Deep eutectic solvents (DES) are eutectic mixtures that present a deviation from the ideal thermodynamic solid–liquid phase behavior, where a significant depression in the melting temperature occurs. If properly designed and chosen, DES may be liquid at room and the human body’s temperatures and display a biocompatible character, thus representing relevant options in the pharmaceutical field. Accordingly, DES have been studied as alternative solvents or in formulations of pharmaceuticals to improve their solubility and stability. Depending on the DES components, these mixtures might exhibit interesting biological activities compatible with several applications. The use of DES as functional agents or as novel liquid forms of active pharmaceutical ingredients (API-DES) with the goal of improving bioavailability, permeability and therapeutic efficacy of a given API stands as alternative strategies in the pharmaceutical field for drug delivery purposes.
- deep eutectic solvents
- active pharmaceutical ingredients
- solubility
- bioavailability
- therapeutic efficacy
- Introduction
The well-known drawbacks associated with solid forms of active pharmaceutical ingredients (APIs) has boosted the search for innovative drug formulations over the years [1]. These drawbacks encompass polymorphism, incomplete dissolution and low bioavailability, and, ultimately, treatment efficacy [2]. Attempting to overcome these limitations, several approaches based on eutectic mixtures and deep eutectic solvents (DES) have been proposed. A eutectic mixture or eutectic system corresponds to a homogeneous mixture of at least two compounds that melts or solidifies at a single temperature that is lower than the melting point of any of the constituents. The lowest possible melting temperature across all of the mixing ratios for the involved component species is known as the eutectic temperature. On the other hand, deep eutectic solvents correspond to eutectic mixtures, but present a strong deviation (negative or positive) from the ideal solid–liquid phase behavior.
Solid dispersion has been one of the most successful methods in improving pharmaceuticals properties; it is based on the drug’s dispersion in a biologically inert matrix prepared by melting or solvent evaporation methods [3], and was first introduced in the 1960s by Sekiguchi and Obi [4]. The authors demonstrated a faster oral absorption profile for sulfathiazole when prepared in a eutectic mixture comprising urea. After this proof of concept, many other APIs have been incorporated in eutectic mixtures and DES, i.e., by dissolving APIs in DES or by using DES in which at least one of the respective components is an API [5,6].
DES were introduced by Abbott et al. [7], in 2003, to describe mixtures of amides with quaternary ammonium salts, with melting temperatures far below those of their pure components and with strong deviations to the ideal solid–liquid phase behavior (Figure 1) [8]. The strong negative deviations observed for some DES can be enough for obtaining mixture compositions with melting temperatures far below room or the human body’s temperature [7]. After this pioneering work, several scientific works and several reviews addressing DES’s definition and related fundamental knowledge, and their applications, have been published [9–12].
DES require the mixture of at least two selected compounds, and can be prepared by heating, grinding, vacuum evaporation or freeze-drying methods [12]. These mixtures can be safely designed for pharmaceutical purposes, namely by the combination of compounds to which safety profiles are already well established and for which use in the pharmaceutical field is already recognized, and are able to be liquid at the temperatures of interest. Accordingly, the adequate selection of the compounds based on their physical–chemical properties, and of their ratio, may allow the tailoring of their solubilization and stabilization potential for a wide range of pharmaceuticals, as well as the creation of DES comprising APIs in their composition (API–DES), where the goal is to decrease the drug melting temperature. Table 1 summarizes some of the DES components and target pharmaceuticals studied up to date targeting these two possibilities.
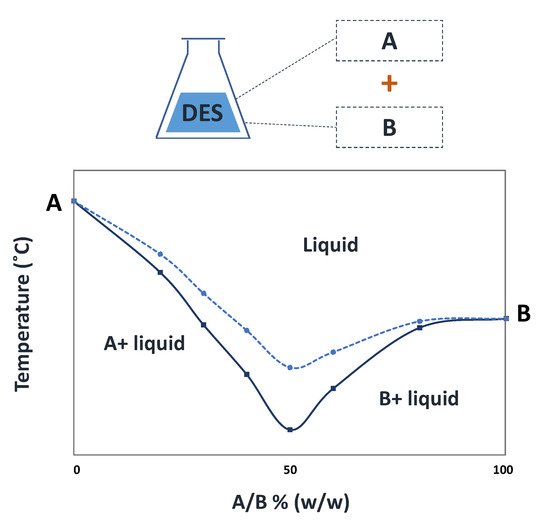 Figure 1. Solid-liquid phase diagram of a hypothetical DES (continuous line) and its comparison with the ideal behavior (dashed line).
Figure 1. Solid-liquid phase diagram of a hypothetical DES (continuous line) and its comparison with the ideal behavior (dashed line).
