Spray congealing is an emerging technology for the production of solid dispersion to enhance the bioavailability of poorly soluble drugs by using low-melting hydrophilic excipients. Since the '90s, spray congealing technology has been used to obtain microparticles (MPs) for controlled release, taste masking and stability enhancement of APIs. The main advantages are the absence of solvents and the possibility to obtain free-flowing MPs by a relatively inexpensive, simple and one step process. This entry focused on the application of spary congealing as an amerging technology for the production of solid dispersions to enhance the bioavailability of poorly water soluble drugs by using low-melting hydrophilic excipients.
- spray chilling
- spray cooling
- microparticles
- solubility enhancement
- dissolution rate
- polyethylene glycol
1. Introduction
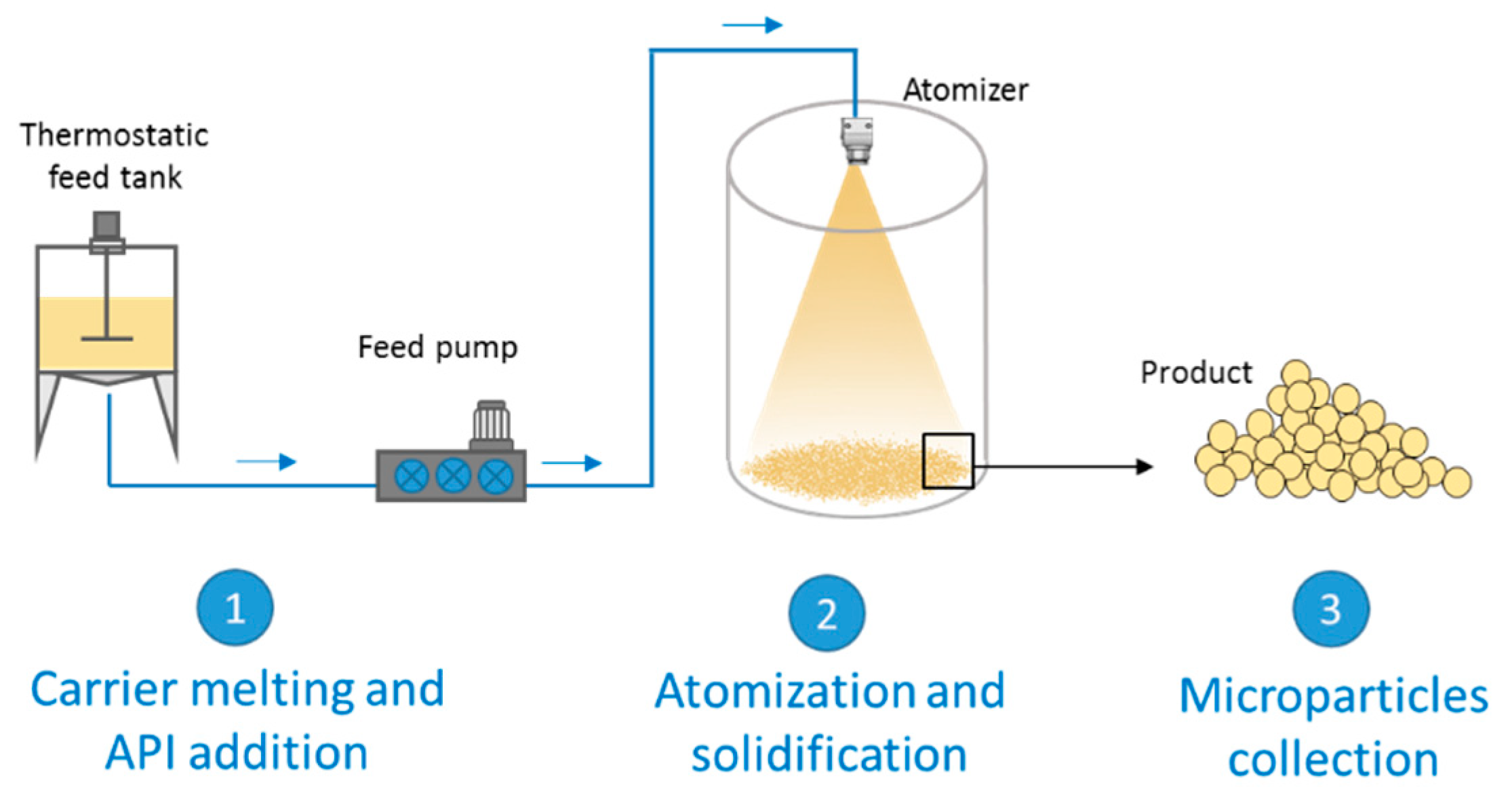
2. Spray Congealing Technology: General Aspects
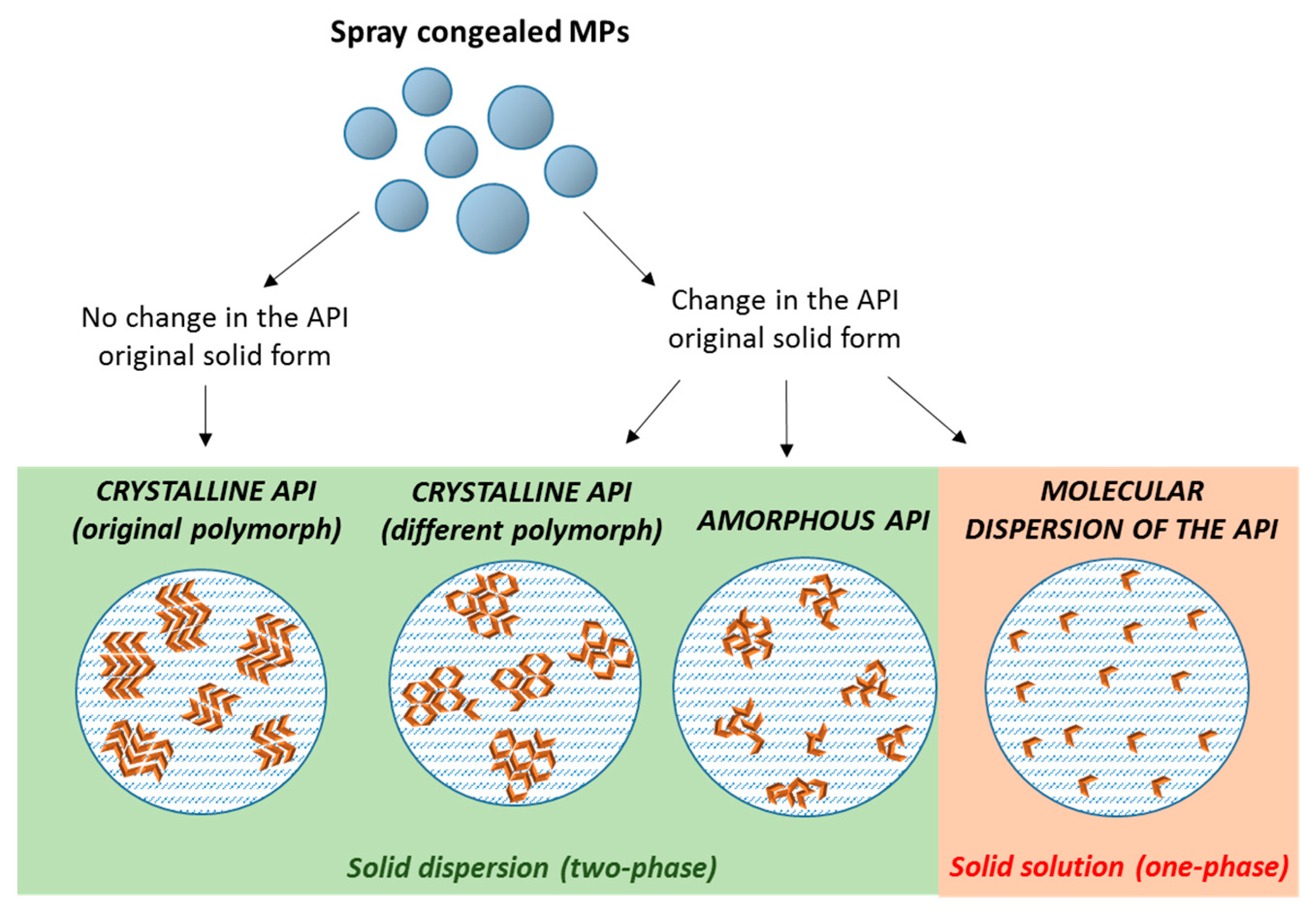
