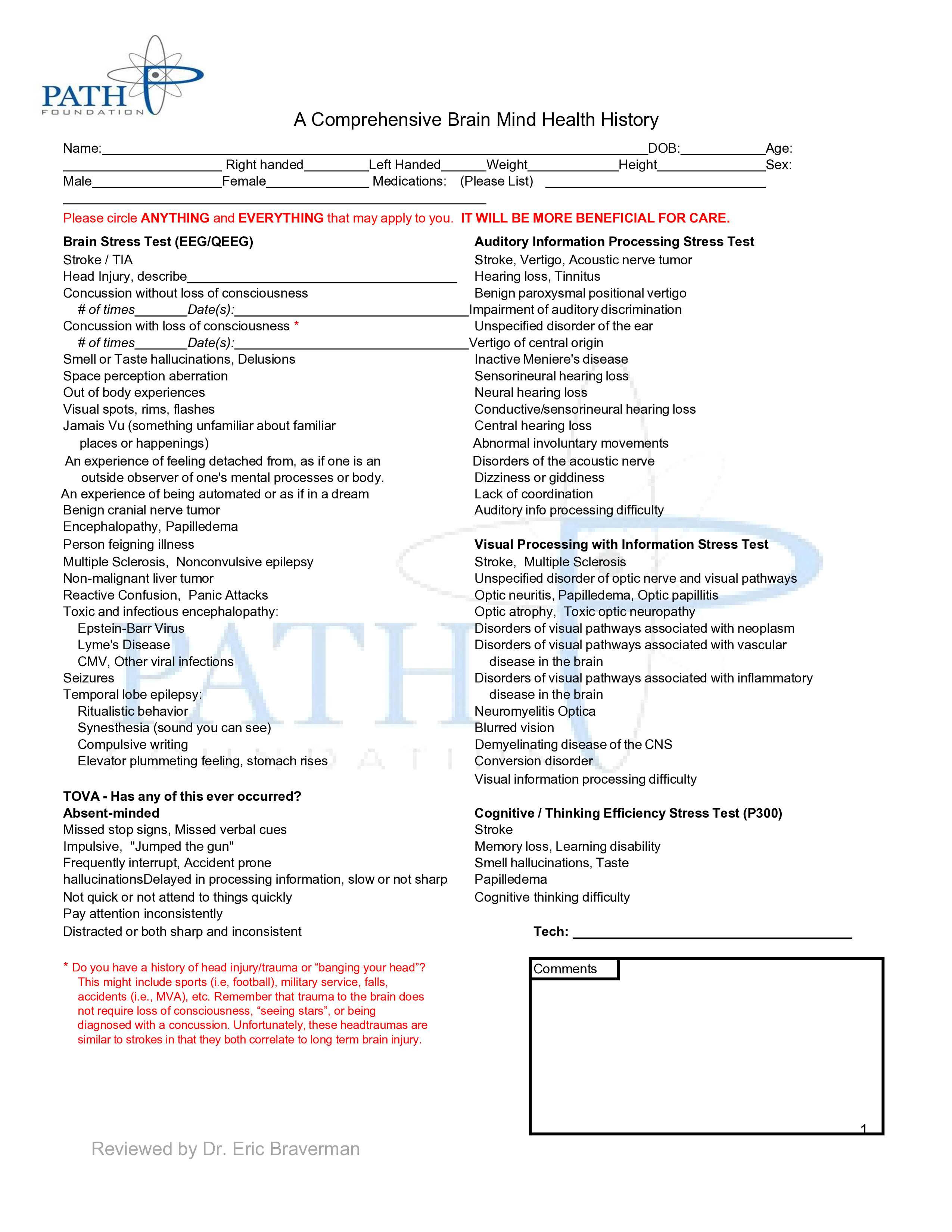
In the outpatient general practice setting, most practitioners do not have the time or resources to acquire a comprehensive history pertaining to patients' brain and mental health. This comprehensive brain-mind health history gives health care providers a simple and easy-to-use checklist, which can be filled out by patients before their appointment and/or while sitting in the waiting room. This will allow practitioners to have a more thorough and detailed history of their patients on hand, which they can quickly skim through as needed. In addition, it will help practitioners introduce and subsequently discuss more sensitive topics with their patients that are often associated with stigmas, such as substance use, mental health issues, etc. Ultimately, this comprehensive history will allow health care practitioners to make better decisions on behalf of their patients.
- Memory
- Attention
- Neuropsychiatric
- ADHD
- Concussion
- Head Trauma
- Neurotransmitters
- Comprehensive Brain Mind Health History
- Mood
- Insurance Codes
A Brain Health Check-Up
Cognitive impairment is an extremely common public health issue that is all too often overlooked. When discussing cognitive impairment most primary care physicians all agree that assessments of cognitive function are valuable tools and vital to patient welfare. However, only about 16% of adults over the age of 65 receive regular routine cognitive assessments, which is dramatically less than other preventive screening tests such as, blood pressure (91%), cholesterol (83%), and diabetes (66%)[1]. Furthermore, the majority of patients who do receive regular cognitive assessments are typically above the age of 50, but cognitive dysfunction can be seen in all ages including the young.
 Psychiatric illness is one of the most prevalent causes of cognitive impairment in those under 50. In 2019 approximately 51.5 million adults (age 18 or older) in the United States suffered from mental illness and the highest prevalence rate was seen in young adults (age 18-25)[2]. Routine cognitive assessments would be a valuable tool in identifying and beginning the management of mental illnesses earlier, which would, in turn, provide these individuals with a better quality of life. However, screening for any form of Mild Cognitive Impairment (MCI) isn’t very common in general and even less so in those under 50. This further exemplifies the under usage of an important health assessment tool and identifies an area of improvement that is desperately needed within our health care system.
Psychiatric illness is one of the most prevalent causes of cognitive impairment in those under 50. In 2019 approximately 51.5 million adults (age 18 or older) in the United States suffered from mental illness and the highest prevalence rate was seen in young adults (age 18-25)[2]. Routine cognitive assessments would be a valuable tool in identifying and beginning the management of mental illnesses earlier, which would, in turn, provide these individuals with a better quality of life. However, screening for any form of Mild Cognitive Impairment (MCI) isn’t very common in general and even less so in those under 50. This further exemplifies the under usage of an important health assessment tool and identifies an area of improvement that is desperately needed within our health care system.
In addition, another challenge that health care providers can face is that patients can be reluctant to discuss any perceived changes in their cognitive function, including memory, attention, confusion, etc. According to the Center for Disease Control’s (CDC) Healthy Aging Data (2015-2019), on average less than half of adults aged 50 years and older with subjective cognitive decline (SCD) reported discussing noticed changes in their cognitive function with a health care professional[3]. A streamlined screening test would not only give health care professionals an opportunity to open a dialogue with their patients, but it would also allow for the identification and subsequent discussion of cognitive impairments without embarrassment.
One solution to this problem would be to implement in the United States (US) an annual routine brain health checkup exam, for all ages, in every aspect of health care. This would not only allow health professionals to identify and diagnose cognitive impairment earlier, but it would also help establish a baseline for their patients in terms of cognitive function. The best comparison of a patient’s cognitive function is to themselves while in a healthy state, so knowing a patient’s baseline cognitive function would provide physicians with invaluable information. With an established baseline and routine brain health checkups, physicians would be able to detect changes in cognitive function much quicker, which would allow them to diagnose and start treatments sooner. Finally, an annual brain health checkup exam would help prevent further deterioration of the mind in the general population, while saving the country millions in related health care costs each year.
This paper includes several detailed checklists, involving brain-mind health, that could be used routinely in an outpatient primary care setting. This would allow primary care physicians to obtain a more thorough and detailed history of their patients in a very efficient manner and subsequently provide better care for their patients.
A Comprehensive Brain Mind Health History
A combined, comprehensive, one-page brain-mind health history is included below. This would provide practitioners with a short and simple document that patients could fill out prior to their appointment whether at home or in the waiting room. This would ensure providers that they had a very thorough detailed history of their patient, which they could quickly read through before seeing the patient or while talking to them. In addition, this helps the patient recall issues they might have otherwise forgotten, or thought was not medically relevant. This would also help providers address more sensitive topics or issues that are often associated with stigmas, such as substance use, mental health issues, etc. Overall, it helps practitioners provide the best possible care for patients.
