Oral mucositis (OM) is a pathological condition with several oral manifestations, originate from cytotoxic effects of non-surgical cancer therapies. The clinical manifestation ranges from diffuse erythematous areas to necrotic ulcers lesions in the mucosa. The oral mucosa presents confluent, deep, and devastatingly painful ulcerations in the most advanced clinical form.[1] Almost all oral or oropharyngeal mucosa areas undergoing radiation will develop this side effect, however, the patients undergoing chemotherapy regiment develop the condition depending on the dose and cytotoxicity of the drug used. Usually, incidence goes around 20 to 40% for solid tumors, while in the therapies with a high dose of cytotoxic drugs, like hematopoietic stem cell transplant, the incidence is around 80%.[2] The patients that develop OM during the cancer treatment can manifest alterations in physical, mental, emotional, and social health factors, proving an unhealthy state. Patients present diet modifications and weight loss, necessitate opioid analgesics, require supplemental nutrition, increase the risk of bacteremia and sepsis, disrupt optimal cancer therapy, and increase healthcare costs. [3]
It is common the association of head and neck cancer and OM in medical care however, the frequency in other cancers has long been overlooked and underreported. For this reason, a multidisciplinary team composed of other health professionals, as dentists, can identify and treat pathologies in advance during oncological treatment.
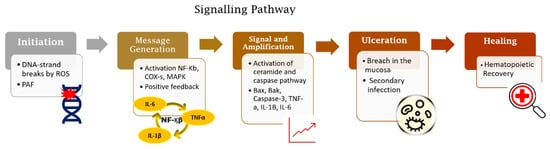
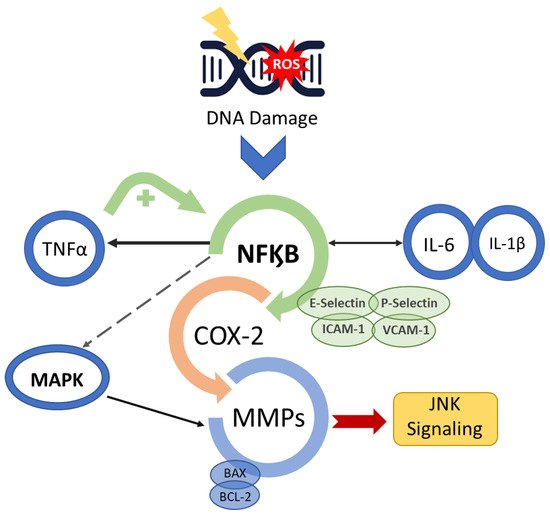
The OM development is described in a five-step pathogenesis model with several biological factors’ combinations. The lesion occurs with the damage of basal epithelial cells due to the radio-chemotherapy. The cascade of events starts with severe alterations in the environment that involves the generation of reactive oxygen species (ROS), activation of transcription factors (NF-kB) and inflammatory pathways (COX), and up-regulation of proinflammatory cytokines (TNF-a, IL1b, and IL-6).[2]
The clinical diagnosis can be made in the early stages. The mucosa presents erythema, the patients complain of burning and intolerance of some specific foods. After two weeks, the ulcerated lesions can be detected in one or more areas of the oral cavity. The patient refers to slight discomfort and inconvenience to severe pain, dysphagia, and difficulty in eating that lead to the opioid intervention. As a result of the cancer treatment, it is common to occur salivary alterations in composition and quantity, leading to the exasperation of OM development and impairment in the patient’s quality of life. The lesions recover depending on the patient's immune compromise, however, heal spontaneously for at least 2 weeks following the completion of the therapeutic regimen.[4] Medical and scientific community discourse about effective management of OM in cancer patients due to its high incidence and clinical significance in patient prognosis. Several scientific studies are carried out to discover a well-defined strategy that provides improved management of OM that may allow more aggressive therapeutic doses and more effective cancer treatment, improved patient survival, and wellbeing.[5]