Solid-liquid phase diagram of a hypothetical DES (continuous line) and its comparison with the ideal behavior (dashed line).
| DES | Molar Ratio | API Solubilized | Ref |
|---|---|---|---|
| [Ch]Cl–urea | 1:2 | Piroxicam | [13] |
| Betaine–urea | 1:2 | Clavulanic acid | [14] |
| [Ch]Cl–lactic acid–water | 1:0.9:0.6 | Aprepitant | [13] |
| [Ch]Cl–1,2-propanediol | 1:2 | Aspirin | [15] |
| [Ch]Cl–ethyleneglycol | 1:2 | Naproxen | [16] |
| Betaine–glycerol–water | 1:2:1 | Indomethacin | [13] |
| [Ch]Cl–malic acid | 1:1 | Celecoxib | [16] |
| Camphor–menthol | 1:1 | Ibuprofen | [17] |
| [Ch]Cl–levulinic acid | 1:2 | Ketoprofen | [15] |
| Parent API | API–DES | Molar ratio | Ref |
| Aspirin | [Ch]Cl–aspirin | 1:2 | [18] |
| Ibuprofen | Ibuprofen–menthol | 1:3 | [19] |
| Ibuprofen | Ibuprofen–benzoic acid | 1:3 | [19] |
| Ibuprofen | Ibuprofen–phenylacetic acid | 1:2 | [19] |
| Ibuprofen | Ibuprofen–limonene | 1:8 | [20] |
| Ethambutol | Citric Acid–Ethambutol–water | 2:1:10 | [21] |
DES application as alternative media for API solubilization and API formulation into its liquid form by the API–DES approach.
|
DES |
Molar Ratio |
API Solubilized |
Ref |
|
[Ch]Cl–urea |
1:2 |
Piroxicam |
[13] |
|
Betaine–urea |
1:2 |
Clavulanic acid |
[14] |
|
[Ch]Cl–lactic acid–water |
1:0.9:0.6 |
Aprepitant |
[13] |
|
[Ch]Cl–1,2-propanediol |
1:2 |
Aspirin |
[15] |
|
[Ch]Cl–ethyleneglycol |
1:2 |
Naproxen |
[16] |
|
Betaine–glycerol–water |
1:2:1 |
Indomethacin |
[13] |
|
[Ch]Cl–malic acid |
1:1 |
Celecoxib |
[16] |
|
Camphor–menthol |
1:1 |
Ibuprofen |
[17] |
|
[Ch]Cl–levulinic acid |
1:2 |
Ketoprofen |
[15] |
|
Parent API |
API–DES |
Molar ratio |
Ref |
|
Aspirin |
[Ch]Cl–aspirin |
1:2 |
[18] |
|
Ibuprofen |
Ibuprofen–menthol |
1:3 |
[19] |
|
Ibuprofen |
Ibuprofen–benzoic acid |
1:3 |
[19] |
|
Ibuprofen |
Ibuprofen–phenylacetic acid |
1:2 |
[19] |
|
Ibuprofen |
Ibuprofen–limonene |
1:8 |
[20] |
|
Ethambutol |
Citric Acid–Ethambutol–water |
2:1:10 |
[21] |
Given the versatility of DES, they can be designed to improve APIs performance. Indeed, and as summarized in Figure 2, DES have been studied for applications in the pharmaceutical field, namely to improve the solubility, permeation and stability of APIs envisaging the development of more effective formulations and to produce new liquid forms of APIs (API–DES) [17,18,22]. Since organic solvents have been the first choice for a long time, and the number of acceptable solvents for pharmaceuticals is limited, with several solvent guides available nowadays [23], DES can also be designed to act as suitable benign alternatives within the pharmaceutical industry, i.e., in the APIs’ synthesis (including biocatalytic-mediated reactions), crystallization and solubilization [24]. On the other hand, the API–DES strategy is particularly advantageous for improving drug solubility while avoiding polymorphism concerns [25]. These liquid forms can even be composed of APIs and polymerizable monomers, offering new possibilities for polymer-based drug delivery systems [26].
The use of DES both as pharmaceutical solvents or as the API itself (using the API–DES approach) plays a key role in the design and development of effective drug delivery systems. DES have been used as media for polymerization processes, to solubilize biopolymers or change the materials properties, providing, for example, plasticizer or porosity enhancer effects or acting as functionalizing agents [27,28]. The numerous possibilities of design drug delivery systems brought by DES while considering their integration, allow researchers to simplify their development and improve therapeutic efficacy.
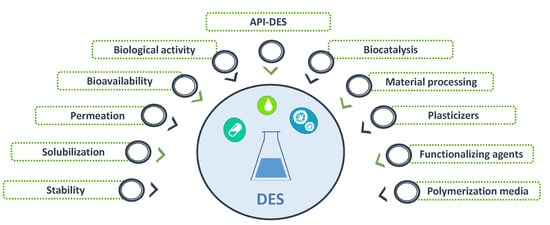 Figure 2. Different applications of DES within the pharmaceutical field.
Figure 2. Different applications of DES within the pharmaceutical field.
Different applications of DES within the pharmaceutical field.
