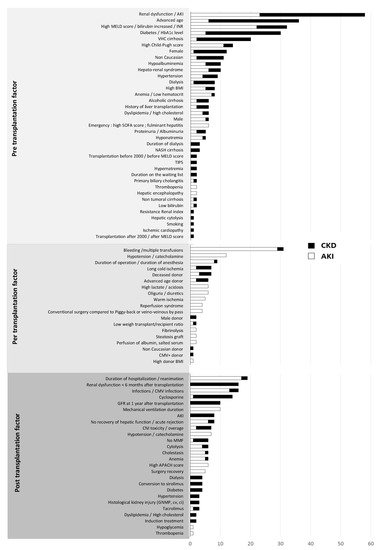
One-third of patients with cirrhosis present kidney failure (AKI and CKD). It has multifactorial causes and a harmful effect on morbidity and mortality before and after liver transplantation. Kidney function does not improve in all patients after liver transplantation, and liver transplant recipients are at a high risk of developing chronic kidney disease. The causes of renal dysfunction can be divided into three groups: pre-operative, perioperative and post-operative factors.
- liver transplantation
- kidney failure
- risk factor
- cirrhosis
- kidney protection
1. Kidney Function and Cirrhosis
2. Change in Kidney Function Post-Transplantation
2.1. Acute Kidney Injury after Liver Transplantation
2.2. Post-Transplantation Chronic Kidney Disease and End-Stage Renal Disease
2.3. The Contribution of Histology in Post-Transplantation Kidney Failure
2.4. The Impact of Kidney Function on Post-Transplantation Mortality
3. Factors Associated with the Risk of Post-Transplantation Renal Dysfunction
4. Markers and Predictive Models of Post-Transplantation Renal Dysfunction
4.1. Markers of Post-Transplantation Renal Dysfunction
4.2. Long-Term CKD Prediction Models
5. Prevention of Post-Liver Transplantation Kidney Failure
5.1. Pre-Transplantation Prevention
5.2. Post-Transplantation Prevention
5.2.1. Control of Cardiovascular Risk Factors
5.2.2. Optimization of Immunosuppressive Treatment
6. The Indication for Liver–Kidney Transplantation
With the increase in the incidence of kidney failure in patients awaiting liver transplantation and with the use of the MELD score, the indication for combined liver–kidney transplantation has been on the rise since 2002 [186][146]. However, it is often difficult to decide whether a dual transplantation is necessary as the assessment of the reversibility of kidney damage is complex, as is the risk of post-transplantation ESRD. Hmoud et al. showed that among patients listed for combined transplantation but who finally received liver transplantation alone, one-third exhibited recovered kidney function with a GFR of more than 60 mL/min/1.73 m2 [187][147]. Similarly, the survival benefit of a combined liver–kidney transplant is currently uncertain. Some studies have shown an advantage of combined transplantation in terms of survival, while others have shown no superiority [188,189,190][148][149][150]. However, most of these are observational monocentric studies conducted in a small number of subjects. In a study of 5609 patients who received combined or isolated liver transplant, Sharma et al. showed that the 5-year survival in patients on dialysis before transplantation was similar in both groups. On the other hand, there is a slight improvement in survival in favor of combined transplantation in patients not on dialysis at the time of transplantation (+3.7 months concentrated mainly in the first year). This is partly due to a better quality of kidney and liver transplants in combined transplants [191][151]. However, renal transplantation performed in a certain period of time after liver transplantation or staggered for 24–48 h (kidney on perfusion machine) appears to cause less morbidity and to have a protective effect on the renal transplant. This is partly explained by less exposure to SIRS in the post-liver transplantation period, which is responsible for early and late renal dysfunction [192][152]. A recent study reports better survival for patients who receive a liver transplant and then a kidney transplant within 3 years compared to patients who receive a liver and a kidney transplant simultaneously [193][153]. However, one of the advantages of combined transplantation remains immunological with a reduced risk of rejection in patients with pre-formed DSAs that allow the long-term preservation of kidney function [194][154]. In order to limit the indications for dual transplantation and to standardize the practices of each center, in 2017, an expert committee published the latest recommendations for combined liver–kidney transplantation in patients with cirrhosis who are on the waiting list (Table 1) [69]. It can be noted that the indications for dual transplantation in the case of CKD are relatively homogeneous over time, in contrast to the indications for combined transplantation for AKI, which remain more heterogeneous [195][155].|
Indications for a Combined Liver–Kidney Transplantation |
|---|
|
Patients with AKI associated with:
|
|
Patients with CKD (eGFR < 60 mL/min for at least 3 months) associated with:
|
AKI: acute kidney injury; GFR: glomerular filtration rate; MDRD: modification of diet in renal disease; CKD: chronic kidney disease; HUS: hemolytic uremic syndrome.
References
- Tsochatzis, E.A.; Bosch, J.; Burroughs, A.K. Liver cirrhosis. Lancet 2014, 383, 1749–1761.
- Wong, F.; Reddy, K.R.; O’Leary, J.G.; Tandon, P.; Biggins, S.W.; Garcia-Tsao, G.; Maliakkal, B.J.; Lai, J.C.; Fallon, M.B.; Vargas, H.E.; et al. Impact of chronic kidney disease on outcomes in cirrhosis. Liver Transpl. 2019, 25, 870–880.
- Wong, F. Acute kidney injury in liver cirrhosis: New definition and application. Clin. Mol. Hepatol. 2016, 22, 415–422.
- Cullaro, G.; Verna, E.C.; Lai, J.C. Association between renal function pattern and mortality in patients with cirrhosis. Clin. Gastroenterol. Hepatol. 2019, 17, 2364–2370.
- Tanriover, B.; Mejia, A.; Weinstein, J.; Foster, S.V.; Ghalib, R.; Mubarak, A.; Cheng, S.S. Analysis of kidney function and biopsy results in liver failure patients with renal dysfunction: A new look to combined liver kidney allocation in the post-MELD era. Transplantation 2008, 86, 1548–1553.
- Calmus, Y.; Conti, F.; Cluzel, P.; Hill, G.; Antoine, C.; Scatton, O.; Soubrane, O.; Glotz, D.; Pillebout, E.; Nochy, D. Prospective assessment of renal histopathological lesions in patients with end-stage liver disease: Effects on long-term renal function after liver transplantation. J. Hepatol. 2012, 57, 572–576.
- Ginès, P.; Solà, E.; Angeli, P.; Wong, F.; Nadim, M.K.; Kamath, P.S. Hepatorenal syndrome. Nat. Rev. Dis. Primers 2018, 4, 23.