All guidelines for the management of OM agree OM management can be divided into three basic components: general oral care, prevention, and palliative cares. The oral care purpose is to reduce some host-related risk factors for stomatitis, including lowering the impact of oral microbial flora. Therefore, a simple care protocol must be suggested, as brushing teeth, daily flossing, and mouth rinsing. In addition, spicy food, alcoholic beverages, and alcohol-based mouthwashes must be avoided.[6]
Prevention is the second most important factor in addressing oral mucositis. The combination of agents and physical strategies can provide anti-inflammatory, analgesic, and anti-microbial more effective effects in OM management. The preventive use of oral cryotherapy and photobiomodulation (PBM) therapy showed a reduction in the impact of the treatment toxicity in the oral mucosa.[7] The OM treatment effectivity increase can be noted with the use of several pharmacological agents (pentoxifylline, benzydamine hydrochloride, thalidomide, and simvastatin) and natural products such as Omega-3 FFA, essential oils from manuka (Leptospermum scoparium), vitamins, glutamine, chamomile, aloe vera, and curcumin.[8] The OM palliative care has focused on symptom control using topical or systemic analgesics and the application of barrier agents to cover injured mucosa.[3]
In conclusion, OM is a painful and wasting consequence of anticancer chemotherapy and/or radiotherapy. The occurrence of this pathology increases the risk of treatment interruption and a decrease in quality of life. A multidisciplinary team can provide global attention during the treatment, detecting early necessary interventions to manage the side effects of the cytotoxic therapeutic and providing wellbeing for cancer patients.
Reference:
1. Sonis, S. Oral Mucositis. Volume1. Springer Healthcare 2012 ISBN 10.1007/978-1-907673-46-7.
2. Sollecito,PT. Clinical Approaches to Oral Mucosal Disorders: Part II, An Issue of Dental Clinics of North America, Volume 58, Issue 2 of The Clinics: Dentistry, Elsevier Health Sciences, 2014, ISBN 0323289967, 9780323289962).
3. Sonis, S.T. Treatment for Oral Mucositis—Current Options and an Update of Small Molecules Under Development. Current Treatment Options in Oncology. 2021 22.. doi:10.1007/s11864-021-00823-6).
4. (Scully, C., Sonis, S., Diz, P., 2006. Oral mucositis. Oral Diseases 12, 229–241. doi:10.1111/j.1601-0825.2006.01258.x).
5. Campos MI, Campos CN, Aarestrup FM, Aarestrup BJ. Oral mucositis in cancer treatment: Natural history, prevention and treatment. Mol Clin Oncol. 2014;2(3):337-340. doi:10.3892/mco.2014.2536.
6. Lionel D, Christophe L, Marc A, Jean-Luc C. Oral mucositis induced by anticancer treatments: physiopathology and treatments. Ther Clin Risk Manag. 2006;2(2):159-168. doi:10.2147/tcrm.2006.2.2.159
7. de Carvalho, P.A.G.; Lessa, R.C.; Carraro, D.M.; Assis Pellizzon, A.C.; Jaguar, G.C.; Alves, F.A. Three photobiomodulation protocols in the prevention/treatment of radiotherapy-induced oral mucositis. Photodiagnosis Photodyn Ther. 2020 Sep; 31:101906. doi: 10.1016/j.pdpdt.2020.101906.
8. Lessa, R.C.; Alves, F.A.; Fortunati E.; Lu J. Oral Mucositis in Cancer and Potential Use of Omega-3 Free Fatty Acids in Its Management: A Review Biomedicines 2021 doi: 10.3390/biomedicines9111531.
- oral mucositis
- inflammation
- polyunsaturated fatty acids
- omega-3 fatty acids
1. Introduction
2. Biomolecular Mechanisms of OM
Radiation-induced and chemotherapy-induced OM have similar developmental mechanisms [1]. The cascade of biological events responsible for the genesis of OM begins with the induction of DNA damage caused by radiation or chemotherapeutic cancer therapy [5][6][6,13] (Figure 1).