Ursolic acid (UA) is a promising triterpenoid compound present in several plants’ leaves, flowers, and fruits. It shows a broad range of pharmaceutical properties and therapeutic effects. UA has been utilized as a herbal medicine with excellent pharmacological activities.
- ursolic acid
- diabetic neuropathy
- inflammatory diseases
- inhibitors
- targeted therapy
1. Introduction
Ursolic acid (UA) is a promising triterpenoid compound present in several plants’ leaves, flowers, and fruits [1]. It shows a broad range of pharmaceutical properties and therapeutic effects [2]. UA has been utilized as a herbal medicine with excellent pharmacological activities [3][4][3,4]. It mediates alterations in many signaling pathways and subsequently prevents the progression of chronic diseases [5], demonstrating its anti-inflammatory [6], anti-oxidant [7], anti-carcinogenic [8], anti-diabetic [9], neuroprotective effects [10]. UA is effective in the treatment of many inflammatory diseases [4], including Parkinson’s disease [11] and diabetes [12]. In addition, UA has been implicated in neurodegenerative and psychiatric disorders [13]. It has considerable potential as an oral anti-inflammatory and neural repair drug [14], attenuating neuropathic pain in animal models that can probably be attributed to its anti-oxidant and anti-inflammatory properties [15]. The mechanisms of UA by which applies these beneficial consequences might engage regulation of metabolic and atrophy pathway in skeletal muscles, insulin pathway in adipose tissue, apoptotic and NF-κB pathway in tumor cells, level of oxidants and metabolic pathway in the liver, anti-oxidants and inflammation in the brain [16][17][18][16,17,18] .
Cancer is the leading cause of human death in economically developed countries [19][20][21][19,20,21]. The cancer burden keeps on enhancing in developing countries due to increasing aging in the population [21][22][21,22]; cancer is a major cause of adult deaths worldwide [21][23][21,23]. Cancer is a complex disease that may be inhibited [24][25][24,25]; cancer progression might take around 10 to 30 years to develop, starting initiation, promotion for development, and progression [24][25][24,25]. Hence, the slow growth of the disease potentially permits interference in the development of tumors into advanced stages and metastases. This disease has a high incidence and mortality rate; its treatment indicates a significant clinical challenge. Hence, the advantages of present chemotherapeutics are inadequate because they tend to cause DNA damage in healthy cells [26][27][26,27]. However, targeting the regulation of cancer cells without causing toxic effects in healthy cells is a potential strategy for cancer treatment [28][29][28,29].
Inflammation engages the activation and employment of phagocytes (neutrophils, macrophages), NK cells, and the discharge of cytokines through activated cells that are crucial to the host defense system. Since the chronic inflammation that continues yet after removal of the pathogen(s) was linked with many diseases, including cancer [30][48], neoplasms, inflammatory bowel disease [31][49], Alzheimer’s disease [32][50], therefore, dysregulation of enzymes and cytokines, might contribute to the pathogenesis of several chronic inflammatory diseases [33][51]. NF-κB , NF-AT, and AP1 with JNK, ERK, and p38 are well-known for regulating inflammatory cytokines and enzymes targeted through various investigators to improve chronic inflammation [34][35][36][52,53,54]. Inflammation plays a fundamental role in the pathogenesis of DN [37][55].
The complexities of DN and inflammatory diseases have considerably evolved over the years. Efforts for understanding the etiology of DN and inflammatory diseases are in progress to design attractive therapeutic approaches. In this context, UA may be a potent therapeutic molecule for DN and inflammatory diseases. UA and its derivatives are potential therapeutic candidates that can be explored to treat DN and inflammatory diseases. In this review, we systematically collected current findings concerning biochemistry, potency, pharmacological aspect, drug delivery system, and clinical trials of UA.
