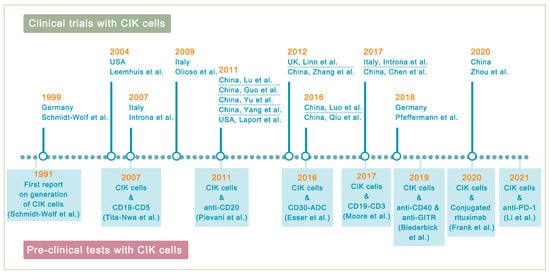
Lymphoma is a heterogeneous group of neoplasms including over 70 different subtypes. Its biological characteristic of deriving from lymphoid tissues makes it ideal for immunotherapy. Cytokine-induced killer (CIK) cells therapy is one of the adoptive immunotherapy which eliminates cancer cells by transfusing immune cells that have been expanded and activated in vitro. CIK cells are heterogeneous in nature and composed of CD3+CD56- (T cells), CD3-CD56+ (NK cells), and CD3+CD56+ (NKT cells) cell populations. The CD3+CD56+ subset is considered as the major effector cells that exert potent anti-tumor cytotoxicity in a major histocompatibility complex (MHC)-unrestricted manner. From 1991 to 2020, there are nearly 20 clinical trials conducted for the treatment of lymphoma. Moreover, a number of pre-clinical approaches are being investigated to improve CIK cell therapy to enhance its anti-tumor activity.
1. Background
Contrary to solid cancers, hematologic malignancies (blood cancers) have some unique characteristics and often require different treatments. Importantly, it is now well established that the hematologic malignancies (lymphoma, leukemia, and myeloma) despite sharing some common clinical features are also biologically distinct entities. Among them, lymphoma, a cancer of lymphocytes, is a very heterogeneous group of neoplasms exhibiting diverse clinical presentations, prognoses, and therapeutic responses and includes more than 70 different subtypes. Lymphomas are conventionally divided into two main groups, Hodgkin’s lymphoma (HL) and non-Hodgkin’s lymphoma (NHL), with both types having multiple early clinical manifestations, often delaying the diagnosis. By comparison, HLs are rare and less heterogeneous, whereas NHLs are more a common and highly heterogeneous group of B-, T-, or NK-cell neoplasms. HL only accounts for approximately 10% of newly diagnosed lymphoma [
1]. The complex heterogeneity can also be evident from the fact that in HL alone, the distinctions can be made between two subtypes, classic HL (cHL) and rare nodular lymphocyte-predominant HL (nLPHL) [
2]. Besides, cHL is further categorized into nodular sclerosis (NS), mixed cellularity (MC), lymphocyte-rich (LR) and lymphocyte-depleted (LD) cHL. The cHL subtype is composed of Hodgkin (H) and Reed-Sternberg (RS) cells, collectively referred to as Hodgkin and Reed-Sternberg cells (HRS). The scenario is more complex in NHL, which is classified according to the type of lymphocytes involved: B lymphocytes (B-cells) or T lymphocytes (T-cells). Diffuse large B-cell lymphoma (DLBCL), follicular lymphoma (FL), and Burkitt’s lymphoma (BL) are common NHL types that are usually classified according to their aggressive or slow growing characteristics.
As per reports from the SEER database (
https://seer.cancer.gov/, accessed on 3 August 2021), HL affected approximately 219,128 people in the United States in 2018. To mention, HL is quite curable, but there are differences in incidence rates, sex and age distribution (young and adults), mainly based on the socioeconomic background [
3]. The most common age group of diagnosis is generally between 20 and 34 years old. Contrarily, NHL pose a challenge to the treatment response. According to the German Center for Cancer Registry Data (ZfKD), about 19,200 people in Germany were diagnosed with NHL in 2017, mostly in people of advanced age (average: women 72 years, men 70 years). In 2020, the number of incident cases is increased to 18,549 in Germany from the data of GLOBOCAN 2020 (
http://gco.iarc.fr/today, accessed on 25 November 2021). Similarly, approximately 81,560 patients are expected to be diagnosed with NHL in the United States in 2021 according to data from Cancer Statistics Center of American Cancer Society (
http://cancerstatisticscenter.cancer.org/, accessed on 3 August 2021).