- Nishi, H.; Shibagaki, Y.; Kido, R.; Tamura, S.; Nangaku, M.; Sugawara, Y.; Fujita, T. Chronic renal outcome after living donor liver transplantation. Clin. Transpl. 2013, 27, 90–97.
- Karapanagiotou, A.; Dimitriadis, C.; Papadopoulos, S.; Kydona, C.; Kefsenidis, S.; Papanikolaou, V.; Gritsi-Gerogianni, N. Comparison of RIFLE and AKIN criteria in the evaluation of the frequency of acute kidney injury in post-liver transplantation patients. Transpl. Proc. 2014, 46, 3222–3227.
- Wong, F.; Nadim, M.K.; Kellum, J.A.; Salerno, F.; Bellomo, R.; Gerbes, A.; Angeli, P.; Moreau, R.; Davenport, A.; Jalan, R.; et al. Working Party proposal for a revised classification system of renal dysfunction in patients with cirrhosis. Gut 2011, 60, 702–709.
- Mendizabal, M.; Reddy, K.R. Chronic hepatitis C and chronic kidney disease: Advances, limitations and unchartered territories. J. Viral Hepat. 2017, 24, 442–453.
- Biagioni, E.; Cavazzuti, I.; Busani, S.; Trevisan, D.; Zavatti, L.; Ferrari, E.; Girardis, M.; Massimo, G. Acute renal failure and renal replacement therapy in the postoperative period of orthotopic liver transplant patients versus nonelective abdominal surgery patients. Transpl. Proc. 2011, 43, 1145–1147.
- Cabezuelo, J.B.; Ramírez, P.; Ríos, A.; Acosta, F.; Torres, D.; Sansano, T.; Pons, J.A.; Bru, M.; Montoya, M.; Bueno, F.S.; et al. Risk factors of acute renal failure after liver transplantation. Kidney Int. 2006, 69, 1073–1080.
- Chen, J.; Singhapricha, T.; Hu, K.-Q.; Hong, J.C.; Steadman, R.H.; Busuttil, R.W.; Xia, V.W. Postliver transplant acute renal injury and failure by the RIFLE criteria in patients with normal pretransplant serum creatinine concentrations: A matched study. Transplantation 2011, 91, 348–353.
- Ferreira, A.C.; Nolasco, F.; Carvalho, D.; Sampaio, S.; Baptista, A.; Pessegueiro, P.; Monteiro, E.; Mourão, L.; Barroso, E. Impact of RIFLE classification in liver transplantation. Clin. Transpl. 2010, 24, 394–400.
- Hong, S.H.; Park, C.O.; Park, C.S. Prediction of newly developed acute renal failure using serum phosphorus concentrations after living-donor liver transplantation. J. Int. Med. Res. 2012, 40, 2199–2212.
- Jeong, T.-D.; Kim, S.; Lee, W.; Song, G.-W.; Kim, Y.-K.; Chun, S.; Lee, S.-G.; Min, W.-K. Neutrophil gelatinase-associated lipocalin as an early biomarker of acute kidney injury in liver transplantation. Clin. Transpl. 2012, 26, 775–781.
- Klaus, F.; Keitel da Silva, C.; Meinerz, G.; Carvalho, L.M.; Goldani, J.C.; Cantisani, G.; Zanotelli, M.L.; Duro Garcia, V.; Keitel, E. Acute kidney injury after liver transplantation: Incidence and mortality. Transpl. Proc. 2014, 46, 1819–1821.
- Kundakci, A.; Pirat, A.; Komurcu, O.; Torgay, A.; Karakayalı, H.; Arslan, G.; Haberal, M. Rifle criteria for acute kidney dysfunction following liver transplantation: Incidence and risk factors. Transpl. Proc. 2010, 42, 4171–4174.
- Leithead, J.A.; Ferguson, J.W.; Hayes, P.C. Modifiable patient factors are associated with the late decline in renal function following liver transplantation. Clin. Transpl. 2012, 26, E316–E323.
- Leithead, J.A.; Rajoriya, N.; Gunson, B.K.; Muiesan, P.; Ferguson, J.W. The evolving use of higher risk grafts is associated with an increased incidence of acute kidney injury after liver transplantation. J. Hepatol. 2014, 60, 1180–1186.
- Aksu Erdost, H.; Ozkardesler, S.; Ocmen, E.; Avkan-Oguz, V.; Akan, M.; Iyilikci, L.; Unek, T.; Ozbilgin, M.; Meseri Dalak, R.; Astarcioglu, I. Acute renal injury evaluation after liver transplantation: With RIFLE criteria. Transpl. Proc. 2015, 47, 1482–1487.
- Karapanagiotou, A.; Kydona, C.; Dimitriadis, C.; Sgourou, K.; Giasnetsova, T.; Fouzas, I.; Imvrios, G.; Gritsi-Gerogianni, N. Acute kidney injury after orthotopic liver transplantation. Transpl. Proc. 2012, 44, 2727–2729.
- Lin, Y.-H.; Lin, C.-C.; Wang, C.-C.; Wang, S.-H.; Liu, Y.-W.; Yong, C.-C.; Lin, T.-L.; Li, W.-F.; Concejero, A.M.; Chen, C.-L. The 4-week serum creatinine level predicts long-term renal dysfunction after adult living donor liver transplantation. Transpl. Proc. 2012, 44, 772–775.
- Nadeem, A.; Salahuddin, N.; El Hazmi, A.; Joseph, M.; Bohlega, B.; Sallam, H.; Sheikh, Y.; Broering, D. Chloride-liberal fluids are associated with acute kidney injury after liver transplantation. Crit. Care 2014, 18, 625.
- Nadim, M.K.; Genyk, Y.S.; Tokin, C.; Fieber, J.; Ananthapanyasut, W.; Ye, W.; Selby, R. Impact of the etiology of acute kidney injury on outcomes following liver transplantation: Acute tubular necrosis versus hepatorenal syndrome. Liver Transpl. 2012, 18, 539–548.
- Niemann, C.U.; Walia, A.; Waldman, J.; Davio, M.; Roberts, J.P.; Hirose, R.; Feiner, J. Acute kidney injury during liver transplantation as determined by neutrophil gelatinase-associated lipocalin. Liver Transpl. 2009, 15, 1852–1860.
- O’Riordan, A.; Wong, V.; McQuillan, R.; McCormick, P.A.; Hegarty, J.E.; Watson, A.J. Acute renal disease, as defined by the RIFLE criteria, post-liver transplantation. Am. J. Transpl. 2007, 7, 168–176.
- Sirivatanauksorn, Y.; Parakonthun, T.; Premasathian, N.; Limsrichamrern, S.; Mahawithitwong, P.; Kositamongkol, P.; Tovikkai, C.; Asavakarn, S. Renal dysfunction after orthotopic liver transplantation. Transpl. Proc. 2014, 46, 818–821.
