Several FDA-approved available antiviral drugs, alone or in combination, have been screened clinically for their extended use since the early phase of the current pandemic to find a safe and effective treatment option against COVID-19, and many clinical trials of these antiviral drugs are still ongoing. However, an in-depth understanding is required from current clinical literature reports to execute integrated approaches between computational and experimental methods to guarantee high success rates of repositioned drugs. Moreover, multiple challenges associated with repurposed drugs have been identified, including dose adjustments, route of administration, acute/chronic toxicity, appropriate delivery systems, etc..
- coronavirus disease 2019 (COVID-19)
- repurposing strategy
- repurposed drugs
- remdesivir
- interferon type I
- clinical trials
1. Introduction
The outbreak of coronavirus disease 2019 (COVID-19) has created a lot of burden on the global medical system, public health, and economic and social life of human beings [1,2]. The causative pathogen identified for COVID-19 is called severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which emerged from viruses of unknown sources [3,4]. SARS-CoV-2 is a type of ß-coronavirus (β-CoV) that belongs to the coronavirus group. The human coronavirus group causes several outbreaks, including the severe acute respiratory syndrome (SARS-CoV) epidemic from 2002 to 2004 and the Middle East respiratory syndrome (MERS-CoV) outbreak in the Middle East, Africa, and South Asia, and many more countries during 2012 [5,6]. Wuhan, China, was the first city for the occurrence of COVID-19, and after that, it spread all over the world, infecting around 218 million people together with over 4.5 million total deaths, according to the COVID-19 global case dashboard of the World Health Organization (WHO), by 29 August 2021 [7]. Based on the data from January 2020, the WHO declared COVID-19 a Public Health Emergency of International Concern (PHEIC), which was followed by a pandemic on 11 March 2020 [8].
To date, no effective and approved antiviral treatment is available to fight against COVID-19. However, some recommendations are being practiced concurrently to manage individual patients’ needs, such as antipyretic drugs for fever, oxygen therapy for respiratory distresses, antimicrobial therapy with mechanical ventilation applied in some severe cases depending on the clinical condition of the patient, and so on [11,12]. Meanwhile, the drug repurposing strategy is being continuously used in COVID-19 treatment. Drug repurposing or drug repositioning is tactically a rapid process to identify new pharmacological indications rather than the original purpose of investigational, existing, already marketed or FDA-approved drugs for the treatment of diseases. This advantageous method provides a great benefit in circumventing some de novo drug design and development stages. Thus, the technique decreases scheduled periods of drug development, reduces failure risk, and protects funds from being wasted [13]. In addition, it is crucial for a drug to be effective, proportionally related to clinical efficacy, or to produce desired pharmacological activities for a specified indication in humans. A potential drug must be passed through efficacy trials to fulfill the principal requirements of clinical efficacy, including several human trial phases [14]. In other words, efficacy trials determine the possibility of an intervention to produce expected results under ideal circumstances or the degree of beneficial effects under real-world clinical settings [15,16].
More importantly, SARS-CoV-2 is the seventh member of the genus β- coronavirus and the Coronavirdiae family [17]. Genome sequencing of SARS -CoV-2 demonstrated that the virus is almost 79% and 50% identical with the previous two SARS-CoV and MERS coronaviruses, respectively [18]. So, it might be very convenient and rational to repurpose the currently available antiviral drugs used against the two previous viral pandemics (SARS and MERS CoV) or have evidence of previous experience. Furthermore, it has been perceived that drug repurposing has already become a “universal strategy” to face the challenges of the COVID-19 pandemic because of several advantages it offers. These include fewer clinical trial steps, the availability of the formulation and distribution of the existing pharmaceutical supply, the possibility of more effective treatment of known combination therapy, the discovery of novel mechanisms of actions of old drugs or new classes of medicines, [19] and the elimination of “activation barriers” in the early stages of research, thus ensuring the rapid advancement of any project to disease-oriented research [20].
