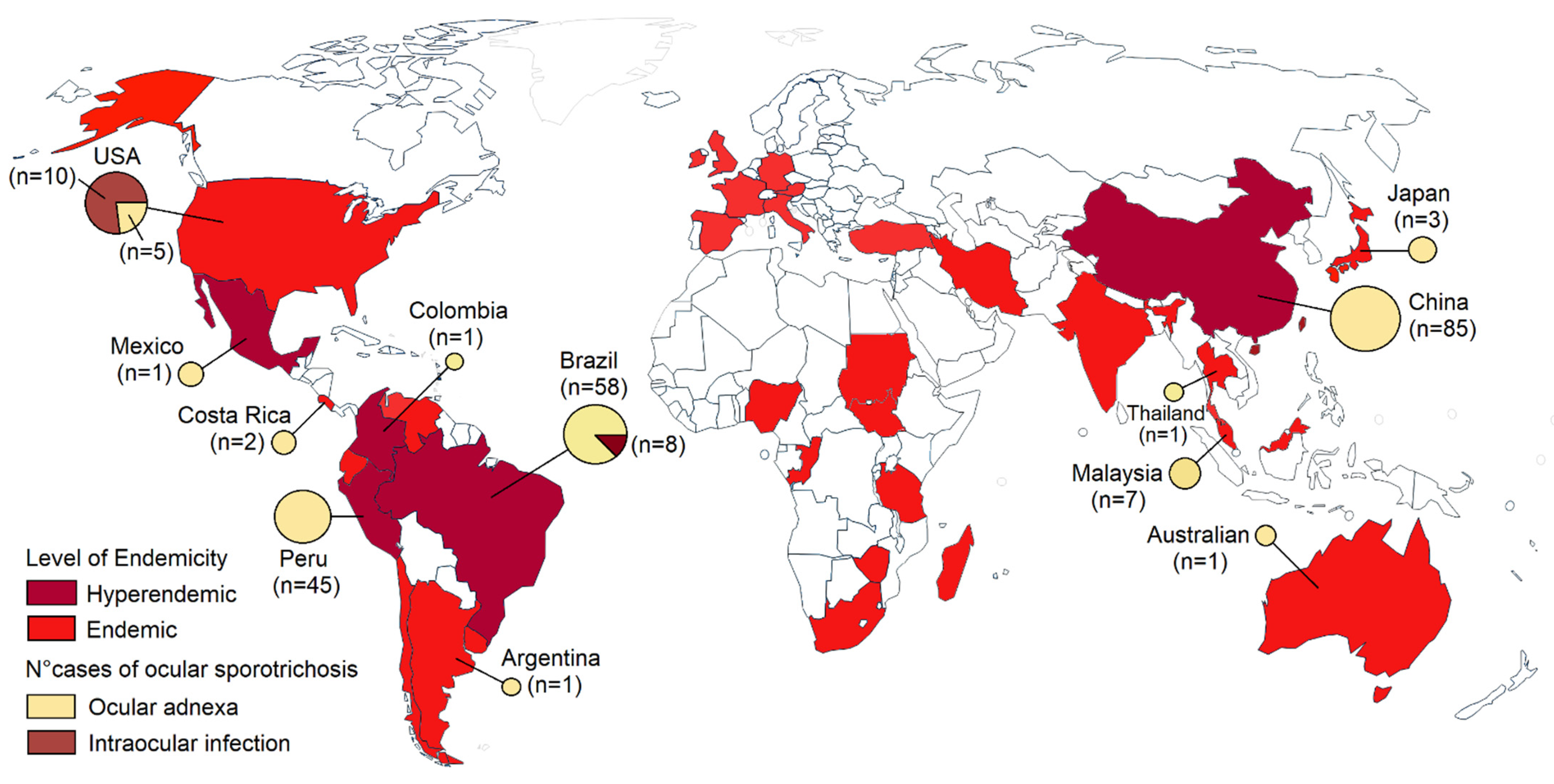
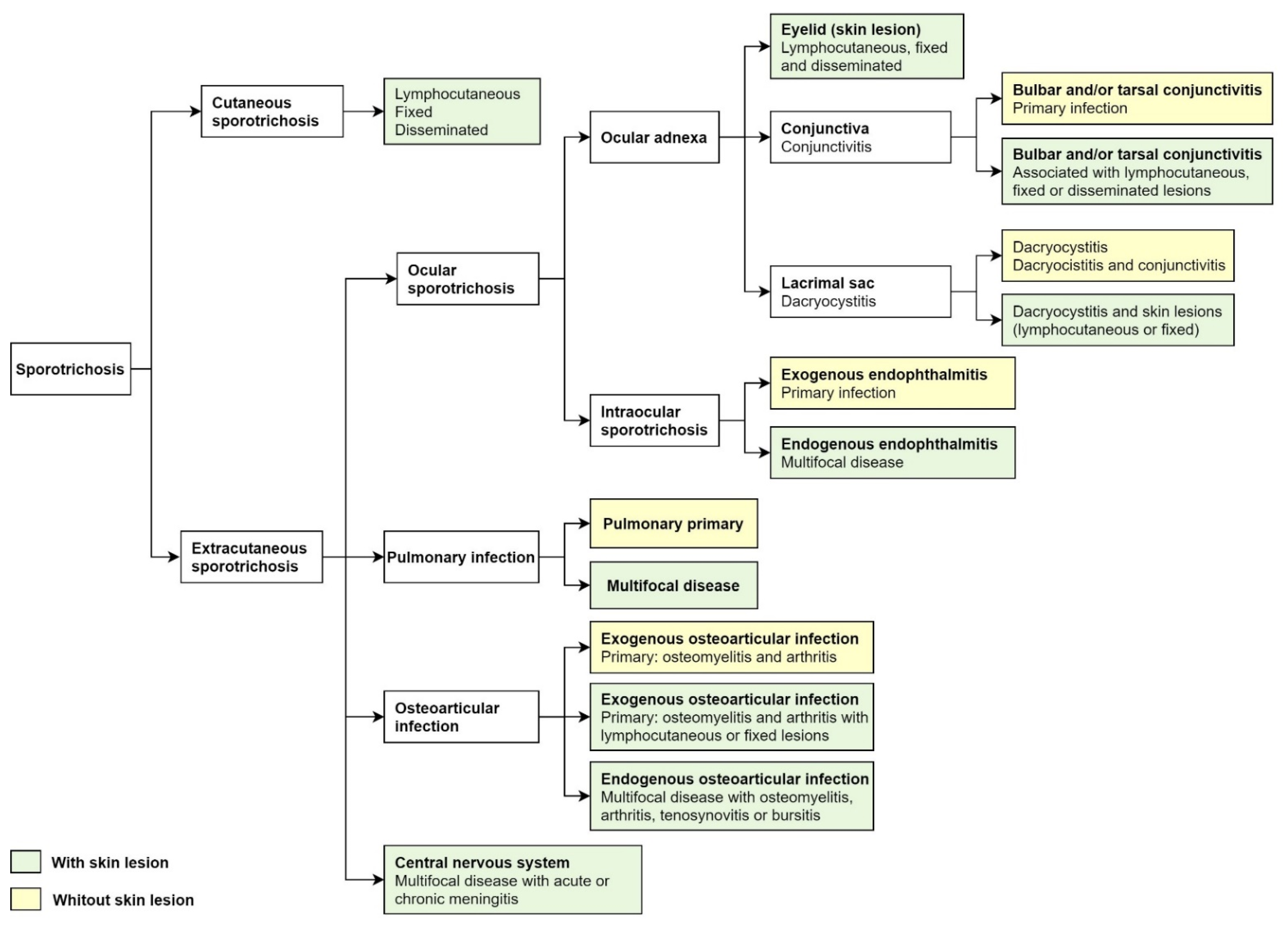
Sporotrichosis is a subacute or chronic mycosis predominant in tropical and subtropical regions. It is an infection of subcutaneous tissue caused by Sporothrix fungus species, but occasionally resulting in an extracutaneous condition, including osteoarticular, pulmonary, nervous central system, and ocular disease. Cases of ocular sporotrichosis are rare, but reports have been increasing in recent decades. Ocular infections usually occur in hyperendemic areas of sporotrichosis. For its classification, anatomic criteria are used. The clinical presentation is the infection in the ocular adnexal and intraocular infection. Ocular adnexa infections include palpebral, conjunctivitis, and infections of the lacrimal sac. Intraocular infection includes exogenous or endogenous endophthalmitis.