- Tinti, F.; Umbro, I.; Meçule, A.; Rossi, M.; Merli, M.; Nofroni, I.; Corradini, S.G.; Poli, L.; Pugliese, F.; Ruberto, F.; et al. RIFLE criteria and hepatic function in the assessment of acute renal failure in liver transplantation. Transpl. Proc. 2010, 42, 1233–1236.
- Umbro, I.; Tinti, F.; Piselli, P.; Fiacco, F.; Giannelli, V.; Di Natale, V.; Zavatto, A.; Merli, M.; Rossi, M.; Ginanni Corradini, S.; et al. Occurrence of chronic renal failure in liver transplantation: Monitoring of pre- and posttransplantation renal function. Transpl. Proc. 2012, 44, 1956–1959.
- Utsumi, M.; Umeda, Y.; Sadamori, H.; Nagasaka, T.; Takaki, A.; Matsuda, H.; Shinoura, S.; Yoshida, R.; Nobuoka, D.; Satoh, D.; et al. Risk factors for acute renal injury in living donor liver transplantation: Evaluation of the RIFLE criteria. Transpl. Int. 2013, 26, 842–852.
- Wagener, G.; Minhaz, M.; Mattis, F.A.; Kim, M.; Emond, J.C.; Lee, H.T. Urinary neutrophil gelatinase-associated lipocalin as a marker of acute kidney injury after orthotopic liver transplantation. Nephrol. Dial. Transpl. 2011, 26, 1717–1723.
- Iglesias, J.I.; DePalma, J.A.; Levine, J.S. Risk factors for acute kidney injury following orthotopic liver transplantation: The impact of changes in renal function while patients await transplantation. BMC Nephrol. 2010, 11, 30.
- Sung, W.-C.; Yu, H.-P.; Tsai, Y.-F.; Chung, P.C.-H.; Lin, C.-C.; Lee, W.-C. The ratio of plasma interleukin-18 is a sensitive biomarker for acute kidney injury after liver transplantation. Transpl. Proc. 2014, 46, 816–817.
- Zhu, M.; Li, Y.; Xia, Q.; Wang, S.; Qiu, Y.; Che, M.; Dai, H.; Qian, J.; Ni, Z.; Axelsson, J.; et al. Strong impact of acute kidney injury on survival after liver transplantation. Transpl. Proc. 2010, 42, 3634–3638.
- Alvares-da-Silva, M.R.; Waechter, F.L.; Francisconi, C.F.; Barros, E.; Thomé, F.; Traiber, C.; Fonseca, D.L.; Zingani, J.M.; Sampaio, J.A.; Pinto, R.D.; et al. Risk factors for postoperative acute renal failure at a new orthotopic liver transplantation program. Transpl. Proc. 1999, 31, 3050–3052.
- Barri, Y.M.; Sanchez, E.Q.; Jennings, L.W.; Melton, L.B.; Hays, S.; Levy, M.F.; Klintmalm, G.B. Acute kidney injury following liver transplantation: Definition and outcome. Liver Transpl. 2009, 15, 475–483.
- Bilbao, I.; Salcedo, M.; Gómez, M.A.; Jimenez, C.; Castroagudín, J.; Fabregat, J.; Almohalla, C.; Herrero, I.; Cuervas-Mons, V.; Otero, A.; et al. Renal function improvement in liver transplant recipients after early everolimus conversion: A clinical practice cohort study in Spain. Liver Transpl. 2015, 21, 1056–1065.
- Cabezuelo, J.B.; Ramirez, P.; Acosta, F.; Sanchez Bueno, F.; Robles, R.; Pons, J.A.; Miras, M.; Munitiz, V.; Fernandez, J.A.; Lujan, J.; et al. Prognostic factors of early acute renal failure in liver transplantation. Transpl. Proc. 2002, 34, 254–255.
- Faenza, S.; Bernardi, E.; Cimatti, M.; Dante, A.; Mancini, E.; Miklosova, Z.; Piraccini, E.; Pierucci, E.; Riganello, I.; Spedicato, S.; et al. Acute renal failure after liver transplantation in MELD era. Transpl. Proc. 2007, 39, 1945–1946.
- Kim, J.M.; Jo, Y.Y.; Na, S.W.; Kim, S.I.; Choi, Y.S.; Kim, N.O.; Park, J.E.; Koh, S.O. The predictors for continuous renal replacement therapy in liver transplant recipients. Transpl. Proc. 2014, 46, 184–191.
- Koo, M.; Sabaté, A.; Ramos, E.; Dalmau, A.; León, E.; Fabregat, J.; Rafecas, A. Factors related to renal dysfunction after liver transplantation in patients with normal preoperative function. Rev. Esp. Anestesiol. Reanim. 2006, 53, 538–544.
- Lafayette, R.A.; Paré, G.; Schmid, C.H.; King, A.J.; Rohrer, R.J.; Nasraway, S.A. Pretransplant renal dysfunction predicts poorer outcome in liver transplantation. Clin. Nephrol. 1997, 48, 159–164.
- Lima, E.Q.; Zanetta, D.M.T.; Castro, I.; Massarollo, P.C.B.; Mies, S.; Machado, M.M.; Yu, L. Risk factors for development of acute renal failure after liver transplantation. Ren. Fail. 2003, 25, 553–560.
- Paramesh, A.S.; Roayaie, S.; Doan, Y.; Schwartz, M.E.; Emre, S.; Fishbein, T.; Florman, S.; Gondolesi, G.E.; Krieger, N.; Ames, S.; et al. Post-liver transplant acute renal failure: Factors predicting development of end-stage renal disease. Clin. Transpl. 2004, 18, 94–99.
- Rimola, A.; Gavaler, J.S.; Schade, R.R.; el-Lankany, S.; Starzl, T.E.; Van Thiel, D.H. Effects of renal impairment on liver transplantation. Gastroenterology 1987, 93, 148–156.
- Rueggeberg, A.; Boehm, S.; Napieralski, F.; Mueller, A.R.; Neuhaus, P.; Falke, K.J.; Gerlach, H. Development of a risk stratification model for predicting acute renal failure in orthotopic liver transplantation recipients. Anaesthesia 2008, 63, 1174–1180.
- McCauley, J.; Van Thiel, D.H.; Starzl, T.E.; Puschett, J.B. Acute and chronic renal failure in liver transplantation. Nephron 1990, 55, 121–128.
- Chuang, F.-R.; Lin, C.-C.; Wang, P.-H.; Cheng, Y.-F.; Hsu, K.-T.; Chen, Y.-S.; Lee, C.-H.; Chen, C.-L. Acute renal failure after cadaveric related liver transplantation. Transpl. Proc. 2004, 36, 2328–2330.