Several FDA-approved available antiviral drugs, alone or in combination, have been screened clinically for their extended use since the early phase of the current pandemic to find a safe and effective treatment option against COVID-19 [21,22], and many clinical trials of these antiviral drugs are still ongoing. However, an in-depth understanding is required from current clinical literature reports to execute integrated approaches between computational and experimental methods to guarantee high success rates of repositioned drugs. Moreover, multiple challenges associated with repurposed drugs have been identified, including dose adjustments, route of administration, acute/chronic toxicity, appropriate delivery systems, etc. [23,24]. Although many preliminary studies exhibited promising results, several extensive clinical investigations reported contradictory findings with significant adverse effects of these elongated applications of antiviral drugs. However, numerous clinical trials conducted with larger samples/patients have recently disclosed many mixed results, which needs careful study. Therefore, it is essential to review comprehensively the uses of repurposed drugs focusing on the therapeutic strategies, advantages, adverse drug reactions, and respective delivery approaches for instigating an instrumental battle against COVID-19. Likewise, it is also necessary to know the clear disease pathology and critical strategies to identify new drugs capable of protecting against highly contagious viral infections, including the SARS-CoV-2 infection. This article summarizes the current understanding of clinical efficacy and the adverse drug reaction of various antiviral drugs used for SARS-CoV-2-infected patients across the world. Here, we also illustrated
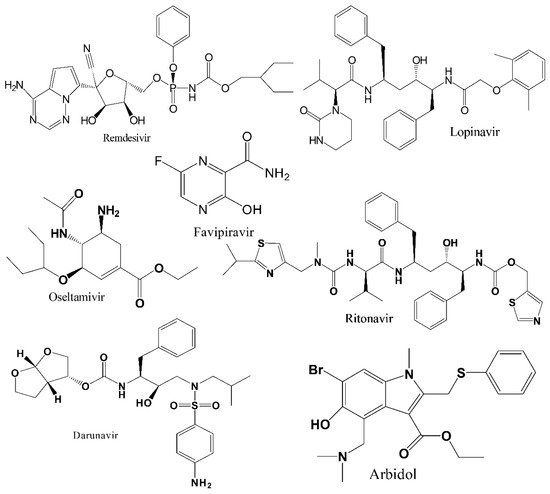
to represent the chemical structures of the seven repurposed antivirals drugs for use against COVID-19.
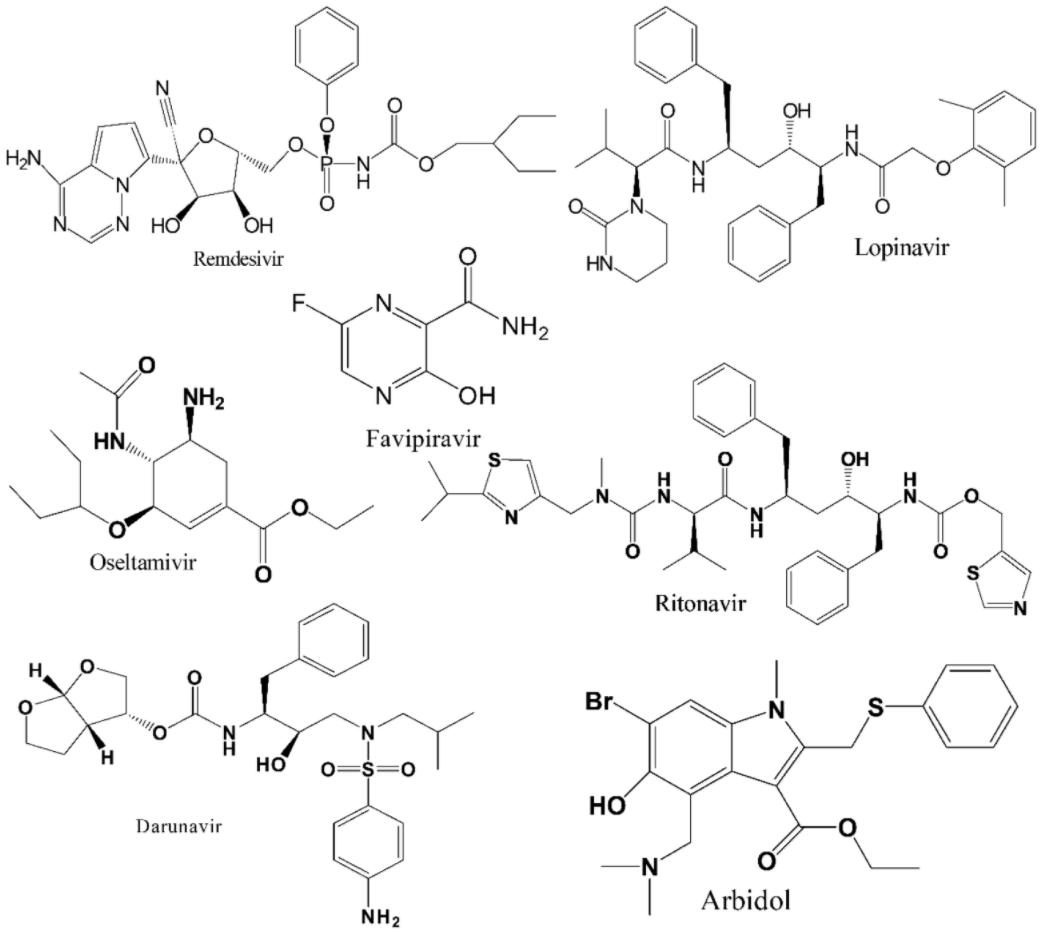
