2. Regulation of IL-4/IL-13 Genes Expression
Th2 cytokines production is governed by a network of factors comprising T-cell receptor (TCR) stimulation with antigenic peptide/main histocompatibility complex class II (MHC-II), with antigen dose playing a key role, co-stimulatory molecules, and an appropriate cytokine environment
[19][57]. The canonical pathway for IL-4/IL-13 production is activated by IL-4 leading to the phosphorylation of STAT6 and an upregulation of GATA binding protein 3 (GATA3)
[20][58]. The interaction between TCR and a peptide/MHC-II complex presented by an antigen-presenting cell (APC) is also involved in the activation of GATA3 expression. GATA3 constitutes the master of Th2 cell transcription regulation. However, IL-4/IL-13 production could be induced by non-canonical signaling pathways independently of IL-4 action. The IL-2-mediated STAT5 pathway is also a crucial element promoting production of Th2 cytokines. Notch signaling is another non-canonical pathway involved in IL-4/IL-13 expression upregulation. In addition, stimulation of TCR also activates a nuclear factor of activated T cells (NFAT) and activator protein-1 (AP-1), which are involved in
IL-4/
IL-13 transcriptional regulation
[21][59]. NFAT induction is mediated by calcium-calcineurin signaling, and the AP-1 is triggered via protein kinase C (PKC)/Ras-dependent pathway. AP-1 transcription factors comprise members of the Jun and Fos protein families characterized by a leucine zipper domain. NFAT binds to the
IL-4 and
IL-13 promoter region and cooperates with AP-1 family members (Fos/Jun), forming a transcriptionally active complex. An important role in the regulation of
IL-4 transcription has also been attributed to a c-Maf, basic region/leucine zipper transcription factor. Additionally, several other transcription factors are involved in orchestrating
IL-4/
IL-13 gene expression, including nuclear factor-κB (NF-κB), nuclear factor of IL-6 (NF-IL6), transcription factor CP2 (TFCP2), nuclear transcription factor Y (NFY), and Yin-yang 1 (YY1)
[22][60].
3. IL-4 and IL-13 Polymorphism in Inflammatory Arthritis
One of the commonly examined versions of
IL-13 is a single nucleotide polymorphism rs1800925 (-1055 C/T; promoter region).
IL-13 rs1800925 has been studied in RA patients; however, no associations have been found between this genetic variant and a susceptibility to the disease in three different studies comprising Chinese and Caucasian populations
[23][24][25][26][61,62,63,64]. Although stratification analyses in the study by Wang et al. revealed that the C allele was associated with RA risk in Chinese patients with erythrocyte sedimentation rate (ESR) < 25.00
[26][64].
IL-13 polymorphisms, such as rs1800925, rs20541 (G/A; Arg130Gln; exon 4), and rs848 (C/A; 3′ untranslated region), have also been studied in the context of PsA and psoriasis. Duffin et al. reported that among psoriasis patients the rs1800925 T, rs20541 A, and rs848 A alleles have the effect of protection from PsA
[23][61]. In line with these findings, significant associations between the rs1800925 C, rs20541 G, and rs848 C polymorphisms and PsA susceptibility have been found in two other studies conducted on Caucasian population
[27][28][65,66]. The rs848 C genetic variant and the rs1800925 C allele were also found to be associated with increased risk of PsA development in psoriasis patients in the study by Eder et al.
[27][65].
The most commonly studied
IL-4 polymorphism in RA was rs2243250 (-590 C/T; promoter region). The
IL-4 -590 T allele was found to be associated with RA susceptibility in Spanish and Chinese populations
[29][30][67,68]. In the study by Pawlik et al., the presence of the T allele of rs2243250 was correlated with the active form of RA and increased parameters of disease activity, including Disease Activity Score 28 (DAS28), ESR, and number of swollen and tender joints. However, an association between rs2243250 and RA predisposition was not observed
[31][69]. In line with these findings, another study conducted by Hussein et al. reported an association of the TT genotype of rs2243250 with erosive RA, presence of anti-cyclic citrullinated peptides (anti-CCP), and increased disease severity parameters. In addition, authors observed that the TT genotype was associated with susceptibility to RA
[32][70]. On the contrary, three other studies did not find significant relationships between the rs2243250 polymorphism and RA risk
[24][33][34][62,71,72]. However, the results from two meta-analyses confirmed that the T allele of the rs2243250 genetic variant was significantly associated with increased risk of RA development
[35][36][73,74].
