedsore prevention. SEI Tech. Rev. 2014, 79, 95–99.
- Aleksandrowicz, H.; Owczarczyk-Saczonek, A.; Placek, W. Venous Leg Ulcers: Advanced Therapies and New Technologies. Biomedicines 2021, 9, 1569.
- Tayyib, N.; Coyer, F. Effectiveness of pressure ulcer prevention strategies for adult patients in intensive care units: A systematic review. Worldviews Evid.-Based Nurs. 2016, 13, 432–444.
- Bergstrom, N. Treatment of Pressure Ulcers: Clinical Practice Guideline; DIANE Publishing: Collingdale, PA, USA, 2004.
- Carter, M.J. Economic Evaluations of Guideline-Based or Strategic Interventions for the Prevention or Treatment of Chronic Wounds. Appl. Health Econ. Health Policy 2014, 12, 373–389.
- Hayakawa, T.; Misaki, A.; Takasugi, S.I.; Furue, M. Smart Rubber Active Mattress” Taiatsu Bunsan. SEI Tech. Rev. 2017, 85, 65–67.
- Yousefi, R.; Ostadabbas, S.; Faezipour, M.; Nourani, M.; Ng, V.; Tamil, L.S.; Bowling, A.; Behan, D.; Pompeo, M. A smart bed platform for monitoring & ulcer prevention. In Proceedings of the 2011 4th International Conference on Biomedical Engineering and Informatics (BMEI), Shanghai, China, 15–17 October 2011; pp. 1362–1366.
- Ricci, E.; Roberto, C.; Ippolito, A.; Bianco, A.; Scalise, M.T. A new pressure-relieving mattress overlay. EWMA J. 2013, 13, 1.
- Defloor, T.; De Bacquer, D.; Grypdonck, M.H. The effect of various combinations of turning and pressure reducing devices on the incidence of pressure ulcers. Int. J. Nurs. Stud. 2005, 42, 37–46.
- Sikka, M.P.; Garg, S. Functional textiles for prevention of pressure ulcers—A review. Res. J. Text. Appar. 2020, 24, 185–198.
- Mansfield, S.; Obraczka, K.; Roy, S. Pressure Injury Prevention: A Survey. IEEE Rev. Biomed. Eng. 2019, 13, 352–368.
- Tannen, A.; Dassen, T.; Halfens, R. Differences in prevalence of pressure ulcers between the Netherlands and Germany—Associations between risk, prevention and occurrence of pressure ulcers in hospitals and nursing homes. J. Clin. Nurs. 2008, 17, 9.
- McInnes, E.; National Institite for Clinical Excellence. The use of pressure-relieving devices (beds, mattresses and overlays) for the prevention of pressure ulcers in primary and secondary care. J. Tissue Viability 2004, 14, 4–6.
- Pan, P.; Haesler, E. Prevention and Treatment of Pressure Ulcers: Clinical Practice Guideline; Cambridge Media: Hong Kong, China, 2014.
- Padula, W.V.; Mishra, M.K.; Makic, M.B.F.; Sullivan, P.W. Improving the Quality of Pressure Ulcer Care with Prevention: A Cost-Effectiveness Analysis. Med. Care 2011, 49, 385.
- Simon, J.P.; Patricia, W.S. A systematic review of economic evaluations assessing interventions aimed at preventing or treating pressure ulcers. Int. J. Nurs. Stud. 2015, 52, 769–788.
More