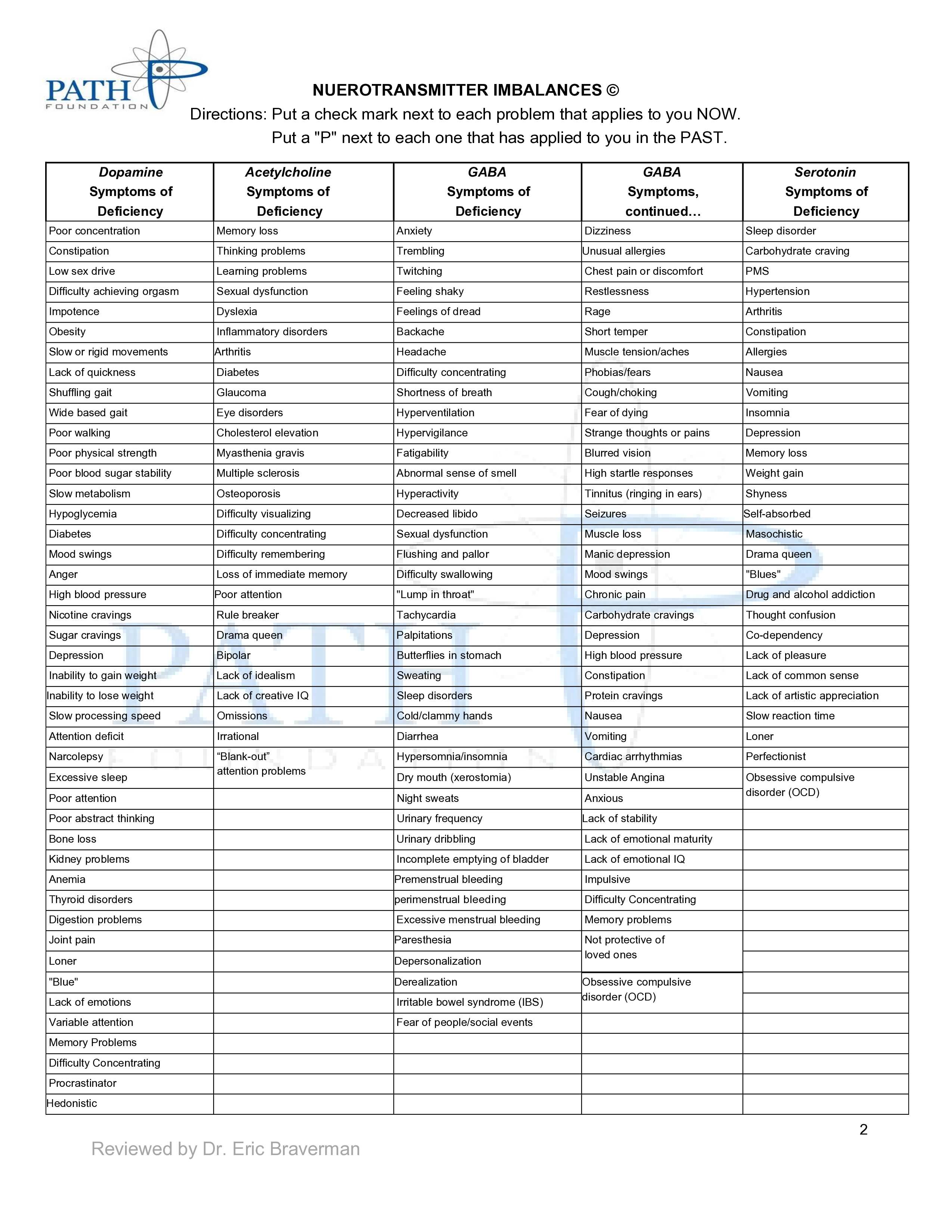
Neurotransmitter Imbalances©
Neurotransmitters are the origin of brain bioelectricity. There are four core families of neurotransmitter systems including, dopamine/catecholamines, acetylcholine, GABA/glutamate, and serotonin. When these neurotransmitters are not balanced, they can cause significant and persistent brain-mind health disturbances. The Neurotransmitter imbalances checklist below lists common symptoms associated with specific neurotransmitter deficiencies. This allows patients to better understand at the chemical level why they are experiencing certain symptoms/disorders and allows treatment to be tailored towards their specific needs. In addition, the checklist offers further value because even individuals who are not seriously ill often have areas within their life that they can or want to improve upon and this list provides them the means to do so. Therefore, the neurotransmitter imbalances checklist not only helps guide health providers in the treatment of memory, attention, and neuropsychiatric problems but also enables individuals to improve upon themselves and their daily life.
Directions: Put a checkmark next to each problem that applies to you NOW. Put a "P" next to each one that has applied to you in the PAST.
|
Dopamine Symptoms of Deficiency |
Acetylcholine Symptoms of Deficiency |
GABA Symptoms of Deficiency |
GABA Symptoms continued… |
Serotonin Symptoms of Deficiency |
|
Poor concentration |
Memory loss |
Anxiety |
Dizziness |
Sleep disorder |
|
Constipation |
Thinking problems |
Trembling |
Unusual allergies |
Carbohydrate craving |
|
Low sex drive |
Learning problems |
Twitching |
Chest pain or discomfort |
PMS |
|
Difficulty achieving orgasm |
Sexual dysfunction |
Feeling shaky |
Restlessness |
Hypertension |
|
Impotence |
Dyslexia |
Feelings of dread |
Rage |
Arthritis |
|
Obesity |
Inflammatory disorders |
Backache |
Short temper |
Constipation |
|
Slow or rigid movements |
Arthritis |
Headache |
Muscle tension/aches |
Allergies |
|
Lack of quickness |
Diabetes |
Difficulty concentrating |
Phobias/fears |
Nausea |
|
Shuffling gait |
Glaucoma |
Shortness of breath |
Cough/choking |
Vomiting |
|
Wide based gait |
Eye disorders |
Hyperventilation |
Fear of dying |
Insomnia |
|
Poor walking |
Cholesterol elevation |
Hypervigilance |
Strange thoughts or pains |
Depression |
|
Poor physical strength |
Myasthenia gravis |
Fatigability |
Blurred vision |
Memory loss |
|
Poor blood sugar stability |
Multiple sclerosis |
Abnormal sense of smell |
High startle responses |
Weight gain |
|
Slow metabolism |
Osteoporosis |
Hyperactivity |
Tinnitus (ringing in ears) |
Shyness |
|
Hypoglycemia |
Difficulty visualizing |
Decreased libido |
Seizures |
Self-absorbed |
|
Diabetes |
Difficulty concentrating |
Sexual dysfunction |
Muscle loss |
Masochistic |
|
Mood swings |
Difficulty remembering |
Flushing and pallor |
Manic depression |
Drama queen |
|
Anger |
Loss of immediate memory |
Difficulty swallowing |
Mood swings |
"Blues" |
|
High blood pressure |
Poor attention |
"Lump in throat" |
Chronic pain |
Drug and alcohol addiction |
|
Nicotine cravings |
Rulebreaker |
Tachycardia |
Carbohydrate cravings |
Thought confusion |
|
Sugar cravings |
Drama queen |
Palpitations |
Depression |
Co-dependency |
|
Depression |
Bipolar |
Butterflies in stomach |
High blood pressure |
Lack of pleasure |
|
Inability to gain weight |
Lack of idealism |
Sweating |
Constipation |
Lack of common sense |
|
Inability to lose weight |
Lack of creative IQ |
Sleep disorders |
Protein cravings |
Lack of artistic appreciation |
|
Slow processing speed |
Omissions |
Cold/clammy hands |
Nausea |
Slow reaction time |
|
Attention-deficit |
Irrational |
Diarrhea |
Vomiting |
Loner |
|
Narcolepsy |
“Blank-out” attention problems |
Hypersomnia/insomnia |
Cardiac arrhythmias |
Perfectionist |
|
Excessive sleep |
Dry mouth (xerostomia) |
Unstable Angina |
Obsessive-compulsive disorder (OCD) |
|
|
Poor attention |