In a multicohort candidate gene study investigating 8 SNPs within the
IL-4 gene, no associations were found in regard to joint damage in the course of RA
[37][75]. Some studies examined also rs79071878,
IL-4’s variable number of tandem repeats (VNTR; 70 bp; 3 intron). Genevay at al. reported that the presence of the rare
IL-4 VNTR (2) allele positively correlated with lower joint destruction in RA patients
[38][76]. The protective effect of the rare
IL-4 VNTR (2) allele was also observed with regard to joint destruction
[39][77]. Conversely, one study reported association of the
IL-4 VNTR (2) allele with RA risk
[33][71]. Although no significant association was detected between the
IL-4 VNTR polymorphism and RA susceptibility, nor with rheumatoid factor (RF) presence and disease severity
[30][68].
Several genetic studies also investigated polymorphisms within the
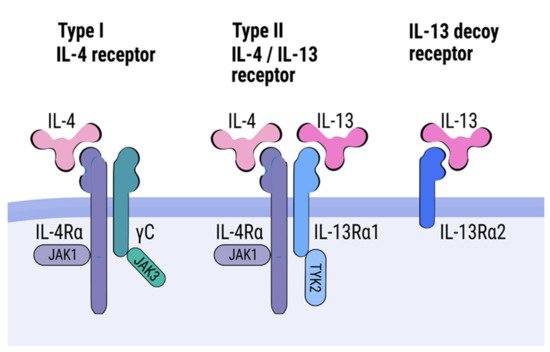
IL-4R gene: rs1805010 (+148 A/G; I50V; exon 5) and rs1801275 (+1902 A/G; Q551R; exon 12). They have important functional significance.
IL-4R I50V polymorphism is located in the extracellular domain and affects strength of interaction with IL-4, while
IL-4R Q551R variant is located in the intracellular domain and affects intracellular signaling. In the study by Prots et al. on rs1805010, the GG genotype (V50/V50) was found to be associated with bone erosion in RA patients
[40][78]. However, no relationship between the
IL-4R I50V polymorphism and RA development was detected
[40][78]. On the other hand, Marinou et al. did not find any association of this genetic variants with RA risk or disease severity
[24][62]. Discordant results were reported by Moreno et al., with the
IL-4R A allele (I50) being correlated with a presence of RF and a history of articular joint replacement
[30][68]. Meta-analysis performed by Peng et al. revealed that the G allele (V50) of the
IL-4R rs1805010 variant might be a risk factor for RA
[41][79]. Interesting results were obtained in the study by Wallis et al. investigating influence of the
IL-4R I50V polymorphism on Th17 production in cell culture experiments
[42][80]. The authors observed that IL-4 effectively inhibited IL-17 secretion by cells obtained from patients with the
IL-4R AA (I50/I50) or AG (I50/V50) genotypes, but it failed to suppress production of IL-17 in the case of the GG genotype (V50/V50)
[42][80].
No association was found between
IL-4R Q551R polymorphism and disease susceptibility or radiographic progression in RA patients
[30][68]. In line with these findings, the Q551R polymorphism was not associated with RA risk, nor joint damage progression, in three other studies
[24][38][39][62,76,77]. However, in another study a significant relationship between the Q551R G allele (R551) genetic variant and RF in RA patients was detected
[40][78]. No association was detected between the Q551R polymorphism and RA risk in meta-analysis performed by Peng et al.
[41][79]. Both the Q551R and I50V polymorphisms were also investigated in PsA patients. However, no significant associations were found with regard to PsA susceptibility or disease severity
[43][81].
In summary, the IL-13 rs1800925 C allele was associated with increased PsA risk; however, no association with RA susceptibility was detected. Additionally, the IL-13 rs20541 G and rs848 C alleles were found to correlate with PsA risk. The results regarding IL-4 rs2243250 are contradictory. However, most of the performed studies, including two meta-analyses, reported association of the IL-4 rs2243250 T allele with RA risk, as well as worse course of disease. On the other hand, a protective effect of the IL-4 VNTR (2) allele was found in context of RA, but two other studies did not confirm these results. The results regarding the rs1805010 polymorphism within the gene encoding IL-4R are not consistent, with some studies indicating a protective, and some a deleterious effect of the G allele on RA development. The second-most commonly studied IL-4R polymorphism, rs1801275, was not found to be associated with RA and PsA risk nor with RA disease course.