- Contreras, G.; Garces, G.; Quartin, A.A.; Cely, C.; LaGatta, M.A.; Barreto, G.A.; Roth, D.; Gomez, E. An epidemiologic study of early renal replacement therapy after orthotopic liver transplantation. J. Am. Soc. Nephrol. 2002, 13, 228–233.
- Fraley, D.S.; Burr, R.; Bernardini, J.; Angus, D.; Kramer, D.J.; Johnson, J.P. Impact of acute renal failure on mortality in end-stage liver disease with or without transplantation. Kidney Int. 1998, 54, 518–524.
- Brescia, M.D.G.; Massarollo, P.C.B.; Imakuma, E.S.; Mies, S. Prospective randomized trial comparing hepatic venous outflow and renal function after conventional versus piggyback liver transplantation. PLoS ONE 2015, 10, e0129923.
- Faenza, S.; Santoro, A.; Mancini, E.; Pareschi, S.; Siniscalchi, A.; Zanzani, C.; Pinna, A.D. Acute renal failure requiring renal replacement therapy after orthotopic liver transplantation. Transpl. Proc. 2006, 38, 1141–1142.
- Gainza, F.J.; Valdivieso, A.; Quintanilla, N.; Errazti, G.; Gastaca, M.; Campo, M.; Lampreabe, I.; Ortiz-de-Urbina, J. Evaluation of acute renal failure in the liver transplantation perioperative period: Incidence and impact. Transpl. Proc. 2002, 34, 250–251.
- Hilmi, I.A.; Damian, D.; Al-Khafaji, A.; Sakai, T.; Donaldson, J.; Winger, D.G.; Kellum, J.A. Acute kidney injury after orthotopic liver transplantation using living donor versus deceased donor grafts: A propensity score-matched analysis. Liver Transpl. 2015, 21, 1179–1185.
- Junge, G.; Schewior, L.V.; Kohler, S.; Neuhaus, R.; Langrehr, J.M.; Tullius, S.; Kahl, A.; Frei, U.; Neuhaus, P. Acute renal failure after liver transplantation: Incidence, etiology, therapy, and outcome. Transpl. Proc. 2006, 38, 723–724.
- Paydas, S.; Balal, M.; Demiryurek, H.; Kose, F. Renal function in patients with orthotopic liver transplantation. Ren. Fail. 2006, 28, 103–105.
- Platz, K.P.; Mueller, A.R.; Blumhardt, G.; Bachmann, S.; Bechstein, W.O.; Kahl, A.; Neuhaus, P. Nephrotoxicity after orthotopic liver transplantation in cyclosporin A and FK 506-treated patients. Transpl. Int. 1994, 7 (Suppl. S1), S52–S57.
- Portal, A.J.; McPhail, M.J.W.; Bruce, M.; Coltart, I.; Slack, A.; Sherwood, R.; Heaton, N.D.; Shawcross, D.; Wendon, J.A.; Heneghan, M.A. Neutrophil gelatinase—Associated lipocalin predicts acute kidney injury in patients undergoing liver transplantation. Liver Transpl. 2010, 16, 1257–1266.
- Sanchez, E.Q.; Gonwa, T.A.; Levy, M.F.; Goldstein, R.M.; Mai, M.L.; Hays, S.R.; Melton, L.B.; Saracino, G.; Klintmalm, G.B. Preoperative and perioperative predictors of the need for renal replacement therapy after orthotopic liver transplantation. Transplantation 2004, 78, 1048–1054.
- Velidedeoglu, E.; Bloom, R.D.; Crawford, M.D.; Desai, N.M.; Campos, L.; Abt, P.L.; Markmann, J.W.; Mange, K.C.; Olthoff, K.M.; Shaked, A.; et al. Early kidney dysfunction post liver transplantation predicts late chronic kidney disease. Transplantation 2004, 77, 553–556.
- Wei, Y.; Zhang, L.; Lin, H.; Li, J.; Li, B.; Yan, L.; Wen, T.; Zeng, Y.; Lu, S. Factors related to post-liver transplantation acute renal failure. Transpl. Proc. 2006, 38, 2982–2984.
- Xu, X.; Ling, Q.; Wei, Q.; Wu, J.; Gao, F.; He, Z.-L.; Zhou, L.; Zheng, S.-S. An effective model for predicting acute kidney injury after liver transplantation. Hepatobiliary Pancreat Dis. Int. 2010, 9, 259–263.
- Jindal, R.M.; Popescu, I. Renal dysfunction associated with liver transplantation. Postgrad. Med. J. 1995, 71, 513–524.
- Guitard, J.; Ribes, D.; Kamar, N.; Muscari, F.; Cointault, O.; Lavayssière, L.; Suc, B.; Esposito, L.; Peron, J.-M.; Rostaing, L. Predictive factors for chronic renal failure one year after orthotopic liver transplantation. Ren. Fail. 2006, 28, 419–425.
- Thongprayoon, C.; Kaewput, W.; Thamcharoen, N.; Bathini, T.; Watthanasuntorn, K.; Lertjitbanjong, P.; Sharma, K.; Salim, S.A.; Ungprasert, P.; Wijarnpreecha, K.; et al. Incidence and impact of acute kidney injury after liver transplantation: A meta-analysis. J. Clin. Med. 2019, 8, 372.
- Umbro, I.; Tinti, F.; Scalera, I.; Evison, F.; Gunson, B.; Sharif, A.; Ferguson, J.; Muiesan, P.; Mitterhofer, A.P. Acute kidney injury and post-reperfusion syndrome in liver transplantation. World J. Gastroenterol. 2016, 22, 9314–9323.
- Formica, R.N.; Aeder, M.; Boyle, G.; Kucheryavaya, A.; Stewart, D.; Hirose, R.; Mulligan, D. Simultaneous liver-kidney allocation policy: A proposal to optimize appropriate utilization of scarce resources. Am. J. Transpl. 2016, 16, 758–766.
- Ojo, A.O.; Held, P.J.; Port, F.K.; Wolfe, R.A.; Leichtman, A.B.; Young, E.W.; Arndorfer, J.; Christensen, L.; Merion, R.M. Chronic renal failure after transplantation of a nonrenal organ. N. Engl. J. Med. 2003, 349, 931–940.
- Herlenius, G.; Fistouris, J.; Olausson, M.; Felldin, M.; Bäckman, L.; Friman, S. Early renal function post-liver transplantation is predictive of progressive chronic kidney disease. Scand. J. Gastroenterol. 2008, 43, 344–349.