2. Biological Potency of UA
The molecular action of bioactive molecules might open up novel opportunities to the scientific community for developing and improving new therapeutic approaches for tackling dreadful diseases, including neurodegenerative disorders. UA is one such plant-based therapeutic metabolite, which plays a vital function in cell death, angiogenesis, metastasis, and inflammatory processes [38][59]. Table 12 presents various health benefits, including anti-apoptotic, anti-oxidant, anti-inflammatory, anti-carcinogenic, anti-rheumatic, anti-tumoral, anti-viral, trypanocidal, etc. , of UA [39][40][81,82]. UA has anti-cancer activity due to low toxicity and commercial accessibility forms [41][42][80,83].
| Disease | Experimental Subject | Dosage | Beneficial Effects | References | |
|---|---|---|---|---|---|
| Diabetes | 3T3-L1 adipocytes | 1 μg/mL for 10 min | ↑ Akt, insulin receptor, and GLUT 4 ↑ Glycogen synthase kinase-3β |
[43] | [84] |
| Diabetes | Streptozotocin-injected male ICR mice |
0.5 g/kg for 4 weeks | ↓ TNF-α and Glucose ↑ Insulin (pancreatic, plasma) |
[44] | [85] |
| Diabetes | Streptozotocin-injected male mice |
200 mg/kg per day for 6 weeks |
↓ Adipocyte dysfunction ↓ Fasting blood glucose ↓ PPAR γ and aP2 ↑ Bone formation |
[45] | [86] |
| Metabolic syndrome | Diagnostics of metabolic syndrome patients |
Orally 150 mg/kg for 12 weeks | ↓ Body weight, BMI, and waist circumference ↓ Fasting glucose |
[46] | [87] |
| Subarachnoid hemorrhage (SAH) |
Male Sprague Dawley experimental SAH rat model |
25 and 50 mg/kg at 0.5, 24, and 47 h after SAH |
↓ MDA ↑ Neurological score ↑ Cerebral vasospasm ↓ BBB permeability (EB content) ↑ GSH/GSSH ratio, SOD activity, and Catalase activity ↓ Apoptotic index ↓ Caspase-3, -9 mRNA expression |
[47] | [88] |
| Parkinson’s disease | Male Swiss albino mice |
5, 25, and 50 mg/kg for 21 days |
↑ Rotarod test ↑ Hanging time ↓ Nitrite level ↓ Narrow beam walking test ↑Acidhomovanilic acid ↑ Dopamine |
[48] | [89] |
| Cerebral ischemia and reperfusion injury |
Male Sprague Dawley rats |
5, 10, and 20 mg/kg at 0.5, 24, and 47 h after reperfusion |
↓ Neurological deficit score ↓ Infarct volume ↑ PPARγ protein level ↑ Number of intact neurons ↓MMP-2 & -9 protein levels |
[49] | [90] |
| IL-1β or TNF-α- induced C6 glioma invasion |
Rat C6 glioma cells | 5, 10, and 20 μM for 24 h |
↓ MMP-9 activity by TNF-α or IL-1β ↓ IκB kinase activity by IL-1β or TNF-α ↓ IκBα activity by IL-1β or TNF-α ↓ NF-κB activity |
[50] | [91] |
| D-Galactose-induced neurodegenerative changes |
Male Kunming strain mice |
10 mg/kg for 8 weeks |
↓ ROS level ↓ AGEs level ↓ Number of CD11b-stained cells, ↓ Carbonyl protein level GFAPstained cells, and RAGE- positive cells ↓ iNOS, IL-6, IL-1β, COX-2, and TNF-α protein levels |
[51] | [92] |
| Domoic acid-induced cognitive deficits |
Male ICR mice | 100 mg/kg for 3 weeks | ↑p-Akt ↑ HO-1 ↑ p-FOXO1 ↑ Complex I-V ↑ Electron transport chain activity ↑ APR and ATP |
[52] | [93] |
| Adrenocorticotrophic hormone-producing pituitary adenoma |
AtT20 cells (mouse corticotrophic tumor cell line) |
10, 20, and 40 μM for 24 h |
↓ ACTH release ↓ POMC mRNA expression ↓ ACTH protein level ↑ p-JNK/JNK protein level |
[53] | [94] |
↓, Decrease; ↑, Increase.