Night sweats |
Anxious |
||
|
Poor abstract thinking |
Urinary frequency |
Lack of stability |
||
|
Bone loss |
Urinary dribbling |
Lack of emotional maturity |
||
|
Kidney problems |
Incomplete emptying of the bladder |
Lack of emotional IQ |
||
|
Anemia |
Premenstrual bleeding |
Impulsive |
||
|
Thyroid disorders |
perimenstrual bleeding |
Difficulty Concentrating |
||
|
Digestion problems |
Excessive menstrual bleeding |
Memory problems |
||
|
Joint pain |
Paresthesia |
Not protective of loved ones |
||
|
Loner |
Depersonalization |
|||
|
"Blue" |
Derealization |
Obsessive compulsive disorder (OCD) |
||
|
Lack of emotions |
Irritable bowel syndrome (IBS) |
|||
|
Variable attention |
Fear of people/social events |
|||
|
Memory Problems |
||||
|
Difficulty Concentrating |
||||
|
Procrastinator |
||||
|
Hedonistic |
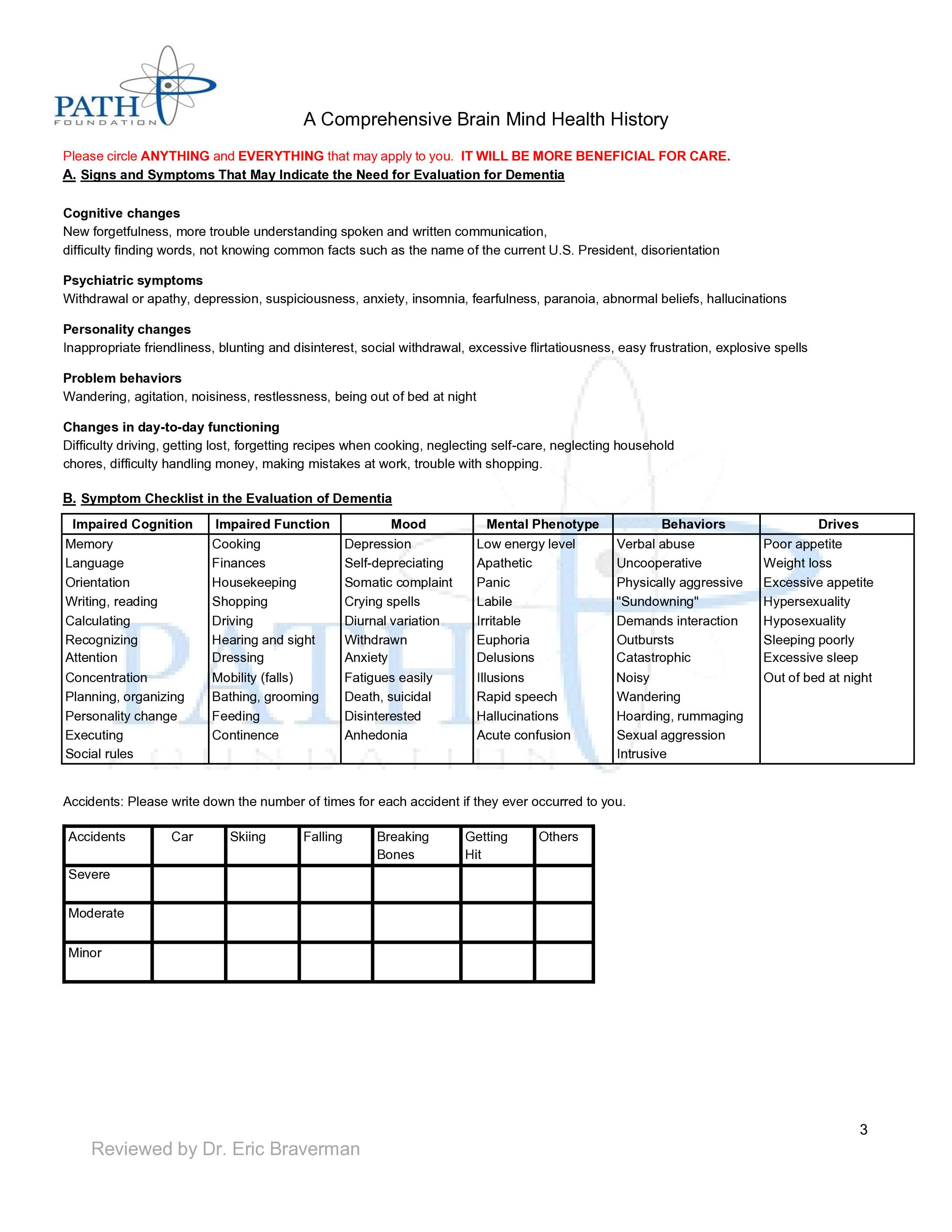
Dementia
Approximately more than 55 million individuals worldwide suffer from dementia[4]. Within the US approximately 5.8 million individuals suffer from Alzheimer’s disease and other related dementias[5]. Alzheimer's disease accounts for ~60% to 70% of dementia cases[6]. Common early symptoms of dementia include short-term memory loss, repetition, getting lost, difficulties tracking bills, problems with cooking especially new or complicated meals, forgetting to take medication, and word-finding problems[7][4]. Despite the high prevalence of dementia routine screening is typically not done in the majority of the population. This may be further exacerbated by the fact that patients with dementia can have poor insight into their own cognitive function and/or they are embarrassed about their situation. The following checklist relating to dementia allows providers to discuss these issues with their patients in a nonjudgmental way and helps to destigmatize dementia and raise awareness.
Signs and Symptoms That May Indicate the Need for Evaluation for Dementia
- Cognitive changes:
New forgetfulness, more trouble understanding spoken and written communication, difficulty finding words, disorientation, not knowing common facts, i.e., name of the current U.S. President
- Psychiatric symptoms:
Withdrawal/apathy, depression, suspiciousness, anxiety, insomnia, fearfulness, paranoia, abnormal beliefs, hallucinations
- Personality changes:
Inappropriate friendliness, blunting and disinterest, social withdrawal, excessive flirtatiousness, easily frustrated, explosive spells
- Problem behaviors:
Wandering, agitation, noisiness, restlessness, being out of bed at night
- Changes in day-to-day functioning:
Difficulty driving, getting lost, forgetting recipes when cooking, neglecting self-care, neglecting household chores, difficulty handling money, making mistakes at work, trouble with shopping
Symptom Checklist in the Evaluation of Dementia
|
Impaired Cognition |
Impaired Function |
Mood |
Mental Phenotype |
Behaviors |
Drives |
|
Memory |
Cooking |
Depression |
Low energy level |
Verbal abuse |
Poor appetite |
|
Language |
Finances |
Self-deprecating |
Apathetic |
Uncooperative |
Weight loss |
|
Orientation |
Housekeeping |
Somatic complaint |
Panic |
Physically aggressive |
Excessive appetite |
|
Writing, reading |
Shopping |
Crying spells |
Labile |
"Sundowning" |
Hypersexuality |
|
Calculating |
Driving |
Diurnal variation |
Irritable |
Demands interaction |
Hyposexuality |
|
Recognizing Attention |
Hearing and sight Dressing |
Withdrawn Anxiety |
Euphoria Delusions |
Outbursts Catastrophic |
Sleeping poorly Excessive sleep |
|
Concentration |
Mobility (falls) |
Fatigues easily |
Illusions |
Noisy |
Out of bed at night |
|
Planning, organizing |
Bathing, grooming |
Death, suicidal |
Rapid speech |
Wandering |
|
|
Personality change |
Feeding |
Disinterested |
Hallucinations |
Hoarding, rummaging |
|
|
Executing |
Continence |
Anhedonia |
Acute confusion |
Sexual aggression |
|
|
Social rules |
Intrusive |
Accidents: Please write down the number of times for each accident if they ever occurred to you.