2. Cytokine-Induced Killer Cells
Since cancer immunotherapy focuses on enhancing the anti-cancer capabilities of immune cells rather than killing cancer cells, one such potential approach of adoptive immunotherapy is cytokine-induced killer (CIK) therapy, which eliminates cancer cells by transfusing immune cells that have been expanded and activated in vitro. Phenotypically, CIK cells are heterogeneous in nature and composed of CD3+CD56− (T cells), CD3−CD56+ (NK cells), and CD3+CD56+ (NKT cells) cell populations [
18]. In fact, the CD3+CD56+ subset is considered as the major effector cells that exert potent anti-tumor cytotoxicity in a major histocompatibility complex (MHC)-unrestricted manner. The generation of CIK cells was first reported in 1991 by sequential incubation of peripheral blood mononuclear cells (PBMCs) with interferon-γ (IFN-γ), anti-CD3 monoclonal antibody (OKT3), and recombinant human interleukin-2 (rhIL-2) [
19]. The manufacturing process of autologous and allogeneic CIK cells is shown in
Figure 1.
Particularly, apparent differences can be drawn between CIK cells and the impressive immunologic approaches against lymphoma, including CAR-T and BiTE therapies (
Table 1). Unlike CAR-T and BiTE that recognize tumor cells by targeting the tumor-associated antigens (TAAs), the majority of the CIK cell cytotoxicity results from the natural killer group 2 member D (NKG2D) interactions [
20,
21,
22,
23]. NKG2D is expressed on all NK cells and recognizes at least six ligands that are relatively restricted on malignant tissues, including MHC class I-related molecules A and B (MICA and MICB) and members of the UL16-binding protein family (ULBP1-4) [
24]. The manufacturing of CAR-T cells requires genetic modification and cell expansion ex vivo, which is time-consuming and brings some financial considerations. However, the relative easiness of CIK cell preparation facilitates the fast growing of CIK cell therapy. Besides, cytokine release syndrome (CRS) is the most severe toxicity in CAR-T and BiTE therapies. It is associated with the rapid and extensive activation of T cells and the release of high-level proinflammatory cytokines (TNFα and IL-6) [
25]. Nonetheless, the crucial advantages of CIK cells are the relatively low toxicity and lack of graft-versus-host diseases (GVHD) response. The most common side effects in CIK cell therapy are fever, chills, fatigue, headache, and skin rash, and patients can usually recover with simple treatment [
26].
Table 1. Similarities and differences between CIK cells, CAR-T cells and BiTEs in lymphoma.
| |
CIK Cells |
CAR-T Cells |
BiTEs |
| Manufacturing Process |
PBMCs sequentially activated with 1000 IU/m IFN-γ on day 0, and 50 ng/mL anti-CD3 mAb and 600 IU/mL IL-2 on the following day; IL-2 supplemented every 2–3 days |
T cells with CAR gene transduction primarily by lentiviruses; CARs consist of an scFv based ectodomain for antigen-binding, a transmembrane domain, and an endodomain containing TCR CD3ζ chain with or without costimulatory signaling components |
Antibodies designed to bind to a selected TAA and CD3 on T cells simultaneously; produced in bioreactors by mammalian cell lines as secreted polypeptides |
| Effector Cells |
CD3+CD56+ cells |
Mostly αβ-TCR+ T cells |
Endogenous CD8+ or CD4+ T cells |
| Cell Source |
Autologous/allogeneic |
Autologous/allogeneic |
Autologous |
| Target Antigen |
MIC A/B and ULBP1–4 |
CD19, CD20, CD22, CD30, BCMA, etc. |
CD19 |
| MHC Restriction |
Dual-functional capability (non-MHC-restricted and TCR-mediated lysis) |
TAA recognition by CARs is MHC-unrestricted |
MHC-unrestricted |
| Mechanism |
Release of perforin and granzyme B from CIK cells |
Release of perforin and granzyme B from CAR-T cells |
Activating T cells to release perforin and granzyme B by linking TAAs to CD3 on T cells |
| Toxicities and Side effects |
Low-grade toxicities including fever, chills, fatigue, headache, and skin rash; grade 3 and 4 toxicities are rare; limited GVHD response in the allogeneic setting |
CRS, ICANS, and MAS/HLH; potentially life-threatening |
CRS and ICANS; severe toxicities are one of the major concerns |
| Clinical Efficacy |
Varied due to heterogeneity of expension method and study design |
Axicabtagene ciloleucel: 83% ORR, 58% CR; Tisagenlecleucel: 54% ORR, 40% CR; Lisocabtagene maraleucel: 73% ORR, 53% CR [27,28,29] |
Blinatumomab: 36% to 69% ORR in relapsed/refractory NHL [11,30] |
CIK cells, cytokine-induced killer cells; MIC A/B, MHC class I-related molecules A and B; ULBP1–4, UL16-binding protein; GVHD, graft-versus-host diseases; CAR, chimeric antigen receptors; scFv, single-chain variable fragment; TCR, T cell receptor; TAA, tumor-associated antigen; CRS, cytokine release syndrome; ICANS, immune effector cell-associated neurotoxicity syndrome; MAS/HLH, Macrophage activation syndrome/hemophagocytic lymphohistiocytosis; CR, complete remission; ORR, objective response rate; BiTE, bispecific T cell engager.