- Allen, A.M.; Kim, W.R.; Therneau, T.M.; Larson, J.J.; Heimbach, J.K.; Rule, A.D. Chronic kidney disease and associated mortality after liver transplantation—A time-dependent analysis using measured glomerular filtration rate. J. Hepatol. 2014, 61, 286–292.
- Fussner, L.A.; Charlton, M.R.; Heimbach, J.K.; Fan, C.; Dierkhising, R.; Coss, E.; Watt, K.D. The impact of gender and NASH on chronic kidney disease before and after liver transplantation. Liver Int. 2014, 34, 1259–1266.
- Aggarwal, S.; Kang, Y.; Freeman, J.A.; Fortunato, F.L.; Pinsky, M.R. Postreperfusion syndrome: Hypotension after reperfusion of the transplanted liver. J. Crit. Care 1993, 8, 154–160.
- Burra, P.; Senzolo, M.; Masier, A.; Prestele, H.; Jones, R.; Samuel, D.; Villamil, F. Factors influencing renal function after liver transplantation. Results from the MOST, an international observational study. Dig. Liver Dis. 2009, 41, 350–356.
- Fisher, N.C.; Nightingale, P.G.; Gunson, B.K.; Lipkin, G.W.; Neuberger, J.M. Chronic renal failure following liver transplantation: A retrospective analysis. Transplantation 1998, 66, 59–66.
- Gayowski, T.; Wagener, M.M.; Marino, I.R.; Singh, N. Quality of life and functional status of liver transplant recipients with recurrent viral hepatitis C. Transpl. Proc. 1999, 31, 1386–1387.
- Giusto, M.; Berenguer, M.; Merkel, C.; Aguilera, V.; Rubin, A.; Ginanni Corradini, S.; Mennini, G.; Rossi, M.; Prieto, M.; Merli, M. Chronic kidney disease after liver transplantation: Pretransplantation risk factors and predictors during follow-up. Transplantation 2013, 95, 1148–1153.
- Gonwa, T.A.; Mai, M.L.; Melton, L.B.; Hays, S.R.; Goldstein, R.M.; Levy, M.F.; Klintmalm, G.B. End-stage renal disease (ESRD) after orthotopic liver transplantation (OLTX) using calcineurin-based immunotherapy: Risk of development and treatment. Transplantation 2001, 72, 1934–1939.
- Kamar, N.; Guilbeau-Frugier, C.; Servais, A.; Tack, I.; Thervet, E.; Cointault, O.; Esposito, L.; Guitard, J.; Lavayssière, L.; Muscari, F.; et al. Kidney histology and function in liver transplant patients. Nephrol. Dial. Transpl. 2011, 26, 2355–2361.
- Karie-Guigues, S.; Janus, N.; Saliba, F.; Dumortier, J.; Duvoux, C.; Calmus, Y.; Lorho, R.; Deray, G.; Launay-Vacher, V.; Pageaux, G.-P. Long-term renal function in liver transplant recipients and impact of immunosuppressive regimens (calcineurin inhibitors alone or in combination with mycophenolate mofetil): The TRY study. Liver Transpl. 2009, 15, 1083–1091.
- Lamattina, J.C.; Foley, D.P.; Mezrich, J.D.; Fernandez, L.A.; Vidyasagar, V.; D’Alessandro, A.M.; Musat, A.I.; Samaniego-Picota, M.D.; Pascual, J.; Alejandro, M.D.R.; et al. Chronic kidney disease stage progression in liver transplant recipients. Clin. J. Am. Soc. Nephrol. 2011, 6, 1851–1857.
- LaMattina, J.C.; Mezrich, J.D.; Fernandez, L.A.; D’Alessandro, A.M.; Djamali, A.; Musat, A.I.; Pirsch, J.D.; Foley, D.P. Native kidney function following liver transplantation using calcineurin inhibitors: Single-center analysis with 20 years of follow-up. Clin. Transpl. 2013, 27, 193–202.
- Lee, J.P.; Heo, N.J.; Joo, K.W.; Yi, N.J.; Suh, K.-S.; Moon, K.C.; Kim, S.G.; Kim, Y.S. Risk factors for consequent kidney impairment and differential impact of liver transplantation on renal function. Nephrol. Dial. Transpl. 2010, 25, 2772–2785.
- Leithead, J.A.; Ferguson, J.W.; Bates, C.M.; Davidson, J.S.; Simpson, K.J.; Hayes, P.C. Chronic kidney disease after liver transplantation for acute liver failure is not associated with perioperative renal dysfunction. Am. J. Transpl. 2011, 11, 1905–1915.
- Machicao, V.I.; Srinivas, T.R.; Hemming, A.W.; Soldevila-Pico, C.; Firpi, R.J.; Reed, A.I.; Morelli, G.J.; Nelson, D.R.; Abdelmalek, M.F. Impact of implementation of the MELD scoring system on the prevalence and incidence of chronic renal disease following liver transplantation. Liver Transpl. 2006, 12, 754–761.
- Morard, I.; Mentha, G.; Spahr, L.; Majno, P.; Hadengue, A.; Huber, O.; Morel, P.; Giostra, E. Long-term renal function after liver transplantation is related to calcineurin inhibitors blood levels. Clin. Transpl. 2006, 20, 96–101.
- Moreno, J.M.; Cuervas-Mons, V.; Rubio, E.; Pons, F.; de Herreros, A.T.; Turrión, V.S.; Millán, I. Chronic renal dysfunction after liver transplantation in adult patients: Prevalence, risk factors, and impact on mortality. Transpl. Proc. 2003, 35, 1907–1908.
- O’Riordan, A.; Wong, V.; McCormick, P.A.; Hegarty, J.E.; Watson, A.J. Chronic kidney disease post-liver transplantation. Nephrol. Dial. Transpl. 2006, 21, 2630–2636.
- Pawarode, A.; Fine, D.M.; Thuluvath, P.J. Independent risk factors and natural history of renal dysfunction in liver transplant recipients. Liver Transpl. 2003, 9, 741–747.
- Ramachandran, J.; Juneja, R.; John, L.; Dutta, A.K.; Chen, J.W.; Woodman, R.J.; Wigg, A.J. Chronic kidney disease following liver transplantation: A South Australian experience. Transpl. Proc. 2010, 42, 3644–3646.
- Sanchez, E.Q.; Melton, L.B.; Chinnakotla, S.; Randall, H.B.; McKenna, G.J.; Ruiz, R.; Onaca, N.; Levy, M.F.; Goldstein, R.M.; Klintmalm, G.B. Predicting renal failure after liver transplantation from measured glomerular filtration rate: Review of up to 15 years of follow-up. Transplantation 2010, 89, 232–235.