3. Structure and Composition of Spray Congealed SD
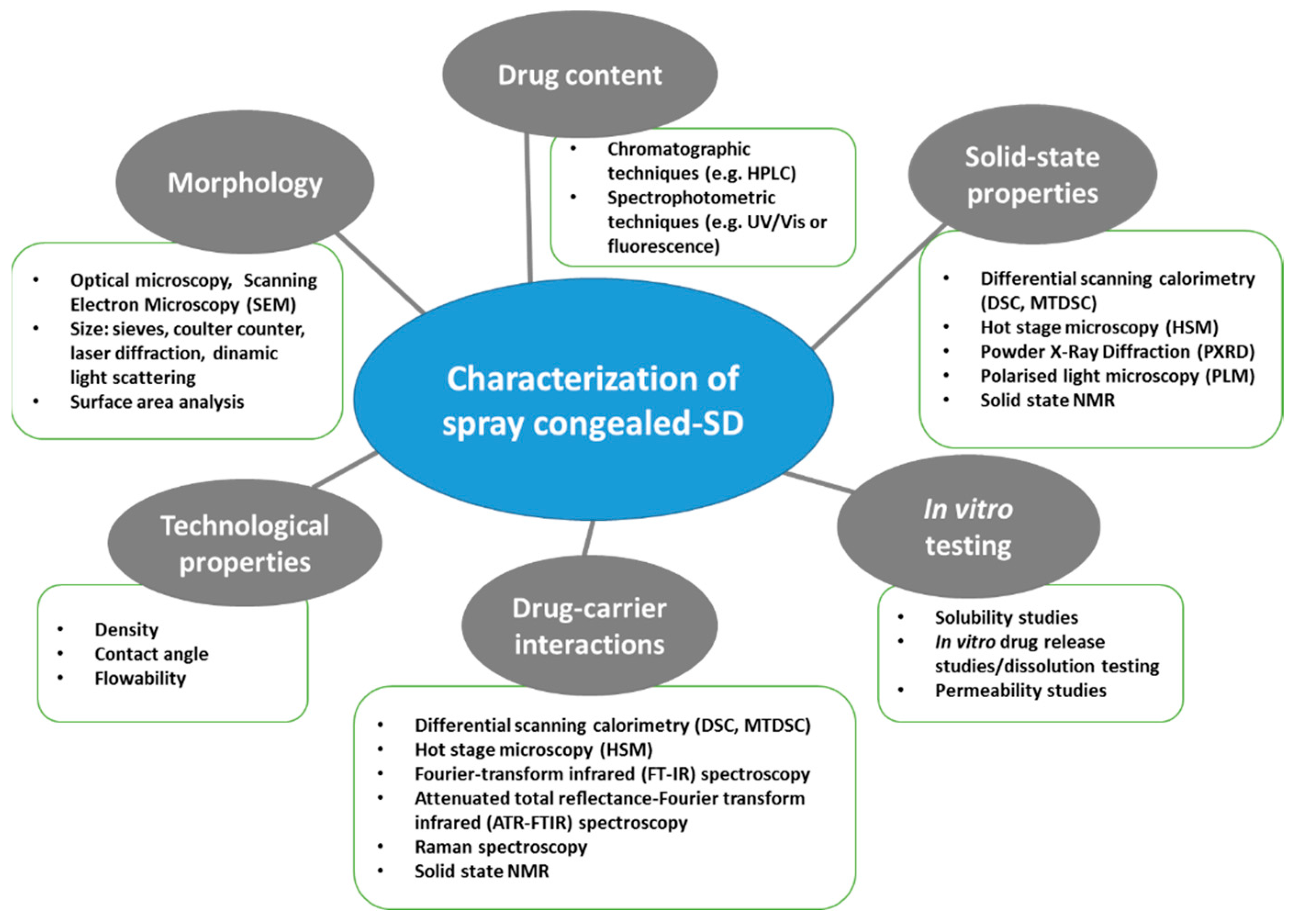
4. Properties and Characterization of Spray Congealed SD
5. Mechanisms of Bioavailability Enhancement of Spray Congealed Systems
-
MPs containing the drug used as received
-
MPs containing pre-activated drug
|
Drug |
Carrier + Additives |
Type of SD |
Achievement |
Ref. |
|---|---|---|---|---|
|
Carbamazepine |
Gelucire® 50/13 |
Crystalline drug (original polymorph) |
Increased in vitro dissolution rate |
|
|
Carbamazepine |
Gelucire® 50/13 |
Crystalline drug (change from β to α) |
Increased in vitro dissolution rate |
|
|
Piroxicam |
Gelucire® 50/13 |
Crystalline drug (original polymorph) |
Increased in vitro dissolution rate |
|
|
Praziquantel |
Gelucire® 50/13 |
Crystalline drug (original polymorph) |
Increased in vitro dissolution rate |
|
|
Olanzapine |
Gelucire® 50/13, Lutrol F68 or Lutrol F127 |
Reduced-sized drug particles |