Chemical structures of the selected most promising antiviral drugs against COVID-19.
2. Discussion and Concluding Remarks
References
- Ashraf, B.N. Economic impact of government interventions during the COVID-19 pandemic: International evidence from financial markets. J. Behav. Exp. Financ. 2020, 27, 100371. [Google Scholar] [CrossRef]
- Hossain, M.J.; Ahmmed, F.; Rahman, S.; Sanam, S.; Emran, T.B.; Mitra, S. Impact of online education on fear of academic delay and psychological distress among university students following one year of COVID-19 outbreak in Bangladesh. Heliyon 2021, 7, e07388. [Google Scholar] [CrossRef]
- Gollakner, R.; Capua, I. Is COVID-19 the first pandemic that evolves into a panzootic? Vet. Ital. 2020, 56, 11–12. [Google Scholar] [CrossRef]
- Yoo, H.S.; Yoo, D. COVID-19 and veterinarians for one health, zoonotic- and reverse-zoonotic transmissions. J. Vet. Sci. 2020, 21, e51. [Google Scholar] [CrossRef] [PubMed]
- Gupta, N.; Singhai, M.; Garg, S.; Shah, D.; Sood, V.; Singh, S.K. The missing pieces in the jigsaw and need for cohesive research amidst coronavirus infectious disease 2019 global response. Med. J. Armed Forces India 2020, 76, 132–135. [Google Scholar] [CrossRef] [PubMed]
- Decaro, N.; Lorusso, A. Novel human coronavirus (SARS-CoV-2): A lesson from animal coronaviruses. Vet. Microbiol. 2020, 244, 108693. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Weekly Operational Update on COVID-19—20 July 2021; World Health Organization: Geneva, Switzerland, 2021; pp. 1–13. [Google Scholar]
- Hossain, M.J.; Kuddus, M.R.; Rahman, S.M.A. Knowledge, attitudes, and behavioral responses toward COVID-19 during early phase in bangladesh: A questionnaire-based study. Asia Pac. J. Public Health 2021, 33, 141–144. [Google Scholar] [CrossRef] [PubMed]
- Our World in Data. Statistics and Research. Coronavirus Disease 2019 (COVID-19) Vaccinations. Available online: https://ourworldindata.org/covid-vaccinations (accessed on 30 August 2021).