4. IL-4 and IL-13 Serum Concentrations in Inflammatory Arthritis
Isomaki et al. observed that IL-13 is consistently present in a synovial fluid (SF) of RA patients
[44][82]. In the study by Spadaro et al., serum levels of IL-13 were significantly higher in RA patients than in healthy individuals
[45][83]. However, the IL-13 serum concentrations did not differ between PsA patients and controls. On the other hand, increased levels of IL-13 in SF have been found in both RA and PsA patients, as compared to osteoarthritis control group
[45][83]. Upregulation of the IL-13 levels in serum was also observed in patients diagnosed with PsA in the study by Szodoray et al.
[46][84].
In addition, increased concentrations of IL-13 were observed in sera of early RA patients, as compared to healthy controls, in the study by Silosi et al. In this study, a positive correlation between the IL-13 serum levels and disease activity was also found
[47][85]. Higher IL-13 levels in serum of RA patients were also detected in other studies
[48][86]. In the study conducted by Tokayer et al. increased concentrations of IL-13 were observed in both serum and SF of RA patients
[49][87]. Additionally, elevated levels of IL-13 were found in SF of patients diagnosed with early RA
[50][88]. However, contradictory results were observed in the study by Azizieh et al. IL-13 levels did not differ from that of control group and no correlation was observed between IL-13 concentrations and disease activity
[51][89]. On the other hand, two research groups reported decreased IL-13 levels in both serum and SF of RA patients
[52][53][90,91].
IL-4 is expressed at relatively low levels in peripheral blood (PB) and SF
[54][55][56][92,93,94]. Increased mRNA levels of IL-4 in the whole blood of RA patients were reported in the study Kawashima et al.
[57][95]. At a protein level, IL-4 was found to be increased in mononuclear and whole blood cells from RA patients in response to in vitro stimulation
[58][59][96,97]. Enhanced IL-4 concentrations were also found in RA SF and plasma samples
[60][61][98,99]. In addition, Kokkonen et al. observed increased IL-4 levels in RA patients before disease development
[62][100]. Conversely, Constantin et al. reported downregulated expression of the
IL-4 gene in mononuclear cells obtained from RA patients as compared to healthy individuals
[54][92]. They also demonstrated negative correlation between
IL-4 gene expression and clinical parameters of the disease
[54][92]. In addition, Kramer et al. also observed that circulating levels of IL-4 were inversely correlated with disease activity in RA patients
[63][101]. On the other hand, IL-4 secretion by SF and PB CD4+ and CD8+ cells from patients with RA was investigated in the study by Isomaki et al. Expressions of IL-4 by CD4+ and CD8+ cells were comparable between PB and SF cells in this study
[64][102]. However, other study found that higher levels of IL-4 were secreted by CD8+ T cells derived from SF than from CD8+ T PB cells of RA patients
[65][103].
In conclusion, the results regarding the IL-4/IL-13 levels in patients diagnosed with inflammatory arthritis are somewhat contradictory. Some studies have reported increased serum and SF levels of IL-13 in patients diagnosed with RA or PsA. However, some studies have documented contrary findings. The results regarding IL-4 concentrations in patients with inflammatory arthritis are also not consistent. It is difficult to compare the results derived from these studies, since the IL-4/IL-13 levels were measured in different cell populations, conditions, and experimental protocols. One of the most important aspect that should be considered regarding these results is disease duration. Three of the aforementioned studies examined patients with early RA and reported significantly elevated levels of IL-4/IL-13
[47][50][62][85,88,100]. Notably, one of these studies documented enhanced IL-4/IL-13 levels present in patients with early inflammatory arthritis, but no longer detected in patients with established RA
[50][88]. These results suggest that cytokines profile of early arthritis patients is transient and differs from cytokines profile characterizing patients with an established RA. In line with this hypothesis, the IL-4/IL-13 cytokines might exert a diverse influence depending on the disease status. It is conceivable that these cytokines might be involved in a pathogenesis of inflammatory arthritis in a time-dependent manner, i.e., having an activatory influence at the disease’s onset and an inhibitory effect when the disease is established.