Increased in vitro dissolution rate |
|
|
Acetazolamide |
Poloxamer-237 |
Conversion to amorphous form/ dispersion on molecular level |
Increased in vitro dissolution rate and 9-fold solubility enhancement |
|
|
Glibenclamide |
Myverol, Myvatex, Gelucire® 50/13, Gelucire® 44/14, Poloxamer 188 and PEG 4000 |
Crystalline drug |
Five-fold increased drug solubilization (Gelucire 50/13 + PEG 4000) |
|
|
Metronidazole |
PEG 3350 + HPMC, Dicalcium phosphate, Magnesium stearate, Methylcellulose, Polyvinylpyrrolidone, Silicon dioxide, Sodium oleate/Citric acid |
Marked reduction in drug crystallinity |
Slightly increased in vitro dissolution rate with only carrier (different results depending on the type and amount of additive) |
|
|
Rifampicin |
PEG 3350 + HPMC (different grades) |
No information provided |
Increased in vitro dissolution rate, with intensity depending on the HPMC grade. |
|
|
Glimepiride |
Gelucire® 50/13, poloxamer 188, and PEG 6000 |
Crystalline drug (original polymorph) |
Increased in vitro dissolution rate (Gelucire the highest increase). 10-fold (Gelucire) and 5-fold (poloxamer, PEG) solubility enhancement |
[19] |
|
Diclofenac |
Gelucire® 50/13 |
Marked reduction in drug crystallinity |
Increase in the in vitro dissolution rate |
|
|
Indomethacin |
Gelucire® 50/13, Gelucire® 48/16 |
Conversion to amorphous form/dispersion on molecular level |
Increase in the in vitro dissolution rate and solubility Increased oral bioavailability in rats |
|
|
Bufadienolides (bufalin, cinobufagin, and resibufogenin) |
Lutrol F127 |
Formation of molecular dispersions |
Four-fold increase in vitro dissolution rate |
|
|
Wild garlic extract |
Gelucire® 50/13 |
No information provided |
Increase in the in vitro dissolution rate |
References
- Chella, N.; Tadikonda, R. Melt dispersion granules: Formulation and evaluation to improve oral delivery of poorly soluble drugs—A case study with valsartan. Drug Dev. Ind. Pharm. 2015, 41, 888–897.