- Forni, G.; Mantovani, A.; COVID-19 Commission of Accademia Nazionale dei Lincei, Rome. COVID-19 vaccines: Where we stand and challenges ahead. Cell Death Differ. 2021, 28, 626–639. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Interim Clinical Guidance for Management of Patients with Confirmed Coronavirus Disease (COVID-19). Available online: https://stacks.cdc.gov/view/cdc/88624 (accessed on 30 August 2021).
- Hossain, M.J. Is Bangladesh moving toward herd immunity? Current COVID-19 perspective. Bangladesh J. Infect. Dis. 2020, 7 (Suppl. S2), S63–S66. [Google Scholar] [CrossRef]
- Pushpakom, S.; Iorio, F.; Eyers, P.A.; Escott, K.J.; Hopper, S.; Wells, A.; Doig, A.; Guilliams, T.; Latimer, J.; McNamee, C.; et al. Drug repurposing: Progress, challenges and recommendations. Nat. Rev. Drug Discov. 2019, 18, 41–58. [Google Scholar] [CrossRef]
- Hossain, M.J.; Kuddus, M.R.; Rashid, M.A.; Sultan, M.Z. Understanding and dealing the SARS-CoV-2 infection: An updated concise review. Bangladesh Pharm. J. 2021, 24, 61–75. [Google Scholar] [CrossRef]
- Godwin, M.; Ruhland, L.; Casson, I.; MacDonald, S.; Delva, D.; Birtwhistle, R.; Lam, M.; Seguin, R. Pragmatic controlled clinical trials in primary care: The struggle between external and internal validity. BMC Med. Res. Methodol. 2003, 3, 28. [Google Scholar] [CrossRef] [PubMed]
- Viveiros Rosa, S.G.; Santos, W.C. Clinical trials on drug repositioning for COVID-19 treatment. Rev. Panam. Salud Publica Pan Am. J. Public Health 2020, 44, e40. [Google Scholar] [CrossRef]
- Wrapp, D.; Wang, N.; Corbett, K.S.; Goldsmith, J.A.; Hsieh, C.L.; Abiona, O.; Graham, B.S.; McLellan, J.S. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science 2020, 367, 1260–1263. [Google Scholar] [CrossRef] [PubMed]
- Lu, R.; Zhao, X.; Li, J.; Niu, P.; Yang, B.; Wu, H.; Wang, W.; Song, H.; Huang, B.; Zhu, N.; et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding. Lancet 2020, 395, 565–574. [Google Scholar] [CrossRef]
- Oprea, T.I.; Bauman, J.E.; Bologa, C.G.; Buranda, T.; Chigaev, A.; Edwards, B.S.; Jarvik, J.W.; Gresham, H.D.; Haynes, M.K.; Hjelle, B.; et al. Drug repurposing from an academic perspective. Drug Discov. Today Ther. Strateg. 2011, 8, 61–69. [Google Scholar] [CrossRef]
- Senanayake, S.L. Drug repurposing strategies for COVID-19. Future Drug Discov. 2020, 2, FDD40. [Google Scholar] [CrossRef]
- Young, B.E.; Ong, S.W.X.; Kalimuddin, S.; Low, J.G.; Tan, S.Y.; Loh, J.; Ng, O.-T.; Marimuthu, K.; Ang, L.W.; Mak, T.M.; et al. Epidemiologic Features and Clinical Course of Patients Infected With SARS-CoV-2 in Singapore. JAMA 2020, 323, 1488–1494. [Google Scholar] [CrossRef]
- Yang, X.; Yu, Y.; Xu, J.; Shu, H.; Xia, J.; Liu, H.; Wu, Y.; Zhang, L.; Yu, Z.; Fang, M.; et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir. Med. 2020, 8, 475–481. [Google Scholar] [CrossRef]
- Parvathaneni, V.; Gupta, V. Utilizing drug repurposing against COVID-19—Efficacy, limitations, and challenges. Life Sci. 2020, 259, 118275. [Google Scholar] [CrossRef]
- Marra, F.; Smolders, E.J.; El-Sherif, O.; Boyle, A.; Davidson, K.; Sommerville, A.J.; Marzolini, C.; Siccardi, M.; Burger, D.; Gibbons, S.; et al. Recommendations for Dosing of Repurposed COVID-19 Medications in Patients with Renal and Hepatic Impairment. Drugs R&D 2021, 21, 9–27. [Google Scholar] [CrossRef]
- OECD. Policy Responses to Coronavirus (COVID-19). Coronavirus (COVID-19) Vaccines for Developing Countries: An Equal Shot at Recovery. Available online: https://www.oecd.org/coronavirus/policy-responses/coronavirus-covid-19-vaccines-for-developing-countries-an-equal-shot-at-recovery-6b0771e6/ (accessed on 27 July 2021).