- Schmitz, V.; Laudi, S.; Moeckel, F.; Puhl, G.; Stockmann, M.; Tran, Z.V.; Kahl, A.; Neumann, U.; Neuhaus, P. Chronic renal dysfunction following liver transplantation. Clin. Transpl. 2008, 22, 333–340.
- Sezer, S.; Karakan, S.; Erişmiş, B.; Çolak, T.; Haberal, M. Risk factors for kidney impairment and differential impact of liver transplantation on renal function. Transpl. Proc. 2011, 43, 609–611.
- Shao, Z.-Y.; Yan, L.-N.; Wang, W.-T.; Li, B.; Wen, T.-F.; Yang, J.-Y.; Xu, M.-Q.; Zhao, J.-C.; Wei, Y.-G. Prophylaxis of chronic kidney disease after liver transplantation—Experience from west China. World J. Gastroenterol. 2012, 18, 991–998.
- Sharma, P.; Goodrich, N.P.; Schaubel, D.E.; Guidinger, M.K.; Merion, R.M. Patient-specific prediction of ESRD after liver transplantation. J. Am. Soc. Nephrol. 2013, 24, 2045–2052.
- Sharma, P.; Welch, K.; Eikstadt, R.; Marrero, J.A.; Fontana, R.J.; Lok, A.S. Renal outcomes after liver transplantation in the model for end-stage liver disease era. Liver Transpl. 2009, 15, 1142–1148.
- Cohen, A.J.; Stegall, M.D.; Rosen, C.B.; Wiesner, R.H.; Leung, N.; Kremers, W.K.; Zein, N.N. Chronic renal dysfunction late after liver transplantation. Liver Transpl. 2002, 8, 916–921.
- de Boccardo, G.; Kim, J.-Y.; Schiano, T.D.; Maurette, R.; Gagliardi, R.; Murphy, B.; Emre, S.; Akalin, E. The burden of chronic kidney disease in long-term liver transplant recipients. Transpl. Proc. 2008, 40, 1498–1503.
- Hao, J.-C.; Wang, W.-T.; Yan, L.-N.; Li, B.; Wen, T.-F.; Yang, J.-Y.; Xu, M.-Q.; Zhao, J.-C.; Wei, Y.-G. Effect of low-dose tacrolimus with mycophenolate mofetil on renal function following liver transplantation. World J. Gastroenterol. 2014, 20, 11356–11362.
- Jain, A.; Singhal, A.; Fontes, P.; Mazariegos, G.; DeVera, M.E.; Cacciarelli, T.; Lopez, R.C.; Sindhi, R.; Humar, A.; Marsh, J.W. One thousand consecutive primary liver transplants under tacrolimus immunosuppression: A 17- to 20-year longitudinal follow-up. Transplantation 2011, 91, 1025–1030.
- Kim, S.G.; Kim, H.J.; Lee, J.-P.; Lee, S.G.; Kim, Y.S.; Ahn, C.; Han, J.S.; Kim, S.; Lee, J.S.; Suh, K.-S. Incidence and risk factors of renal dysfunction after liver transplantation in Korea. Transpl. Proc. 2004, 36, 2318–2320.
- Kim, D.Y.; Lim, C.; Parasuraman, R.; Raoufi, M.; Yoshida, A.; Arenas, J.; Denny, J.; Malinzak, L.; Almarastani, M.; Moonka, D.; et al. Renal disease burden following liver transplantation. Transpl. Proc. 2006, 38, 3663–3665.
- Patel, H.K.; Patel, A.; Abouljoud, M.; Divine, G.; Moonka, D.K. Survival after liver transplantation in patients who develop renal insufficiency. Transpl. Proc. 2010, 42, 4167–4170.
- Kalisvaart, M.; Schlegel, A.; Trivedi, P.J.; Roberts, K.; Mirza, D.F.; Perera, T.; Isaac, J.I.; Ferguson, J.; de Jonge, J.; Muiesan, P. Chronic kidney disease after liver transplantation: Impact of extended criteria grafts. Liver Transpl. 2019, 25, 922–933.
- Fabrizi, F.; Dixit, V.; Martin, P.; Messa, P. Pre-transplant kidney function predicts chronic kidney disease after liver transplant: Meta-analysis of observational studies. Dig. Dis. Sci. 2011, 56, 1282–1289.
- Kim, J.-Y.; Akalin, E.; Dikman, S.; Gagliardi, R.; Schiano, T.; Bromberg, J.; Murphy, B.; de Boccardo, G. The variable pathology of kidney disease after liver transplantation. Transplantation 2010, 89, 215–221.
- Kubal, C.; Cockwell, P.; Gunson, B.; Jesky, M.; Hanvesakul, R.; Dronavalli, V.; Bonser, R.S.; Neil, D. Chronic kidney disease after nonrenal solid organ transplantation: A histological assessment and utility of chronic allograft damage index scoring. Transplantation 2012, 93, 406–411.
- Chonchol, M.; Wachs, M.; Taylor, J.; Popovtzer, M.M. Should we biopsy kidneys of patients post-liver transplant? Transpl. Proc. 2003, 35, 3035–3038.
- Beloncle, F.; Sayegh, J.; Duveau, A.; Besson, V.; Croue, A.; Subra, J.-F.; Augusto, J.-F. An unexpected cause of progressive renal failure in a 66-year-old male after liver transplantation: Secondary hyperoxaluria. Int. Urol. Nephrol. 2013, 45, 1209–1213.
- Kamar, N.; Maaroufi, C.; Guilbeau-Frugier, C.; Servais, A.; Meas-Yedid, V.; Tack, I.; Thervet, E.; Cointault, O.; Esposito, L.; Guitard, J.; et al. Do kidney histology lesions predict long-term kidney function after liver transplantation? Clin. Transpl. 2012, 26, 927–934.
- Sharma, P.; Schaubel, D.E.; Guidinger, M.K.; Goodrich, N.P.; Ojo, A.O.; Merion, R.M. Impact of MELD-based allocation on end-stage renal disease after liver transplantation. Am. J. Transpl. 2011, 11, 2372–2378.
- Watt, K.D.S.; Pedersen, R.A.; Kremers, W.K.; Heimbach, J.K.; Charlton, M.R. Evolution of causes and risk factors for mortality post-liver transplant: Results of the NIDDK long-term follow-up study. Am. J. Transpl. 2010, 10, 1420–1427.
- Leithead, J.A.; Armstrong, M.J.; Corbett, C.; Andrew, M.; Kothari, C.; Gunson, B.K.; Muiesan, P.; Ferguson, J.W. Hepatic ischemia reperfusion injury is associated with acute kidney injury following donation after brain death liver transplantation. Transpl. Int. 2013, 26, 1116–1125.