- Morishita, M.; Peppas, N.A. Advances in oral drug delivery: Improved bioavailability of poorly absorbed drugs by tissue and cellular optimization. Adv. Drug Deliv. Rev. 2012, 64, 479.
- Kawabata, Y.; Wada, K.; Nakatani, M.; Yamada, S.; Onoue, S. Formulation design for poorly water-soluble drugs based on biopharmaceutics classification system: Basic approaches and practical applications. Int. J. Pharm. 2011, 420, 1–10.
- Lipinski, C.A. Drug-like properties and the causes of poor solubility and poor permeability. J. Pharmacol. Toxicol. Methods 2000, 44, 235–249.
- FDA. Guidance for Industry, Waiver of In Vivo Bioavailability and Bioequivalence Studies for Immediate-Release Solid Oral Dosage Forms based on a Biopharmaceutics Classification System; FDA: Silver Spring, MD, USA, 2000.
- Baghel, S.; Cathcart, H.; O’Reilly, N.J. Polymeric Amorphous Solid Dispersions: A Review of Amorphization, Crystallization, Stabilization, Solid-State Characterization, and Aqueous Solubilization of Biopharmaceutical Classification System Class II Drugs. J. Pharm. Sci. 2016, 105, 2527–2544.
- Serajuddin, A.T.M. Solid dispersion of poorly water-soluble drugs: Early promises, subsequent problems, and recent breakthroughs. J. Pharm. Sci. 1999, 88, 1058–1066.
- Mishra, D.K.; Dhote, V.; Bhargava, A.; Jain, D.K.; Mishra, P.K. Amorphous solid dispersion technique for improved drug delivery: Basics to clinical applications. Drug Deliv. Transl. Res. 2015, 5, 552–565.
- Ellenberger, D.J.; Miller, D.A.; Williamsiii, R.O. Expanding the Application and Formulation Space of Amorphous Solid Dispersions with KinetiSol®: A Review. AAPS PharmSciTech 2018, 19, 1933–1956.
- Dedroog, S.; Huygens, C.; Van Den Mooter, G. Chemically identical but physically different: A comparison of spray drying, hot melt extrusion and cryo-milling for the formulation of high drug loaded amorphous solid dispersions of naproxen. Eur. J. Pharm. Biopharm. 2019, 135, 1–12.
- Zanolla, D.; Perissutti, B.; Passerini, N.; Invernizzi, S.; Voinovich, D.; Bertoni, S.; Melegari, C.; Millotti, G.; Albertini, B. Milling and comilling Praziquantel at cryogenic and room temperatures: Assessment of the process-induced effects on drug properties. J. Pharm. Biomed. Anal. 2018, 153, 82–89.
- Davis, M.; Walker, G. Recent strategies in spray drying for the enhanced bioavailability of poorly water-soluble drugs. J. Control. Release 2018, 269, 110–127.
- Patil, H.; Tiwari, R.V.; Repka, M.A. Hot-Melt Extrusion: From Theory to Application in Pharmaceutical Formulation. AAPS PharmSciTech 2016, 17, 20–42.
- Cordeiro, P.; Temtem, M.; Winters, C. Spray Congealing: Applications in the Pharmaceutical Industry. Chem. Today 2013, 31, 69–72.
- Bertoni, S.; Dolci, L.S.; Albertini, B.; Passerini, N. Spray congealing: A versatile technology for advanced drug delivery systems. Ther. Deliv. 2018, 9, 833–845.