- sporotrichosis
- Sporothrix
- ocular infection
- conjunctivitis
- ocular adnexa
- endophthalmitis
1. Introduction
2. Epidemiology and Etiology
3. Clinical Presentation

|
Intraocular Sporotrichosis [9 |
|---|
|
Type of Disease, Agent | ] | ||||
|---|---|---|---|---|---|
Ocular Adnexal Sporotrichosis |
Intraocular Sporotrichosis |
||||
|
Epidemiology (most commonly found in) |
Eyelid sporotrichosis in China and Peru Conjunctivitis and dacryocystitis in Brazil |
The United States and Brazil |
|||
|
Fungal infection |
|
|
|||
|
Age group |
|||||
|
Bacterial infection |
2–89 years |
12–75 years |
|||
|
|
Occurs in children |
|||
|
Viral infection |
Yes (frequent) |
|
Yes (rare) |
||
|
Clinical course |
Less aggressive |
Aggressive |
||
|
Non-infectious |
|
Site of lesion |
Eyelid, conjunctiva, and lacrimal sac |
Scleral, cornea, retina, choroid, and optic nervous |
|
|
Complications |
Rare (cases of bulbar conjunctivitis) |
Irreversible vision loss (endophthalmitis) |
|||
|
Risk factor |
Traumatic inoculation with plant material and contact with cats |
Traumatic inoculation with plant material, HIV infection, and residence in a hyperendemic area of sporotrichosis |
4. Differential Diagnoses
| ||
|
|
5. Laboratory Diagnosis
6. Treatment
References
- Barros, M.B.D.L.; de Almeida Paes, R.; Schubach, A.O. Sporothrix schenckii and Sporotrichosis. Clin. Microbiol. Rev. 2011, 24, 633–654.
- Chakrabarti, A.; Bonifaz, A.; Gutierrez-Galhardo, M.C.; Mochizuki, T.; Li, S. Global epidemiology of sporotrichosis. Med. Mycol. 2015, 53, 3–14.
- Rodrigues, A.M.; Della Terra, P.P.; Gremião, I.D.; Pereira, S.A.; Orofino-Costa, R.; de Camargo, Z.P. The threat of emerging and re-emerging pathogenic Sporothrix species. Mycopathologia 2020, 185, 813–842.
- Queiroz-Telles, F.; Fahal, A.H.; Falci, D.R.; Caceres, D.H.; Chiller, T.; Pasqualotto, A.C. Neglected endemic mycoses. Lancet Infect. Dis. 2017, 17, 367–377.
- Bonifaz, A.; Tirado-Sánchez, A. Cutaneous Disseminated and Extracutaneous Sporotrichosis: Current Status of a Complex Disease. J. Fungi 2017, 3, 6.
- Orofino-Costa, R.; de Macedo, P.M.; Rodrigues, A.M.; Bernardes-Engemann, A.R. Sporotrichosis: An update on epidemiology, etiopathogenesis, laboratory and clinical therapeutics. An. Bras. Dermatol. 2017, 92, 606–620.
- Gutierrez-Galhardo, M.C.; Freitas, D.F.S.; Valle, A.C.F.D. Clinical Forms of Human Sporotrichosis and Host Immunocompetence. In Sporotrichosis; Springer: Berlin/Heidelberg, Germany, 2015; pp. 73–82.
- Soto, M.C.R. Sporotrichosis in the Ocular Adnexa: 21 Cases in an Endemic Area in Peru and Review of the Literature. Am. J. Ophthalmol. 2016, 162, 173–179.e3.
- Ramírez-Soto, M.C. Differences in clinical ocular outcomes between exogenous and endogenous endophthalmitis caused by Sporothrix: A systematic review of published literature. Br. J. Ophthalmol. 2018, 102, 977–982.
- Ramírez-Oliveros, J.F.; Casz Schechtman, R.; de Vries, H.J.; Lora, L.; Arinelli, A.C.; da Costa Nery, J.A.; Freitas, D.F.S. Ocular adnexal sporotrichosis: A case series. JAAD Case Rep. 2021, 13, 52–56.
- Zhang, Y.; Wang, Y.; Cong, L.; Yang, H.; Cong, X. Eyelid sporotrichosis: Unique clinical findings in 72 patients. Australas. J. Dermatol. 2016, 57, 44–47.