UA is popular due to its anti-proliferative properties, the incentive of tumor cell death, an obstacle of tumorigenesis, and inhibiting the cell cycle in tumors cells. Hence, examining one cell death mechanism that indicated UA could prevent NF-κB pathway through p65 phosphorylation repression, effecting a mandatory reduction in several downstream oncogenes, including Bcl-xL and Bcl-2. The anti-cancer effectiveness of UA is weak due to its lesser solubility that reduces the drug absorption in the human body system, which causes challenges in achieving comprehensive benefits. However, it is required for making its derivatives by semi-synthetic alterations for improving its anti-cancer action. Frequently, the modifications of UA occur on positions C-3, C12–C13, and positions C-28 [54][55][56][63,76,95]. Antimicrobial activity of UA compounds against Mycobacterium tuberculosis H37Rv has been recently reported [57][58][96,97]. UA is currently in different phases of clinical studies due to its therapeutic effects and selectivity against several diseases [59][60][98,99].
3. Bioavailability and Pharmacokinetic Properties of UA
Cell membrane permeability and pharmacokinetics are vital in the clinical development and improvement of novel biologically active agents/compounds with an outlook for considering their performance in vivo and establishing the most acceptable dosage regimen. Hence, pentacyclic triterpenoids usually suffer from less oral bioavailability [61][100]. In the organism, a vast inter and intra character absorption variability shows challenges in accomplishing secure and efficient concentration of drug [62][101]. Physicochemical characters of the molecules are the first reason which affects bioavailability [63][102]. UA is a low molecular weight compound [64][58], with three hydrogen bond donors and acceptors. However, these properties for estimating the drug-likeness are in harmony with Lipinski’s rule [65][103]. UA has more lipophilicity [61][100] and less wettability [66][104]. Hence, their absorption is obstructed through slow partitioning between extracellular fluid and cell membrane and poor dissolution. UA can be inserted in the phospholipid bilayer while not taken up via cells [66][104].
Moreover, aqueous solubility is exaggerated through the crystalline structure of natural UA. Decreased particle size and amorphous state remarkably increased rate of dissolution and solubility of triterpenoid [67][105]. Adverse characteristics of UA should be addressed in the improvement of pharmaceutical dose shapes. Hence, for overcoming biological barriers, the second main factor is the capability of the drug [63][102]. The proof from in vitro permeability investigations involves which passive diffusion is the primary process of UA transport [63][102]. Hence, apparent permeability coefficients, estimated applying Caco-2 monolayers, have been in limits of oral absorption [63][102], which instant glucuronidation, and sulfation in the intestinal cells, are extremely unlikely [68][106]. UA is a substrate of cytochrome P450 and P-glycoprotein. Therefore their bio-availability can be limited through biotransformation and active efflux [67][69][105,107].
Many pharmacokinetic examinations have exposed where maximal plasma concentration subsequent oral administration of doses up to 300 mg/kg has been low, and removal half-life has been comparatively short (<1 h) [70][67][69,105]. This pharmacokinetic outline shows that fast elimination and tissue distribution in the pharmacological results of UA may not be honestly related to plasma concentrations. UA has broad tissue distribution, such as in the animal’s testes, colon, lung, kidney, spleen, brain, liver, heart and bladder [70][71][69,108]. The liver is the main organ of the triterpene disposition [71][108], and liver-related doses limit the toxicity in clinical trial phase I of UA liposomes [72][109]. UA can cross the blood-brain barrier, and they have potent neuroprotective effects [71][108]. Targeted delivery for the brain may be attained through particular delivery systems that use UA nano-lipid vesicles in the form of intranasal gel [73][110]. Hence, high lipophilicity influences triterpenoids for liver metabolism. However, a tissue distribution examination in mice has shown that the UA concentration in plasma was gradually reduced, but the concentration in the liver increased [74][111].
4. Pharmacological Aspects of UA
In cerebral ischemia and reperfusion injury, TLRs play a critical role by inducing the making of inflammatory mediators, including ILs and TNF-α [75][76][77][152,153,154]. TLR4 was primarily reported as receptors to endogenous ligands such as DAMPs, and HMGB1, during brain injury. UA controls the TLR pathway and shows prominent anti-inflammatory functions. UA demonstrates biological actions in the brain, such as anti-inflammatory, anti-oxidative, anti-rheumatic and anti-tumor effects [78][155]. UA decreases inflammatory cytokine-making to protect the brain from cerebral ischemia and reperfusion injury, probably by HMGB1/TLR4/NF-κB pathway [79][156]. UA might be helpful as a potential efficient adjunct for therapy to ischemic brain injury before reperfusion.