|
Accidents |
Car |
Skiing |
Falling |
Breaking Bones |
Getting Hit |
Others |
|
Severe |
||||||
|
Moderate |
||||||
|
Minor |
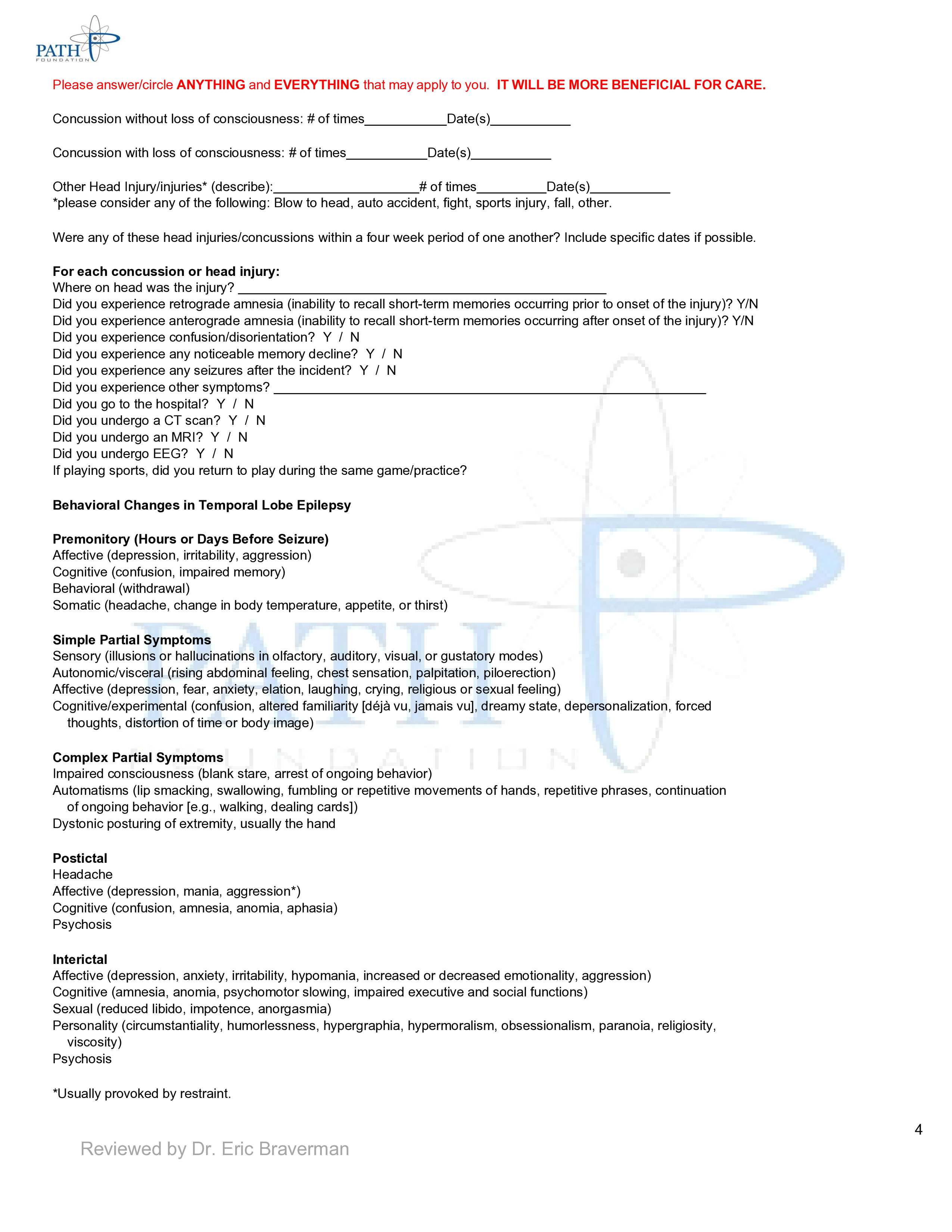
Traumatic Brain Injury/Concussion
According to the Centers for Disease Control and Prevention, approximately 1.5 million Americans sustain a Traumatic Brain Injury (TBI) annually[8]. It is also considered to be one of the leading causes of disability and death within the pediatric population (26 years of age and younger). Injuries of this nature can have serious short-term and long-term effects on individuals, their families, and society. Short-term consequences may include headache, dizziness, fatigue, nausea, vomiting, blurred vision, temporary loss of consciousness, etc. Long-term consequences may involve problems with memory, concentration, verbal communication, impulse control, sleep, etc. In addition, patients may exhibit personality changes or suffer psychological problems, such as depression, suicidal ideation, etc. Despite the prevalence and devastating effects associated with these injuries most physicians do not routinely screen or ask patients during clinical interview about previous head trauma/concussions/TBIs. Therefore, a thorough, repetitive (concussion/TBI histories that are filled out repeatedly at intervals, often leads to better recall and more honest answers), and multipage concussion/head injury questionnaire was created and included below.
|
Please answer/circle ANYTHING and EVERYTHING that may apply to you. IT WILL BE MORE BENEFICIAL FOR CARE. |
|
Concussion without loss of consciousness: # of times Date(s) |
|
Concussion with loss of consciousness: # of times Date(s) |
|
Other Head Injury/injuries* (describe): # of times Date(s) |
|
*Please consider any of the following: Blow to head, auto accident, fight, sports injury, fall, other. |
|
Were any of these head injuries/concussions within a four-week period of one another? Include specific dates if possible. |
|
For each concussion or head injury: |
|
Where on the head was the injury? |
|
Did you experience retrograde amnesia (inability to recall short-term memories occurring prior to onset of the injury)? Y/N |
|
Did you experience anterograde amnesia (inability to recall short-term memories occurring after onset of the injury)? Y/N |
|
Did you experience confusion/disorientation? Y / N |
|
Did you experience any noticeable memory decline? Y / N |
|
Did you experience any seizures after the incident? Y / N |
|
Did you experience other symptoms? |
|
Did you go to the hospital? Y / N |
|
Did you undergo a CT scan? Y / N |
|
Did you undergo an MRI? Y / N |
|
Did you undergo EEG? Y / N |
|
If playing sports, did you return to play during the same game/practice? |
|
Behavioral Changes in Temporal Lobe Epilepsy |
|
Premonitory (Hours or Days Before Seizure) |
|
Affective (depression, irritability, aggression) |
|
Cognitive (confusion, impaired memory) |
|
Behavioral (withdrawal) |
|
Somatic (headache, change in body temperature, appetite, or thirst) |
|
Simple Partial Symptoms |
|
Sensory (illusions or hallucinations in olfactory, auditory, visual, or gustatory modes) |
|
Autonomic/visceral (rising abdominal feeling, chest sensation, palpitation, piloerection) |
|
Affective (depression, fear, anxiety, elation, laughing, crying, religious or sexual feeling) |
|
Cognitive/experimental (confusion, altered familiarity [déjà vu, jamais vu], dreamy state, depersonalization, forced |
|
thoughts, distortion of time or body image) |
|
Complex Partial Symptoms |
|
Impaired consciousness (blank stare, arrest of ongoing behavior) |
|
Automatisms (lip-smacking, swallowing, fumbling or repetitive movements of hands, repetitive phrases, continuation |
|
of ongoing behavior [e.g., walking, dealing cards]) |
|
Dystonic posturing of extremity, usually the hand |
|
Postictal |
|
Headache |
|
Affective (depression, mania, aggression*) |
|
Cognitive (confusion, amnesia, anomia, aphasia) |
|
Psychosis |
|
Interictal |
|
Affective (depression, anxiety, irritability, hypomania, increased or decreased emotionality, aggression) |
|
Cognitive (amnesia, anomia, psychomotor slowing, impaired executive and social functions) |
|
Sexual (reduced libido, impotence, anorgasmia) |
|
Personality (circumstantiality, humorlessness, hypergraphia, hypermoralism, obsessionalism, paranoia, religiosity, |
|
viscosity) |
|
Psychosis |
|
*Usually provoked by restraint. |
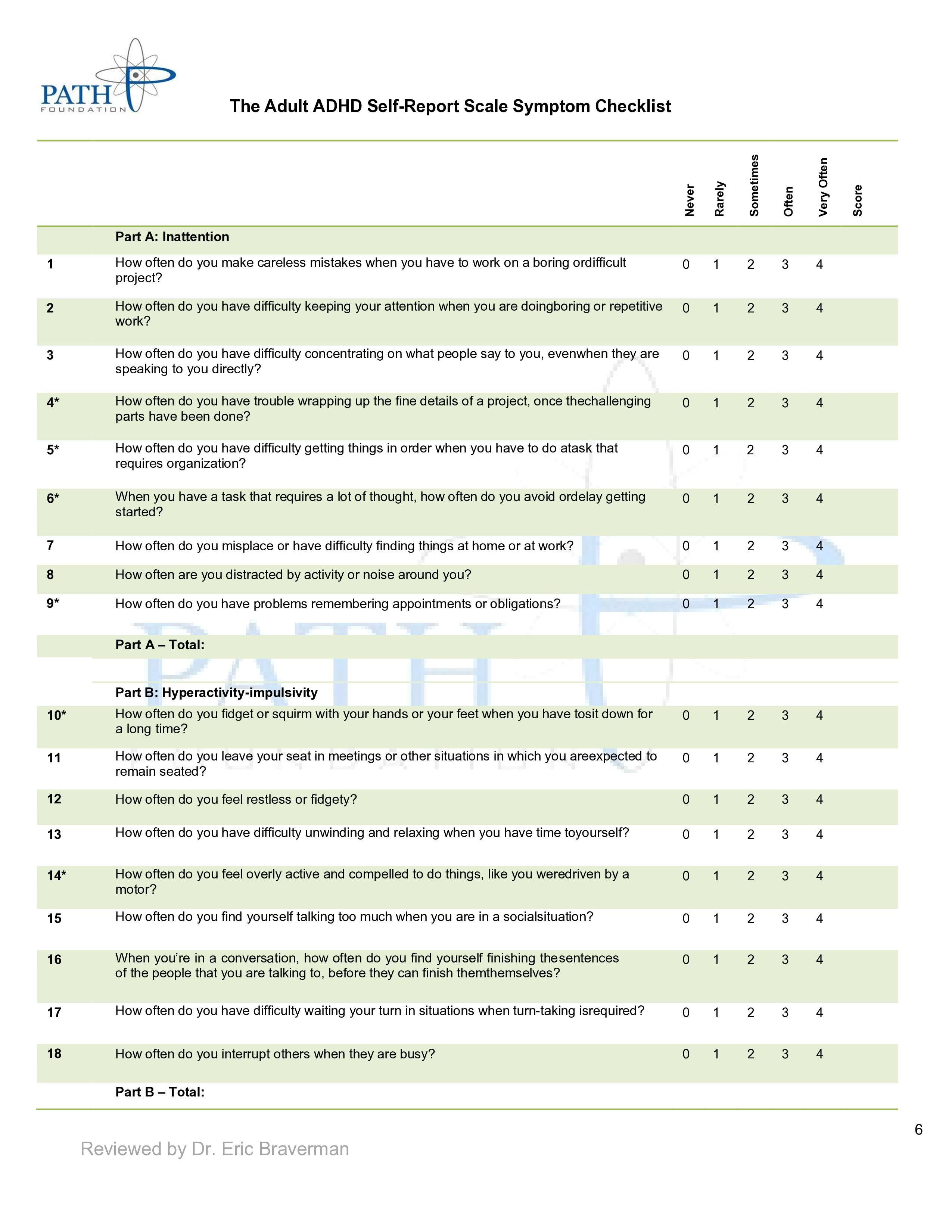
Adult Attention Deficit Hyperactivity Disorder