- Arinelli, A.; Aleixo, A.L.Q.D.C.; Freitas, D.F.S.; Valle, A.C.F.D.; Almeida-Paes, R.; Gutierrez-Galhardo, M.C.; Curi, A.L.L. Ocular Sporotrichosis: 26 Cases with Bulbar Involvement in a Hyperendemic Area of Zoonotic Transmission. Ocul. Immunol. Inflamm. 2020, 28, 764–771.
- Gremião, I.D.F.; Oliveira, M.M.E.; De Miranda, L.H.M.; Freitas, D.F.S.; Pereira, S.A. Geographic Expansion of Sporotrichosis, Brazil. Emerg. Infect. Dis. 2020, 26, 621–624.
- Yao, L.; Song, Y.; Zhou, J.-F.; Cui, Y.; Li, S.-S. Epidemiological and clinical comparisons of paediatric and adult sporotrichosis in Jilin Province, China. Mycoses 2020, 63, 308–313.
- Toriello, C.; Brunner-Mendoza, C.; Ruiz-Baca, E.; Duarte-Escalante, E.; Pérez-Mejía, A.; Del Rocío Reyes-Montes, M. Sporotrichosis in Mexico. Braz. J. Microbiol. 2021, 52, 49–62.
- Ramírez-Soto, M.C. Sporotrichosis: The Story of an Endemic Region in Peru over 28 Years (1985 to 2012). PLoS ONE 2015, 10, e0127924.
- Lopes-Bezerra, L.M.; Mora-Montes, H.M.; Zhang, Y.; Nino-Vega, G.; Rodrigues, A.M.; De Camargo, Z.P.; De Hoog, S. Sporotrichosis between 1898 and 2017: The evolution of knowledge on a changeable disease and on emerging etiological agents. Med. Mycol. 2018, 56, 126–143.
- Gremião, I.D.F.; Miranda, L.H.M.; Reis, E.G.; Rodrigues, A.M.; Pereira, S.A. Zoonotic Epidemic of Sporotrichosis: Cat to Human Transmission. PLoS Pathog. 2017, 13, e1006077.
- Davies, C.; Troy, G.C. Deep mycotic infections in cats. J. Am. Anim. Hosp. Assoc. 1996, 32, 380–391.
- Nakamura, Y.; Sato, H.; Watanabe, S.; Takahashi, H.; Koide, K.; Hasegawa, A. Sporothrix schenckii isolated from a cat in Japan. Mycoses 1996, 39, 125–128.
- Ramírez-Soto, M.C.; Malaga, G. Subcutaneous mycoses in Peru: A systematic review and meta-analysis for the burden of disease. Int. J. Dermatol. 2017, 56, 1037–1045.
- Ramírez-Soto, M.C.; Aguilar-Ancori, E.G.; Tirado-Sánchez, A.; Bonifaz, A. Ecological Determinants of Sporotrichosis Etiological Agents. J. Fungi 2018, 4, 95.
- Morrison, A.S.; Lockhart, S.R.; Bromley, J.G.; Kim, J.Y.; Burd, E.M. An environmental Sporothrix as a cause of corneal ulcer. Med Mycol. Case Rep. 2013, 2, 88–90.
- Queiroz-Telles, F.; Buccheri, R.; Benard, G. Sporotrichosis In Immunocompromised Hosts. J. Fungi 2019, 5, 8.
- Brunette, I.; Stulting, R.D. Sporothrix schenckii scleritis. Am. J. Ophthalmol. 1992, 114, 370–371.
- Witherspoon, C.D.; Kuhn, F.; Owens, S.D.; White, M.F.; Kimble, J.A. Endophthalmitis due to Sporothrix schenckii after penetrating ocular injury. Ann. Ophthalmol. 1990, 22, 385–388.
- Cassady, J.R.; Foerster, H.C. Sporotrichum schenckii endophthalmitis. Arch. Ophthalmol. 1971, 85, 71–74.
- Levy, J.H. Intraocular sporotrichosis. Report of a case. Arch. Ophthalmol. 1971, 85, 574–579.
- Cartwright, M.J.; Promersberger, M.; Stevens, G.A. Sporothrix schenckii endophthalmitis presenting as granulomatous uveitis. Br. J. Ophthalmol. 1993, 77, 61–62.
- Agger, W.A.; Caplan, R.H.; Maki, D.G. Ocular sporotrichosis mimicking mucormycosis in a diabetic. Ann. Ophthalmol. 1978, 10, 767–771.