- Oh, C.M.; Guo, Q.; Heng, P.W.S.; Chan, L.W. Spray-congealed microparticles for drug delivery—An overview of factors influencing their production and characteristics. Expert Opin. Drug Deliv. 2014, 11, 1047–1060.
- Kumar, S.; Jeet, K.; Ashish, B. Recent technological advancements in multiparticulate formulations: The smart drug delivery systems. Asian J. Pharm. 2018, 9, S13–S25.
- Van Duong, T.; Van den Mooter, G. The role of the carrier in the formulation of pharmaceutical solid dispersions. Part I: Crystalline and semi-crystalline carriers. Expert Opin. Drug Deliv. 2016, 13, 1583–1594.
- Ilić, I.; Dreu, R.; Burjak, M.; Homar, M.; Kerč, J.; Srčič, S. Microparticle size control and glimepiride microencapsulation using spray congealing technology. Int. J. Pharm. 2009, 381, 176–183.
- Zhu, Q.; Taylor, L.S.; Harris, M.T. Evaluation of the Microstructure of Semicrystalline Solid Dispersions. Mol. Pharm. 2010, 7, 1291–1300.
- Chiou, W.L.; Riegelman, S. Pharmaceutical Applications of Solid Dispersion Systems. J. Pharm. Sci. 1971, 60, 1281–1302.
- Bley, H.; Fussnegger, B.; Bodmeier, R. Characterization and stability of solid dispersions based on PEG/polymer blends. Int. J. Pharm. 2010, 390, 165–173.
- Faucher, J.A.; Koleske, J.V.; Santee, E.R.; Stratta, J.J.; Wilson, C.W. Glass Transitions of Ethylene Oxide Polymers. J. Appl. Phys. 1966, 37, 3962–3964.
- Yang, M.; Gogos, C. Crystallization of poly(ethylene oxide) with acetaminophen—A study on solubility, spherulitic growth, and morphology. Eur. J. Pharm. Biopharm. 2013, 85, 889–897.
- Elander, M.; Boll, J.B.; Hojman, A.S.; Rasmussen, A.D. Gelucire and Gelucire-PEG400 formulations; tolerability in species used for non-clinical safety testing after oral (gavage) dosing. J. Appl. Toxicol. 2016, 36, 1430–1436.
- Kawakami, K.; Miyoshi, K.; Ida, Y. Solubilization behavior of poorly soluble drugs with combined use of Gelucire 44/14 and cosolvent. J. Pharm. Sci. 2004, 93, 1471–1479.
- El Hadri, M.; Achahbar, A.; El Khamkhami, J.; Khelifa, B.; Faivre, V.; Abbas, O.; Bresson, S. Lyotropic behavior of Gelucire 50/13 by XRD, Raman and IR spectroscopies according to hydration. Chem. Phys. Lipids 2016, 200, 11–23.
- Dumortier, G.; Grossiord, J.L.; Agnely, F.; Chaumeil, J.C. A Review of Poloxamer 407 Pharmaceutical and Pharmacological Characteristics. Pharm. Res. 2006, 23, 2709–2728.
- Giuliano, E.; Paolino, D.; Fresta, M.; Cosco, D. Mucosal Applications of Poloxamer 407-Based Hydrogels: An Overview. Pharmaceutics 2018, 10, e159.
- Albertini, B.; Passerini, N.; Di Sabatino, M.; Monti, D.; Burgalassi, S.; Chetoni, P.; Rodriguez, L. Poloxamer 407 microspheres for orotransmucosal drug delivery. Part I: Formulation, manufacturing and characterization. Int. J. Pharm. 2010, 399, 71–79.
- Monti, D.; Burgalassi, S.; Rossato, M.S.; Albertini, B.; Passerini, N.; Rodriguez, L.; Chetoni, P. Poloxamer 407 microspheres for orotransmucosal drug delivery. Part II: In vitro/in vivo evaluation. Int. J. Pharm. 2010, 400, 32–36.