Attention Deficit Hyperactivity Disorder (ADHD) is one of the most common neurodevelopmental disorders that affect children. According to the CDC approximately 6.1 million children (age 5-17)[9], in the United States (US), are affected. Usually, it is diagnosed during childhood, however, sometimes individuals aren’t properly diagnosed until adulthood. Some typical types of symptoms of ADHD include impulsiveness, disorganization, difficulty concentrating, mood swings, low frustration tolerance, restlessness, trouble multitasking, etc. ADHD can persist throughout adulthood and can cause problems for individuals at home, work, or with relationships. Therefore, it is imperative to properly diagnose ADHD early. So, a more thorough questionnaire designed to diagnose ADHD in adults was created and included down below.
The Adult ADHD Self-Report Scale Symptom Checklist
|
Never |
Rarely |
Sometimes |
Often |
Very Often |
Score |
||
|
Part A: Inattention |
|||||||
|
1 |
How often do you make careless mistakes when you have to work on a boring or difficult project? |
0 |
1 |
2 |
3 |
4 |
|
|
2 |
How often do you have difficulty keeping your attention when you are doing boring or repetitive work? |
0 |
1 |
2 |
3 |
4 |
|
|
3 |
How often do you have difficulty concentrating on what people say to you, even when they are speaking to you directly? |
0 |
1 |
2 |
3 |
4 |
|
|
4* |
How often do you have trouble wrapping up the fine details of a project, once the challenging parts have been done? |
0 |
1 |
2 |
3 |
4 |
|
|
5* |
How often do you have difficulty getting things in order when you have to do a task that requires organization? |
0 |
1 |
2 |
3 |
4 |
|
|
6* |
When you have a task that requires a lot of thought, how often do you avoid or delay getting started? |
0 |
1 |
2 |
3 |
4 |
|
|
7 |
How often do you misplace or have difficulty finding things at home or at work? |
0 |
1 |
2 |
3 |
4 |
|
|
8 |
How often are you distracted by activity or noise around you? |
0 |
1 |
2 |
3 |
4 |
|
|
9* |
How often do you have problems remembering appointments or obligations? |
0 |
1 |
2 |
3 |
4 |
|
|
Part A – Total: |
|||||||
|
Part B: Hyperactivity-impulsivity |
|||||||
|
10* |
How often do you fidget or squirm with your hands or your feet when you have to sit down for a long time? |
0 |
1 |
2 |
3 |
4 |
|
|
11 |
How often do you leave your seat in meetings or other situations in which you are expected to remain seated? |
0 |
1 |
2 |
3 |
4 |
|
|
12 |
How often do you feel restless or fidgety? |
0 |
1 |
2 |
3 |
4 |
|
|
13 |
How often do you have difficulty unwinding and relaxing when you have time to yourself? |
0 |
1 |
2 |
3 |
4 |
|
|
14* |
How often do you feel overly active and compelled to do things, like you were driven by a motor? |
0 |
1 |
2 |
3 |
4 |
|
|
15 |
How often do you find yourself talking too much when you are in a social situation? |
0 |
1 |
2 |
3 |
4 |
|
|
16 |
When you’re in a conversation, how often do you find yourself finishing the sentences of the people that you are talking to before they can finish them themselves? |
0 |
1 |
2 |
3 |
4 |
|
|
17 |
How often do you have difficulty waiting your turn in situations when turn-taking is required? |
0 |
1 |
2 |
3 |
4 |
|
|
18 |
How often do you interrupt others when they are busy? |
0 |
1 |
2 |
3 |
4 |
|
|
Part B – Total: |
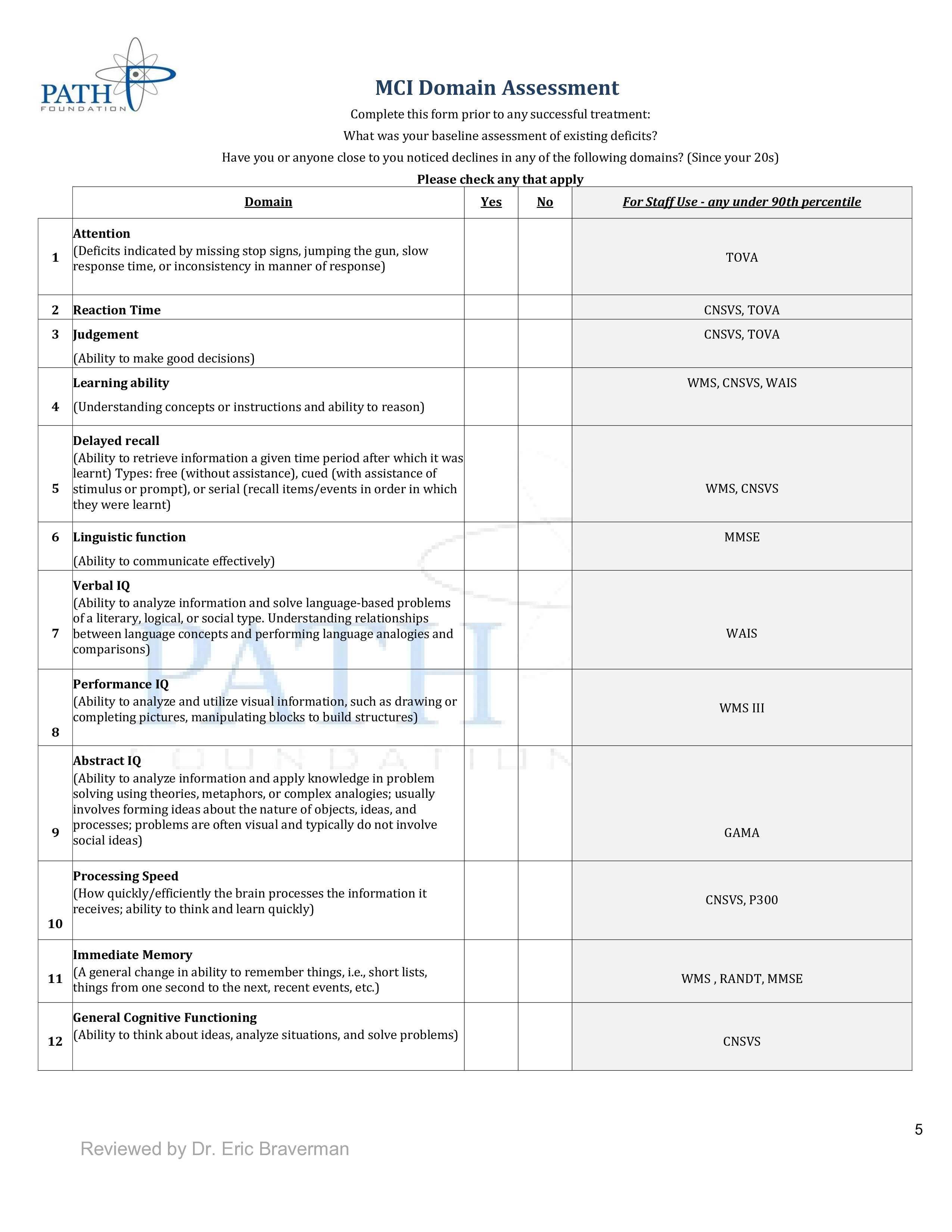
Mild Cognitive Domain Assessment
Subjective checklists can be useful in diagnosing/screening for certain disorders; however, they are not always the most accurate. Patients can be unreliable due to lack of awareness, poor historians, neuropsychiatric disturbances, denial, intentional lying, etc. Therefore, tests that provide objective measurements are also needed to evaluate brain health. Objective measures of a direct brain injury are necessary because they can confirm the severity of head trauma, concussion, cognitive impairment, neuropsychiatric disorders, medical comorbidities, etc. The MCI Domain Assessment below combines subjective and objective testing. It includes a simple subjective checklist that allows health providers to screen patients for deficits in certain domains i.e., memory, attention, judgement, IQ, etc. If a deficit is reported in one of these categories then the provider can look into the last column to see what possible objective assessments can be used to investigate the deficit further. By identifying these deficits/Mild Cognitive Impairment (MCI) earlier providers can prevent, slow, and sometimes reverse brain injury.