3. Improving CIK Cell Therapy on Lymphoma
Despite the positive clinical benefit observed in trials, it is difficult to achieve long-lasting response and complete cancer eradication in patients with refractory or relapsed lymphoma. Therefore, a number of pre-clinical approaches are being investigated to improve CIK cell therapy to enhance its anti-tumor activity (
Figure 2). Among these innovative methods, bispecific antibodies (bsAb) represent a promising development bringing targeted antigen on tumor cells into close proximity to receptors on cytotoxic T-cells, and thereby triggering T-cell receptor signaling and anti-tumor immune response [
53]. In a particular study, it was reported that the bsAb CD19 × CD5 (HD37 × T5.16) enhanced the cytotoxicity activity of CIK cells against B lymphoma cells [
54]. Moore et al. used a bispecific antibody platform known as dual affinity retargeting (DART) to eradicate B-cell lymphomas by targeting the B-cell-specific antigen CD19 and the TCR/CD3 complex to effector T cells [
55]. Subsequently, it was shown that CIK cells and CD19xCD3 DART can control and/or eradicate patient-derived tumor xenografts from chemo-refractory B-ALL and diffuse large B-cell lymphoma (DLBCL) patients [
56].
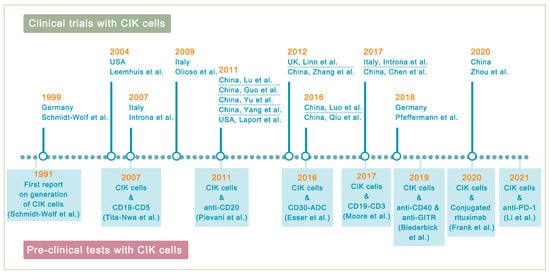
Figure 2. Highlights in the development of CIK cell immunotherapy. In 1991, the development of CIK therapy began (in Germany) and continued in several countries, with 2011 being the year with the most clinical trial reports. The supporting pre-clinical models that are used to improve the therapeutic activity of CIK cells are also highlighted.
Likewise, studies also have shown an enhancement of CIK cell activity when combined with anti-CD20 antibodies. For instance, Pievani et al. showed that the addition of the anti-CD20 antibodies GA101 or rituximab in B-NHL increased the cytotoxicity of CIK cells by 35% and 15%, respectively [
57]. The authors also suggested that activation of the MAPK pathway may be a possible mechanism for the anti-apoptosis effect on CIK cell proliferation. Esser et al., investigated the effect of CIK cells in combination with brentuximab vedotin (SGN-35) on three different CD30+ lymphoma cell lines (Daudi, KI-JK, and L-540), and was found that the combined approach led to better results in vitro [
58]. Recently, a novel antibody-cell conjugation method for the enhancement and characterization of cytokine-induced killer cells has been presented [
59]. The authors demonstrated that CIK cells conjugated with rituximab exhibited increased cytotoxic activity against CD20+ lymphoma cell lines and suggested that without any genetic modification, CIK cells can be rapidly equipped with monoclonal antibodies to target tumor cells.
Biederbick et al. recently contributed to raise concerns about synergistic molecular mechanisms of CIK cells by using a combination of anti-CD40 and anti-GITR mAb in the human lymphoma cell lines SU-DHL-4 and Daudi (both CD40-positive) [
60]. More recently, Li et al. reported an increase in IFN-γ secretion in B-NHL cell lines treated with CIK alone or with the PD-1 antibody, yet this trend was not observed for PD-L1, raising the question of whether PD-1 and PD-L1 are comparable and interchangeable in the clinical practice [
61].