- Boin, I.F.S.F.; de Ataide, E.C.; Dias, E.P.O.; Stucchi, R.S.B.; Seva-Pereira, T.; Calomeni, G.; Capel Junior, C.C.; Mazzali, M. Can pre-liver transplantation renal insufficiency using a creatinine clearance calculator predict long-term survival? Transpl. Proc. 2012, 44, 2452–2454.
- Wenger, U.; Neff, T.A.; Oberkofler, C.E.; Zimmermann, M.; Stehberger, P.A.; Scherrer, M.; Schuepbach, R.A.; Cottini, S.R.; Steiger, P.; Béchir, M. The relationship between preoperative creatinine clearance and outcomes for patients undergoing liver transplantation: A retrospective observational study. BMC Nephrol. 2013, 14, 37.
- Aberg, F.; Lempinen, M.; Hollmén, M.; Nordin, A.; Mäkisalo, H.; Isoniemi, H. Neutrophil gelatinase-associated lipocalin associated with irreversibility of pre-liver transplant kidney dysfunction. Clin. Transpl. 2014, 28, 869–876.
- Afonso, R.C.; Hidalgo, R.; Zurstrassen, M.P.V.C.; Fonseca, L.E.P.; Pandullo, F.L.; Rezende, M.B.; Meira-Filho, S.P.; Ferraz-Neto, B.H. Impact of renal failure on liver transplantation survival. Transpl. Proc. 2008, 40, 808–810.
- Bahirwani, R.; Campbell, M.S.; Siropaides, T.; Markmann, J.; Olthoff, K.; Shaked, A.; Bloom, R.D.; Reddy, K.R. Transplantation: Impact of pretransplant renal insufficiency. Liver Transpl. 2008, 14, 665–671.
- Bahirwani, R.; Forde, K.A.; Mu, Y.; Lin, F.; Reese, P.; Goldberg, D.; Abt, P.; Reddy, K.R.; Levine, M. End-stage renal disease after liver transplantation in patients with pre-transplant chronic kidney disease. Clin. Transpl. 2014, 28, 205–210.
- Braun, N.; Dette, S.; Viebahn, R. Impairment of renal function following liver transplantation. Transpl. Proc. 2003, 35, 1458–1460.
- Campbell, M.S.; Kotlyar, D.S.; Brensinger, C.M.; Lewis, J.D.; Shetty, K.; Bloom, R.D.; Markmann, J.F.; Olthoff, K.M.; Shaked, A.; Reddy, K.R. Renal function after orthotopic liver transplantation is predicted by duration of pretransplantation creatinine elevation. Liver Transpl. 2005, 11, 1048–1055.
- Fujinaga, K.; Usui, M.; Yamamoto, N.; Ishikawa, E.; Nakatani, A.; Kishiwada, M.; Mizuno, S.; Sakurai, H.; Tabata, M.; Isaji, S. Hypertension and hepatitis C virus infection are strong risk factors for developing late renal dysfunction after living donor liver transplantation: Significance of renal biopsy. Transpl. Proc. 2014, 46, 804–810.
- Lebrón Gallardo, M.; Herrera Gutierrez, M.E.; Seller Pérez, G.; Curiel Balsera, E.; Fernández Ortega, J.F.; Quesada García, G. Risk factors for renal dysfunction in the postoperative course of liver transplant. Liver Transpl. 2004, 10, 1379–1385.
- Israni, A.K.; Xiong, H.; Liu, J.; Salkowski, N.; Trotter, J.F.; Snyder, J.J.; Kasiske, B.L. Predicting end-stage renal disease after liver transplant. Am. J. Transpl. 2013, 13, 1782–1792.
- Levitsky, J.; Salomon, D.R.; Abecassis, M.; Langfelder, P.; Horvath, S.; Friedewald, J.; Wang, E.; Kurian, S.M.; Mondala, T.; Gil, S.; et al. Clinical and plasma proteomic markers correlating with chronic kidney disease after liver transplantation. Am. J. Transpl. 2011, 11, 1972–1978.
- Moreno, J.M.; Rubio, E.; Pons, F.; Velayos, B.; Navarrete, E.; Herreros de Tejada, A.; López-Monclús, J.; Sánchez-Turrión, V.; Cuervas-Mons, V. Usefulness of mycophenolate mofetil in patients with chronic renal insufficiency after liver transplantation. Transpl. Proc. 2003, 35, 715–717.
- Northup, P.G.; Argo, C.K.; Bakhru, M.R.; Schmitt, T.M.; Berg, C.L.; Rosner, M.H. Pretransplant predictors of recovery of renal function after liver transplantation. Liver Transpl. 2010, 16, 440–446.
- Ruebner, R.L.; Reese, P.P.; Abt, P.L. Donation after cardiac death liver transplantation is associated with increased risk of end-stage renal disease. Transpl. Int. 2014, 27, 1263–1271.
- Asfandiyar, S.; Abouljoud, M.; Kim, D.; Brown, K.; Yoshida, A.; Arenas, J.; Sherbondy, M.; Divine, G.; Moonka, D. Influence of hepatitis C on renal function after liver transplantation. Transpl. Proc. 2006, 38, 3643–3645.
- Milongo, D.; Bascands, J.-L.; Huart, A.; Esposito, L.; Breuil, B.; Moulos, P.; Siwy, J.; Ramírez-Torres, A.; Ribes, D.; Lavayssière, L.; et al. Pretransplant urinary proteome analysis does not predict development of chronic kidney disease after liver transplantation. Liver Int. 2015, 35, 1893–1901.
- Warnaar, N.; Mallett, S.V.; de Boer, M.T.; Rolando, N.; Burroughs, A.K.; Nijsten, M.W.N.; Slooff, M.J.H.; Rolles, K.; Porte, R.J. The impact of aprotinin on renal function after liver transplantation: An analysis of 1043 patients. Am. J. Transpl. 2007, 7, 2378–2387.
- Bilbao, I.; Charco, R.; Balsells, J.; Lazaro, J.L.; Hidalgo, E.; Llopart, L.; Murio, E.; Margarit, C. Risk factors for acute renal failure requiring dialysis after liver transplantation. Clin. Transpl. 1998, 12, 123–129.
- Hand, W.R.; Whiteley, J.R.; Epperson, T.I.; Tam, L.; Crego, H.; Wolf, B.; Chavin, K.D.; Taber, D.J. Hydroxyethyl starch and acute kidney injury in orthotopic liver transplantation: A single-center retrospective review. Anesth. Analg. 2015, 120, 619–626.