There are several objective assessments listed within the MCI Domain Assessment. The Central Nervous System Vital Signs (CNSVS), is a computerized assessment that evaluates memory, attention, simple motor performance, and executive functions. The Test of Variables of Attention (TOVA), is a computerized assessment that evaluates an individual's attention while screening for ADHD. Wechsler Memory Scale (WMS) is a neuropsychological test designed to measure different types of memory functions. Wechsler Adult Intelligence Scale (WAIS) is an IQ test that evaluates intelligence and cognitive ability in older adolescents and adults. Mini-Mental State Exam (MMSE) assesses cognitive function including tests of memory, attention, orientation, language, and visual-spatial skills. General Ability Measure for Adults (GAMA) is a brief assessment that evaluates a person's intellectual ability. Electroencephalography (EEG/P300) is an electrophysiological monitoring method designed to record the brain’s electrical activity. In particular, the P300 wave is an event-related potential that quantifies synaptic speed during an EEG and these measurements are like a stress test of the brain.
MCI Domain Assessment
Complete this form prior to any successful treatment:
What was your baseline assessment of existing deficits?
Have you or anyone close to you noticed declines in any of the following domains? (Since your 20s)
Please check any that apply
|
Domain |
Yes |
No |
For Staff Use - Possible Assessments |
|
|
1 |
Attention (Deficits indicated by missing stop signs, jumping the gun, slow response time, or inconsistency in the manner of response) |
TOVA |
||
|
2 |
Reaction Time |
CNSVS, TOVA |
||
|
3 |
Judgment (Ability to make good decisions) |
CNSVS, TOVA |
||
|
4 |
Learning ability (Understanding concepts or instructions and ability to reason) |
WMS, CNSVS, WAIS |
||
|
5 |
Delayed recall (Ability to retrieve information a given time period after which it was learned) Types: free (without assistance), cued (with assistance of stimulus or prompt), or serial (recall items/events in order in which they were learned) |
WMS, CNSVS |
||
|
6 |
Linguistic function (Ability to communicate effectively) |
MMSE |
||
|
7 |
Verbal IQ (Ability to analyze information and solve language-based problems of a literary, logical, or social type. Understanding relationships between language concepts and performing language analogies and comparisons) |
WAIS |
||
|
8 |
Performance IQ (Ability to analyze and utilize visual information, such as drawing or completing pictures, manipulating blocks to build structures) |
WMS III |
||
|
9 |
Abstract IQ (Ability to analyze information and apply knowledge in problem-solving using theories, metaphors, or complex analogies; usually involves forming ideas about the nature of objects, ideas, and processes; problems are often visual and typically do not involve social ideas) |
GAMA |
||
|
10 |
Processing Speed (How quickly/efficiently the brain processes the information it receives; ability to think and learn quickly) |
CNSVS, EEG (P300) |
||
|
11 |
Immediate Memory (A general change in ability to remember things, i.e., shortlists, things from one second to the next, recent events, etc.) |
WMS, MMSE |
||
|
12 |
General Cognitive Functioning (Ability to think about ideas, analyze situations, and solve problems) |
CNSVS |
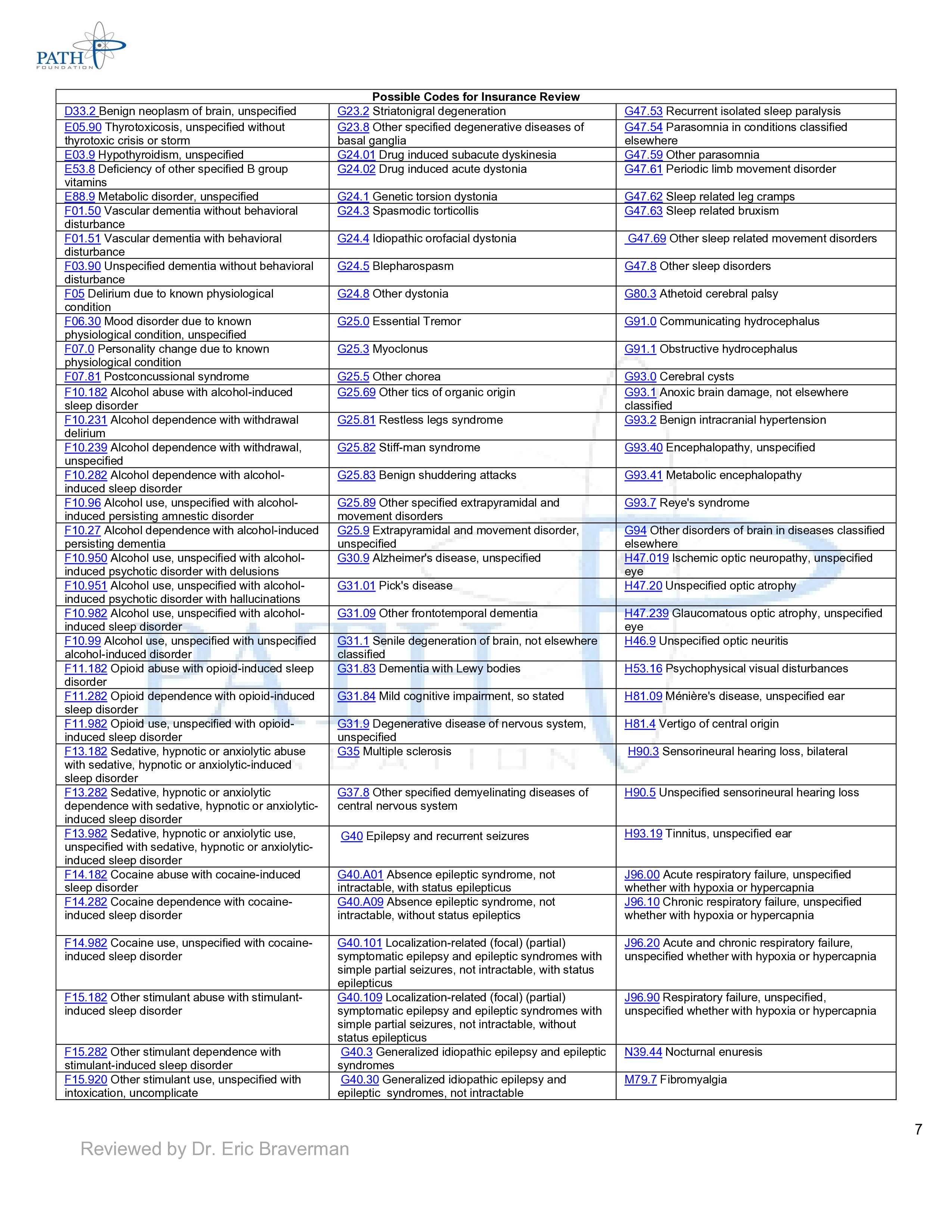
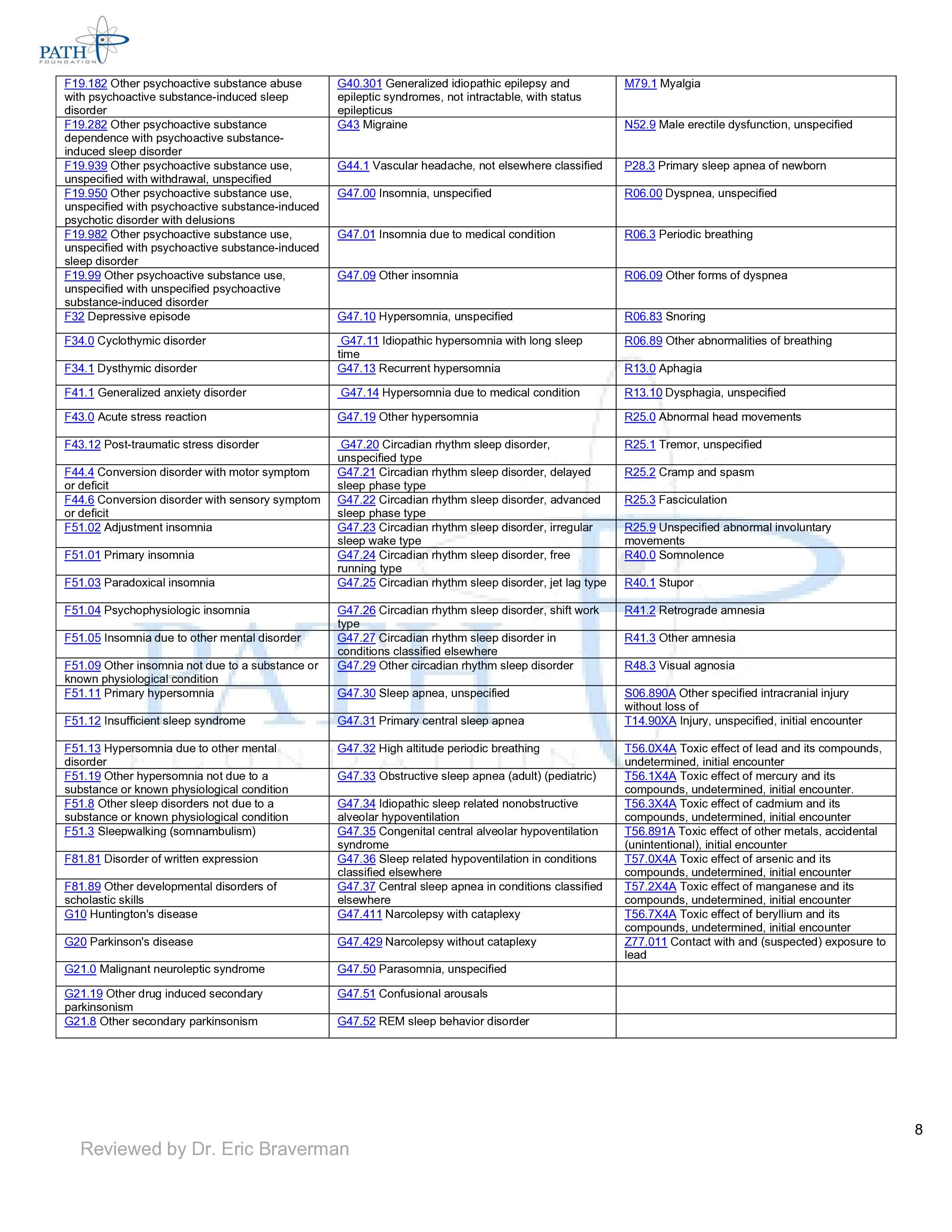
International Classification of Disease (ICD)-10 Codes
Below is a condensed list of common insurance codes for various neurological, psychiatric, and medical conditions.
|
Possible Codes for Insurance Review |
||
|
D33.2 Benign neoplasm of brain, unspecified |
G23.2 Striatonigral degeneration |
G47.53 Recurrent isolated sleep paralysis |
|
E05.90 Thyrotoxicosis, unspecified without thyrotoxic crisis or storm |
G23.8 Other specified degenerative diseases of basal ganglia |
G47.54 Parasomnia in conditions classified elsewhere |
|
E03.9 Hypothyroidism, unspecified |
G24.01 Drug induced subacute dyskinesia |
G47.59 Other parasomnia |
|
E53.8 Deficiency of other specified B group vitamins |
G24.02 Drug induced acute dystonia |
G47.61 Periodic limb movement disorder |
|
E88.9 Metabolic disorder, unspecified |
G24.1 Genetic torsion dystonia |
G47.62 Sleep related leg cramps |
|
F01.50 Vascular dementia without behavioral disturbance |
G24.3 Spasmodic torticollis |
G47.63 Sleep related bruxism |
|
F01.51 Vascular dementia with behavioral disturbance |
G24.4 Idiopathic orofacial dystonia |
G47.69 Other sleep related movement disorders |
|
F03.90 Unspecified dementia without behavioral disturbance |
G24.5 Blepharospasm |
G47.8 Other sleep disorders |
|
F05 Delirium due to known physiological condition |
G24.8 Other dystonia |
G80.3 Athetoid cerebral palsy |
|
F06.30 Mood disorder due to known physiological condition, unspecified |
G25.0 Essential Tremor |
G91.0 Communicating hydrocephalus |
|
F07.0 Personality change due to known physiological condition |