- Passerini, N.; Perissutti, B.; Moneghini, M.; Voinovich, D.; Albertini, B.; Cavallari, C.; Rodriguez, L. Characterization of Carbamazepine-Gelucire 50/13 Microparticles Prepared by a Spray-Congealing Process Using Ultrasounds. 2002, 91, 699–707. J. pharm. Sci. 2002, 91, 699–707.
- Martins, R.M.; Siqueira, S.; Machado, M.O.; Freitas, L.A.P. The effect of homogenization method on the properties of carbamazepine microparticles prepared by spray congealing. J. Microencapsul. 2013, 30, 692–700.
- Qi, S.; Marchaud, D.; Craig, D.Q. An Investigation into the mechanism of dissolution rate enhancement of poorly water-soluble drugs from spray chilled Gelucire 50/13 microspheres. J. Pharm. Sci. 2010, 99, 262–274.
- Passerini, N.; Albertini, B.; Perissutti, B.; Rodriguez, L. Evaluation of melt granulation and ultrasonic spray congealing as techniques to enhance the dissolution of praziquantel. Int. J. Pharm. 2006, 318, 92–102.
- Cavallari, C.; Gonzalez-Rodriguez, M.; Tarterini, F.; Fini, A. Image analysis of lutrol/gelucire/olanzapine microspheres prepared by ultrasound-assisted spray congealing. Eur. J. Pharm. Biopharm. 2014, 88, 909–918.
- Kulthe, V.V.; Chaudhari, P.D. Effectiveness of Spray Congealing to Obtain Physically Stabilized Amorphous Dispersions of a Poorly Soluble Thermosensitive API. AAPS PharmSciTech 2014, 15, 1370–1377.
- Albertini, B.; Di Sabatino, M.; Melegari, C.; Passerini, N. Formulation of spray congealed microparticles with self-emulsifying ability for enhanced glibenclamide dissolution performance. J. Microencapsul. 2015, 32, 181–192.
- Oh, C.M.; Wan, P.; Heng, S.; Chan, L.W. Influence of Hydroxypropyl Methylcellulose on Metronidazole Crystallinity in Spray-Congealed Polyethylene Glycol Microparticles and Its Impact with Various Additives on Metronidazole Release. AAPS PharmSciTech 2015, 16, 1357–1367.
- Oh, C.M.; Ru Shan Siow, C.; Heng, P.V.; Chan, L.W. Impact of HPMC on the physical properties of spray-congealed PEG microparticles and its swelling effect on rifampicin dissolution. Drug Dev. Ind. Pharm. 2016, 42, 403–411.
- Cavallari, C.; Rodriguez, L.; Albertini, B.; Passerini, N.; Rosetti, F.; Fini, A. Thermal and Fractal Analysis of Diclofenac/Gelucire 50/13 Microparticles Obtained by Ultrasound-Assisted Atomization. J. Pharm. Sci. 2005, 94, 1124–1134.
- Bertoni, S.; Albertini, B.; Ferraro, L.; Beggiato, S.; Dalpiaz, A.; Passerini, N. Exploring the use of spray congealing to produce solid dispersions with enhanced indomethacin bioavailability: In vitro characterization and in vivo study. Eur. J. Pharm. Biopharm. 2019, 139, 132–141.
- Zuo, W.; Li, N.; Zhao, Y.; Fu, T.; Fei, W.; Yu, R. Synchronized release of bufadienolides in a stable Lutrol F127 based solid dispersion prepared with spray congealing dispersion prepared with spray congealing. Drug Dev. Ind. Pharm. 2018, 44, 1817–1825.
- Tomšik, A.; Šarić, L.; Bertoni, S.; Protti, M.; Albertini, B.; Mercolini, L.; Passerini, N. Encapsulations of wild garlic (Allium ursinum L.) extract using spray congealing technology. Food Res. Int. 2018, 119, 941–950.