Inflammation plays an essential role in developing and progressing multiple diseases, including neuropathy, insulin resistance, and diabetes [80][157], cancer [81][82][83][84][85][158,159,160,161,162]. After injury and microbial attack, the inflammatory reaction is started to recover homeostatic tissue equilibrium between composition and physiological role. Hence, persistent inflammation can cause harm to tissues, affecting non-functioning tissues/organs [86][87][163,164]. Inflammation is an obscured incidence connected to the progression of various diseases, including neurodegenerative diseases and cancer [88][165]. Acute inflammation, with attendant cytokine action and the increased output of ROS, is reported like a tumor-promoting disease [89][90][91][166,167,168]. For detecting the anti-inflammatory activity, the study reported UA’s capability to reduce the making of TNF-α in A549 and RAW 267.4 cell lines infected by Mycobacterium tuberculosis and Con A-stimulated mouse splenocytes.
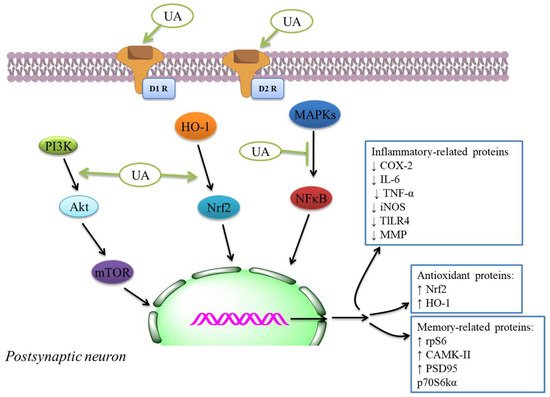
The authors examined UA action intending to reduce COX-2 and NO synthase levels found in roused cells. Hence, UA showed a considerable inhibitory effect of cytokine levels, immunomodulatory mediators, and liberate of NO. This compound may be used for tuberculosis and antibiotic therapy due to the UA’s anti-inflammatory effectiveness in cells [92][169]. IThe study showed in vitro inhibition of COX-2 action was because of UA and cranberry extracts [93][170], indicating potential anti-inflammatory and anti-oxidant activity ( Table 2 ). The anti-inflammatory activity was investigated by utilizing enzyme inhibitory examine in vitro COX-1 and COX-2 [94][95][171,172]. The molecular docking discoveries exhibited; the UA derivatives indicated elevated attraction to effective COX-2 site, potentially showing anti-inflammatory effectiveness by COX-2 inhibition. Hence, UA and its derivatives showed anti-inflammatory activity that might cause the development and improvement of potentially novel and secure COX-2 inhibitors [96][97][173,174]. The anti-inflammatory mechanisms inhibit main inflammatory cytokines, iNOS and COX expressions, and anti-oxidant mechanisms like the activation of Nrf2 signaling. The inflammatory and anti-oxidant mechanisms of neuroprotection through UA [98][175] are also indicated by the plethora of extra systemic results of UA in several experimental models [98][175]. The effects were linked with the inhibition of NF-κB translocation to the nucleus ( Figure 12 ) and decreased expression of iNOS, COX-2, TNF-α, and interleukin-6 that decreased the phosphorylation of p38MAPK in the mouse brain [99][146].
Terpenoids could have anti-oxidant results in vivo through mediating anti-oxidant defenses, including CAT, SOD, GPx, and GR, exhibited to their therapeutic potent in AD by a range of assays [100][101][102][103][104][176,177,178,179,180]. These compounds display anti-oxidant effects and possess anti-inflammatory functions. They are tackling complex diseases by what has been explained as one drug → multi-targets → one/many disease(s) therapeutic theory [105][181]. In this perspective, the therapeutic promising of UA like a prototype lead is exhibited in several CNS diseases, mainly by anti-inflammatory and anti-oxidant mechanisms. The anti-oxidant–anti-inflammatory axis was indicated to play a function in the anti-diabetic effect of UA as displayed in streptozotocin-mediated rats [106][182] in db/db diabetic mouse model [107][183] , DN models [108][184], diabetic-mediated monocyte dysfunction in mice [109][185], aortic damage in the STZ-mediated diabetic rats [110][186].