G25.3 Myoclonus |
G91.1 Obstructive hydrocephalus |
|
F07.81 Postconcussional syndrome |
G25.5 Other chorea |
G93.0 Cerebral cysts |
|
F10.182 Alcohol abuse with alcohol-induced sleep disorder |
G25.69 Other tics of organic origin |
G93.1 Anoxic brain damage, not elsewhere classified |
|
F10.231 Alcohol dependence with withdrawal delirium |
G25.81 Restless legs syndrome |
G93.2 Benign intracranial hypertension |
|
F10.239 Alcohol dependence with withdrawal, unspecified |
G25.82 Stiff-man syndrome |
G93.40 Encephalopathy, unspecified |
|
F10.282 Alcohol dependence with alcohol-induced sleep disorder |
G25.83 Benign shuddering attacks |
G93.41 Metabolic encephalopathy |
|
F10.96 Alcohol use, unspecified with alcohol-induced persisting amnestic disorder |
G25.89 Other specified extrapyramidal and movement disorders |
G93.7 Reye's syndrome |
|
F10.27 Alcohol dependence with alcohol-induced persisting dementia |
G25.9 Extrapyramidal and movement disorder, unspecified |
G94 Other disorders of brain in diseases classified elsewhere |
|
F10.950 Alcohol use, unspecified with alcohol-induced psychotic disorder with delusions |
G30.9 Alzheimer's disease, unspecified |
H47.019 Ischemic optic neuropathy, unspecified eye |
|
F10.951 Alcohol use, unspecified with alcohol-induced psychotic disorder with hallucinations |
G31.01 Pick's disease |
H47.20 Unspecified optic atrophy |
|
F10.982 Alcohol use, unspecified with alcohol-induced sleep disorder |
G31.09 Other frontotemporal dementia |
H47.239 Glaucomatous optic atrophy, unspecified eye |
|
F10.99 Alcohol use, unspecified with unspecified alcohol-induced disorder |
G31.1 Senile degeneration of brain, not elsewhere classified |
H46.9 Unspecified optic neuritis |
|
F11.182 Opioid abuse with opioid-induced sleep disorder |
G31.83 Dementia with Lewy bodies |
H53.16 Psychophysical visual disturbances |
|
F11.282 Opioid dependence with opioid-induced sleep disorder |
G31.84 Mild cognitive impairment, so stated |
H81.09 Ménière's disease, unspecified ear |
|
F11.982 Opioid use, unspecified with opioid-induced sleep disorder |
G31.9 Degenerative disease of nervous system, unspecified |
H81.4 Vertigo of central origin |
|
F13.182 Sedative, hypnotic or anxiolytic abuse with sedative, hypnotic or anxiolytic-induced sleep disorder |
G35 Multiple sclerosis |
H90.3 Sensorineural hearing loss, bilateral |
|
F13.282 Sedative, hypnotic or anxiolytic dependence with sedative, hypnotic or anxiolytic-induced sleep disorder |
G37.8 Other specified demyelinating diseases of central nervous system |
H90.5 Unspecified sensorineural hearing loss |
|
F13.982 Sedative, hypnotic or anxiolytic use, unspecified with sedative, hypnotic or anxiolytic-induced sleep disorder |
G40 Epilepsy and recurrent seizures |
H93.19 Tinnitus, unspecified ear |
|
F14.182 Cocaine abuse with cocaine-induced sleep disorder |
G40.A01 Absence epileptic syndrome, not intractable, with status epilepticus |
J96.00 Acute respiratory failure, unspecified whether with hypoxia or hypercapnia |
|
F14.282 Cocaine dependence with cocaine-induced sleep disorder |
G40.A09 Absence epileptic syndrome, not intractable, without status epileptics |
J96.10 Chronic respiratory failure, unspecified whether with hypoxia or hypercapnia |
|
F14.982 Cocaine use, unspecified with cocaine-induced sleep disorder |
G40.101 Localization-related (focal) (partial) symptomatic epilepsy and epileptic syndromes with simple partial seizures, not intractable, with status epilepticus |
J96.20 Acute and chronic respiratory failure, unspecified whether with hypoxia or hypercapnia |
|
F15.182 Other stimulant abuse with stimulant-induced sleep disorder |
G40.109 Localization-related (focal) (partial) symptomatic epilepsy and epileptic syndromes with simple partial seizures, not intractable, without status epilepticus |
J96.90 Respiratory failure, unspecified, unspecified whether with hypoxia or hypercapnia |
|
F15.282 Other stimulant dependence with stimulant-induced sleep disorder |
G40.3 Generalized idiopathic epilepsy and epileptic syndromes |
N39.44 Nocturnal enuresis |
|
F15.920 Other stimulant use, unspecified with intoxication, uncomplicated |
G40.30 Generalized idiopathic epilepsy and epileptic syndromes, not intractable |
M79.7 Fibromyalgia |
|
F19.182 Other psychoactive substance abuse with psychoactive substance-induced sleep disorder |
G40.301 Generalized idiopathic epilepsy and epileptic syndromes, not intractable, with status epilepticus |
M79.1 Myalgia |
|
F19.282 Other psychoactive substance dependence with psychoactive substance-induced sleep disorder |
G43 Migraine |
N52.9 Male erectile dysfunction, unspecified |
|
F19.939 Other psychoactive substance use, unspecified with withdrawal, unspecified |
G44.1 Vascular headache, not elsewhere classified |
P28.3 Primary sleep apnea of newborn |
|
F19.950 Other psychoactive substance use, unspecified with psychoactive substance-induced psychotic disorder with delusions |
G47.00 Insomnia, unspecified |
R06.00 Dyspnea, unspecified |