- Tinti, F.; Umbro, I.; Giannelli, V.; Merli, M.; Ginanni Corradini, S.; Rossi, M.; Nofroni, I.; Poli, L.; Berloco, P.B.; Mitterhofer, A.P. Acute renal failure in liver transplant recipients: Role of pretransplantation renal function and 1-year follow-up. Transpl. Proc. 2011, 43, 1136–1138.
- De Boer, J.D.; Blok, J.J.; Braat, A.E. Graft quality and prediction of outcome after liver transplantation. Transplantation 2017, 101, e286.
- Christians, U.; Klawitter, J.; Klawitter, J.; Brunner, N.; Schmitz, V. Biomarkers of immunosuppressant organ toxicity after transplantation: Status, concepts and misconceptions. Expert Opin. Drug Metab. Toxicol. 2011, 7, 175–200.
- Fagundes, C.; Pépin, M.-N.; Guevara, M.; Barreto, R.; Casals, G.; Solà, E.; Pereira, G.; Rodríguez, E.; Garcia, E.; Prado, V.; et al. Urinary neutrophil gelatinase-associated lipocalin as biomarker in the differential diagnosis of impairment of kidney function in cirrhosis. J. Hepatol. 2012, 57, 267–273.
- Verna, E.C.; Brown, R.S.; Farrand, E.; Pichardo, E.M.; Forster, C.S.; Sola-Del Valle, D.A.; Adkins, S.H.; Sise, M.E.; Oliver, J.A.; Radhakrishnan, J.; et al. Urinary neutrophil gelatinase-associated lipocalin predicts mortality and identifies acute kidney injury in cirrhosis. Dig. Dis. Sci. 2012, 57, 2362–2370.
- Singal, A.K.; Jackson, B.; Pereira, G.B.; Russ, K.B.; Fitzmorris, P.S.; Kakati, D.; Axley, P.; Ravi, S.; Seay, T.; Ramachandra Rao, S.P.; et al. Biomarkers of renal injury in cirrhosis: Association with acute kidney injury and recovery after liver transplantation. Nephron 2018, 138, 1–12.
- Kalisvaart, M.; Schlegel, A.; Umbro, I.; de Haan, J.E.; Polak, W.G.; IJzermans, J.N.; Mirza, D.F.; Perera, M.T.P.; Isaac, J.R.; Ferguson, J.; et al. The AKI Prediction Score: A new prediction model for acute kidney injury after liver transplantation. HPB 2019, 21, 1707–1717.
- O’Leary, J.G.; Levitsky, J.; Wong, F.; Nadim, M.K.; Charlton, M.; Kim, W.R. Protecting the kidney in liver transplant candidates: Practice-Based recommendations from the american society of transplantation liver and intestine community of practice. Am. J. Transpl. 2016, 16, 2516–2531.
- Segev, D.L.; Sozio, S.M.; Shin, E.J.; Nazarian, S.M.; Nathan, H.; Thuluvath, P.J.; Montgomery, R.A.; Cameron, A.M.; Maley, W.R. Steroid avoidance in liver transplantation: Meta-analysis and meta-regression of randomized trials. Liver Transpl. 2008, 14, 512–525.
- Sgourakis, G.; Radtke, A.; Fouzas, I.; Mylona, S.; Goumas, K.; Gockel, I.; Lang, H.; Karaliotas, C. Corticosteroid-free immunosuppression in liver transplantation: A meta-analysis and meta-regression of outcomes. Transpl. Int. 2009, 22, 892–905.
- Neal, D.A.; Tom, B.D.; Gimson, A.E.; Gibbs, P.; Alexander, G.J. Hyperuricemia, gout, and renal function after liver transplantation. Transplantation 2001, 72, 1689–1691.
- Durand, F.; Francoz, C.; Asrani, S.K.; Khemichian, S.; Pham, T.A.; Sung, R.S.; Genyk, Y.S.; Nadim, M.K. Acute kidney injury after liver transplantation. Transplantation 2018, 102, 1636–1649.
- Hmoud, B.; Kuo, Y.-F.; Wiesner, R.H.; Singal, A.K. Outcomes of liver transplantation alone after listing for simultaneous kidney: Comparison to simultaneous liver kidney transplantation. Transplantation 2015, 99, 823–828.
- Gonwa, T.A.; McBride, M.A.; Anderson, K.; Mai, M.L.; Wadei, H.; Ahsan, N. Continued influence of preoperative renal function on outcome of orthotopic liver transplant (OLTX) in the US: Where will MELD lead us? Am. J. Transpl. 2006, 6, 2651–2659.
- Schmitt, T.M.; Kumer, S.C.; Al-Osaimi, A.; Shah, N.; Argo, C.K.; Berg, C.; Pruett, T.L.; Northup, P.G. Combined liver-kidney and liver transplantation in patients with renal failure outcomes in the MELD era. Transpl. Int. 2009, 22, 876–883.
- Locke, J.E.; Warren, D.S.; Singer, A.L.; Segev, D.L.; Simpkins, C.E.; Maley, W.R.; Montgomery, R.A.; Danovitch, G.; Cameron, A.M. Declining outcomes in simultaneous liver-kidney transplantation in the MELD era: Ineffective usage of renal allografts. Transplantation 2008, 85, 935–942.
- Sharma, P.; Shu, X.; Schaubel, D.E.; Sung, R.S.; Magee, J.C. Propensity score-based survival benefit of simultaneous liver-kidney transplant over liver transplant alone for recipients with pretransplant renal dysfunction. Liver Transpl. 2016, 22, 71–79.
- Ekser, B.; Mangus, R.S.; Fridell, W.; Kubal, C.A.; Nagai, S.; Kinsella, S.B.; Bayt, D.R.; Bell, T.M.; Powelson, J.A.; Goggins, W.C.; et al. A novel approach in combined liver and kidney transplantation with long-term outcomes. Ann. Surg 2017, 265, 1000–1008.
- Yunhua, T.; Qiang, Z.; Lipeng, J.; Shanzhou, H.; Zebin, Z.; Fei, J.; Zhiheng, Z.; Linhe, W.; Weiqiang, J.; Dongping, W.; et al. Liver transplant recipients with end-stage renal disease largely benefit from kidney transplantation. Transpl. Proc. 2018, 50, 202–210.
- Taner, T.; Heimbach, J.K.; Rosen, C.B.; Nyberg, S.L.; Park, W.D.; Stegall, M.D. Decreased chronic cellular and antibody-mediated injury in the kidney following simultaneous liver-kidney transplantation. Kidney Int. 2016, 89, 909–917.
- Singal, A.K.; Ong, S.; Satapathy, S.K.; Kamath, P.S.; Wiesner, R.H. Simultaneous liver kidney transplantation. Transpl. Int. 2019, 32, 343–352.