- Font, R.L.; Jakobiec, F.A. Granulomatous necrotizing retinochoroiditis caused by Sporotrichum schenkii. Report of a case including immunofluorescence and electron microscopical studies. Arch. Ophthalmol. 1976, 94, 1513–1519.
- Kurosawa, A.; Pollock, S.C.; Collins, M.P.; Kraff, C.R.; Tso, M.O. Sporothrix schenckii endophthalmitis in a patient with human immunodeficiency virus infection. Arch. Ophthalmol. 1988, 106, 376–380.
- Silva-Vergara, M.L.; de Camargo, Z.P.; Silva, P.F.; Abdalla, M.R.; Sgarbieri, R.N.; Rodrigues, A.M.; dos Santos, K.C.; Barata, C.H.; Ferreira-Paim, K. Disseminated Sporothrix brasiliensis infection with endocardial and ocular involvement in an HIV-infected patient. Am. J. Trop. Med. Hyg. 2012, 86, 477–480.
- Biancardi, A.L.; Freitas, D.F.; Valviesse, V.R.; Andrade, H.B.; de Oliveira, M.M.; do Valle, A.C.; Zancope-Oliveira, R.M.; Galhardo, M.C.; Curi, A.L. Multifocal choroiditis in disseminated sporotrichosis in patients with HIV/AIDS. Retin. Cases Brief Rep. 2017, 11, 67–70.
- Vieira-Dias, D.; Sena, C.M.; Oréfice, F.; Tanure, M.A.; Hamdan, J.S. Ocular and concomitant cutaneous sporotrichosis. Mycoses 1997, 40, 197–201.
- Lopes-Bezerra, L.M.; Mora-Montes, H.M.; Bonifaz, A. Sporothrix and Sporotrichosis. In Current Progress in Medical Mycology; Springer: Berlin/Heidelberg, Germany, 2017; Chapter 9; pp. 309–331.
- Filho, A.R.G.; Estacia, C.T.; Gameiro, R.R.; Vieira, L.D.M.F.; da Costa, D.S. Ocular and cutaneous sporotrichosis. Am. J. Ophthalmol. Case Rep. 2020, 20, 100885.
- Liu, F.; Liu, Y.; Yuan, N.; Zhang, X.; Cao, M.; Dong, J.; Zhang, J. Fixed Cutaneous Sporotrichosis Due to Sporothrix globosa. Clin. Cosmet. Investig. Dermatol. 2021, 14, 91–96.
- Ribeiro, C.R.; Silva, B.P.; Almeida Costa, A.A.; Neto, A.B.; Vieira, L.A.; Lima, M.A.; Lima, M.H.C. Ocular Sporotrichosis. Am. J. Ophthalmol. Case Rep. 2020, 19, 100865.
- Bonifaz, A.; Toriello, C.; Araiza, J.; Ramírez-Soto, M.C.; Tirado-Sánchez, A. Sporotrichin Skin Test for the Diagnosis of Sporotrichosis. J. Fungi 2018, 4, 55.
- Kauffman, C.A.; Bustamante, B.; Chapman, S.W.; Pappas, P.G.; Infectious Diseases Society of America. Clinical practice guidelines for the management of Sporotrichosis: 2007 update by the Infectious Diseases Society of America. Clin. Infect. Dis. 2007, 45, 1255–1265.
- Yamada, K.; Zaitz, C.; Framil, V.M.; Muramatu, L.H. Cutaneous sporotrichosis treatment with potassium iodide: A 24-year experience in São Paulo State, Brazil. Rev. Inst. Med. Trop. Sao Paulo 2011, 53, 89–93.
- Xue, S.; Gu, R.; Wu, T.; Zhang, M.; Wang, X. Oral potassium iodide for the treatment of sporotrichosis. Cochrane Database Syst. Rev. 2009, 7, CD006136.
- Macedo, P.M.; Lopes-Bezerra, L.M.; Bernardes-Engemann, A.R.; Orofino-Costa, R. New posology of potassium iodide for the treatment of cutaneous sporotrichosis: Study of efficacy and safety in 102 patients. J. Eur. Acad. Dermatol. Venereol. 2015, 29, 719–724.
- Ramírez-Soto, M.C.; Bonifaz, A.; Tirado-Sánchez, A. Endophthalmitis in patients co-infected by HIV and Sporotrichosis: A systematic review of published case reports. Eye 2018, 32, 1678–1680.