|
F19.982 Other psychoactive substance use, unspecified with psychoactive substance-induced sleep disorder |
G47.01 Insomnia due to medical condition |
R06.3 Periodic breathing |
|
F19.99 Other psychoactive substance use, unspecified with unspecified psychoactive substance-induced disorder |
G47.09 Other insomnia |
R06.09 Other forms of dyspnea |
|
F32 Depressive episode |
G47.10 Hypersomnia, unspecified |
R06.83 Snoring |
|
F34.0 Cyclothymic disorder |
G47.11 Idiopathic hypersomnia with long sleep time |
R06.89 Other abnormalities of breathing |
|
F34.1 Dysthymic disorder |
G47.13 Recurrent hypersomnia |
R13.0 Aphagia |
|
F41.1 Generalized anxiety disorder |
G47.14 Hypersomnia due to medical condition |
R13.10 Dysphagia, unspecified |
|
F43.0 Acute stress reaction |
G47.19 Other hypersomnia |
R25.0 Abnormal head movements |
|
F43.12 Post-traumatic stress disorder |
G47.20 Circadian rhythm sleep disorder, unspecified type |
R25.1 Tremor, unspecified |
|
F44.4 Conversion disorder with motor symptom or deficit |
G47.21 Circadian rhythm sleep disorder, delayed sleep phase type |
R25.2 Cramp and spasm |
|
F44.6 Conversion disorder with sensory symptom or deficit |
G47.22 Circadian rhythm sleep disorder, advanced sleep phase type |
R25.3 Fasciculation |
|
F51.02 Adjustment insomnia |
G47.23 Circadian rhythm sleep disorder, irregular sleep wake type |
R25.9 Unspecified abnormal involuntary movements |
|
F51.01 Primary insomnia |
G47.24 Circadian rhythm sleep disorder, free running type |
R40.0 Somnolence |
|
F51.03 Paradoxical insomnia |
G47.25 Circadian rhythm sleep disorder, jet lag type |
R40.1 Stupor |
|
F51.04 Psychophysiologic insomnia |
G47.26 Circadian rhythm sleep disorder, shift work type |
R41.2 Retrograde amnesia |
|
F51.05 Insomnia due to other mental disorder |
G47.27 Circadian rhythm sleep disorder in conditions classified elsewhere |
R41.3 Other amnesia |
|
F51.09 Other insomnia not due to a substance or known physiological condition |
G47.29 Other circadian rhythm sleep disorder |
R48.3 Visual agnosia |
|
F51.11 Primary hypersomnia |
G47.30 Sleep apnea, unspecified |
S06.890A Other specified intracranial injury without loss of |
|
F51.12 Insufficient sleep syndrome |
G47.31 Primary central sleep apnea |
T14.90XA Injury, unspecified, initial encounter |
|
F51.13 Hypersomnia due to other mental disorder |
G47.32 High altitude periodic breathing |
T56.0X4A Toxic effect of lead and its compounds, undetermined, initial encounter |
|
F51.19 Other hypersomnia not due to a substance or known physiological condition |
G47.33 Obstructive sleep apnea (adult) (pediatric) |
T56.1X4A Toxic effect of mercury and its compounds, undetermined, initial encounter. |
|
F51.8 Other sleep disorders not due to a substance or known physiological condition |
G47.34 Idiopathic sleep related nonobstructive alveolar hypoventilation |
T56.3X4A Toxic effect of cadmium and its compounds, undetermined, initial encounter |
|
F51.3 Sleepwalking (somnambulism) |
G47.35 Congenital central alveolar hypoventilation syndrome |
T56.891A Toxic effect of other metals, accidental (unintentional), initial encounter |
|
F81.81 Disorder of written expression |
G47.36 Sleep related hypoventilation in conditions classified elsewhere |
T57.0X4A Toxic effect of arsenic and its compounds, undetermined, initial encounter |
|
F81.89 Other developmental disorders of scholastic skills |
G47.37 Central sleep apnea in conditions classified elsewhere |
T57.2X4A Toxic effect of manganese and its compounds, undetermined, initial encounter |
|
G10 Huntington's disease |
G47.411 Narcolepsy with cataplexy |
T56.7X4A Toxic effect of beryllium and its compounds, undetermined, initial encounter |
|
G20 Parkinson's disease |
G47.429 Narcolepsy without cataplexy |
Z77.011 Contact with and (suspected) exposure to lead |
|
G21.0 Malignant neuroleptic syndrome |
G47.50 Parasomnia, unspecified |
|
|
G21.19 Other drug induced secondary parkinsonism |
G47.51 Confusional arousals |
|
|
G21.8 Other secondary parkinsonism |
G47.52 REM sleep behavior disorder |
|
References
- 2019 Alzheimer's Disease Facts and Figures . Alzheimer's Assocation. Retrieved 2021-11-15
- Mental Illness . National Institute of Mental Health. Retrieved 2021-11-15
- Alzheimer's Disease and Healthy Aging Data . Centers for Disease Control and Prevention . Retrieved 2021-11-15
- Dementia . World Health Organization. Retrieved 2021-11-15
- Minorities and Women Are at Greater Risk for Alzheimer's Disease . Centers for Disease Control and Prevention . Retrieved 2021-11-15
- Jeffrey L. Cummings; Alzheimer Disease. JAMA: The Journal of the American Medical Association 2002, 287, 2335-2338, 10.1001/jama.287.18.2335.
- Alistair Burns; Stephen Iliffe; Dementia. BMJ 2009, 338, b75-b75, 10.1136/bmj.b75.
- Report to Congress: Traumatic Brain Injury in the United States . Centers for Disease Control and Prevention. Retrieved 2021-11-15
- Data and Statistics About ADHD . Centers for Disease Control and Prevention . Retrieved 2021-11-15