- Bari, M.S.; Hossain, M.J.; Akhter, S.; Emran, T.B. Delta variant and black fungal invasion: A bidirectional assault might worsen the massive second/third stream of COVID-19 outbreak in South-Asia. Ethics Med. Public Health 2021, 19, 100722. [Google Scholar] [CrossRef]
- Williamson, B.N.; Feldmann, F.; Schwarz, B.; Meade-White, K.; Porter, D.P.; Schulz, J.; Van Doremalen, N.; Leighton, I.; Yinda, C.K.; Pérez-Pérez, L.; et al. Clinical benefit of remdesivir in rhesus macaques infected with SARS-CoV-2. Nature 2020, 585, 273–276. [Google Scholar] [CrossRef] [PubMed]
- Nagata, T.; Lefor, A.K.; Hasegawa, M.; Ishii, M. Favipiravir: A new medication for the Ebola virus disease pandemic. Dis. Med. Public Health Prep. 2015, 9, 79–81. [Google Scholar] [CrossRef]
- Sharun, K.; Tiwari, R.; Dhama, K.; Emran, T.B.; Rabban, A.A.; Al Mutair, A. Emerging SARS-CoV-2 variants: Impact on vaccine efficacy and neutralizing antibodies. Hum. Vaccines Immunother. 2021, 17, 1–4. [Google Scholar] [CrossRef]
- Hossain, M.J. Impact of COVID-19 pandemic among health care providers in Bangladesh: A systematic review. Bangladesh J. Infect. Dis. 2020, 7 (Suppl. S2), S8–S15. [Google Scholar] [CrossRef]
- Hossain, M.J.; Islam, M.S.; Shahriar, S.; Sanam, S.; Emran, T.B.; Khatun, C.S.; Islam, M.R.; Mitra, S.; Dhama, K. Comedication of rabeprazole sodium causes potential drug-drug interaction with diabetic drug linagliptin: In-vitro and in-silico approaches. J. Exp. Biol. Agric. Sci. 2021, 9, 528–542. [Google Scholar] [CrossRef]
- Lai, C.C.; Wang, C.Y.; Hsueh, P.R. Coinfections among patients with COVID-19: The need for combination therapy with non-anti-SARS-CoV-2 agents? J. Microbiol. Immunol. Infect. 2020, 53, 505–512. [Google Scholar] [CrossRef] [PubMed]
- Zuo, Y.; Liu, Y.; Zhong, Q.; Zhang, K.; Xu, Y.; Wang, Z. Lopinavir/ritonavir and interferon combination therapy may help shorten the duration of viral shedding in patients with COVID-19: A retrospective study in two designated hospitals in Anhui, China. J. Med. Virol. 2020, 92, 2666–2674. [Google Scholar] [CrossRef] [PubMed]
- Hossain, M.J.; Rahman, S.M.A. Repurposing therapeutic agents against SARS-CoV-2 infection: Most promising and neoteric progress. Expert Rev. Anti. Infect. Ther. 2020, 19, 1009–1027. [Google Scholar] [CrossRef] [PubMed]