Due to their advantages, in what concerns the advances brought by DES in drug formulation and delivery, some review papers and book chapters can be found [29–32] encouraging the expansion of the research in this area and contributing to the correct and rational development of these strategies. Of high interest are the recent advances achieved in the field of computational methods, which represent a step forward in understanding DES phase behavior and the underlying molecular-level mechanisms, permitting a better design of these mixtures for specific applications, while avoiding extensive trial and error methods [33,34]. Below, the main examples found of DES applications within the pharmaceutical field are provided and discussed.
- DES Applications within the Pharmaceutical Field
2.1. DES in Biocatalysis to Produce APIs Precursors
Biocatalysis is amongst the most promising technologies for the sustainable synthesis of APIs and their precursors, with high profit within the pharmaceutical sector [35]. Although many biocatalytic reactions can be carried out in aqueous media, the use of organic solvents is commonly required in the synthesis of pharmaceuticals [36,37]. However, to guarantee enzymatic activity, the adequate selection of organic solvents is required. As an alternative to the use of these common solvents, DES have shown promising results in improving the activity and selectivity, while presenting good yields.
Due to the possibility of preparing DES with more biocompatible features, DES have been studied, although briefly, as alternative co-solvents in enzyme-catalyzed reactions for the production of APIs precursors [38]. The study of aqueous solutions of DES, such as cholinium chloride ([Ch]Cl)–urea (1:2) and [Ch]Cl–glycerol (1:2), highlight the possibility to not only improve the structural and thermal stability of α-chymotrypsin while preserving its activity in aqueous media [39] but also enable reactions where hydrophobic and hydrophilic substrates need to be combined and where high selectivity for the peptide (100%) can be achieved [40].
DES have been studied as solvents and co-solvents to enhance the activity and stability of lipases in aqueous reactions, improving their enantioselectivity [41,42]. The activity of Candida rugosa lipase in the synthesis of p-nitrophenol, a model pharmaceutical intermediate, in aqueous solution was enhanced to 155% by using [Ch]Cl–urea–glycerol (1:1:1) as a cosolvent, when compared to the activity in phosphate buffer [41]. This improvement surpasses the lipase activity obtained with co-solvents such as glycerol, ethylene glycol, or even ILs in aqueous solutions, e.g., 1-butyl-3-methylimidazolium tetrafluoroborate. DES, especially glycerol-based, were shown to be capable of efficiently enhancing the activity, thermal, pH and storage stability of the lipase in aqueous solutions [41]. Given the wide variety of DES studied, the influence of these mixtures on the activity and stability of lipase was appraised by the solvent nature, addressed by the determination of solvatochromic parameters, namely dipolarity/polarizability, hydrogen bond acidity and hydrogen bond basicity. The thermal and storage stability of lipase in DES aqueous solutions was associated with the hydrogen bond acidity of DES mixtures; therefore, the stabilizing effect of DES mixtures on lipase may be caused by the strong hydrogen bond donating power of DES [41].
Enantioselectivity is of high pharmaceutical importance since different enantiomers may differ significantly in their biological effect, ranging from therapeutic to highly toxic. In this sense, lipases are commonly applied as chiral catalysts in the synthesis of various fine chemicals and APIs precursors. DES have also been successfully designed and applied in the kinetic resolution of (R,S)-1-phenylethyl acetate to produce f (R)-1-phenylethanol, a high-value API precursor [42]. The preparation of (R)-1-phenylethanol with Candida antarctica lipase B was studied in aqueous solutions of [Ch]Cl–glycerol (1:2) with 10, 30 and 50% of water. These mixtures allowed the increase in the stability of the enzyme over a one-month period, retaining 80% of its initial activity over 28 days. The presence of a high content of water in the DES may destroy the strong hydrogen-bonding network and compromise the DES structure, whereas lower amounts of water (<30%) could negatively influence hydrolysis. Therefore, solutions with approximately 50% of DES are preferential for this type of reaction. The yield of purification of (R)-1-phenylethanol was determined at a laboratory (81.2%) and a preparative (49.5%) scale by liquid–liquid extraction with ethyl acetate and [Ch]Cl–glycerol. The DES was successfully recycled and reused after biocatalysis up to 5 times, exhibiting only 35% yield decrease on the last cycle, in comparison to the initial reaction [42].
DES have been also applied as co-solvents on whole-cell biocatalysis to enhance the production of vanillin, a precursor in the manufacture of APIs [43]. The reaction catalyzed by Lysinibacillus fusiformis CGMCC1347 cells from isoeugenol was studied in a range of twenty-four DES in aqueous media. These co-solvents showed the ability to improve the production yields by up to 142% with the addition of relatively small amounts of DES (1% v/v in water) compared to the yields obtained in pure water. The immobilization of the Lysinibacillus fusiformis CGMCC1347 cells in PVA-alginate beads granted an augmented production yield in the presence of the DES [Ch]Cl–galactose (20% v/v), up to 181%, while allowing maintaining of the catalytic activity after being used for at least thirteen cycles.
The main results of the selected and discussed examples are summarized in Table 2, where the DES, enzyme used, API precursor, amount of DES and reaction yield are identified.
Table 2. Summary of the main results and conditions of cholinium ([Ch])-based DES used in biocatalysis for the production of APIs precursors.
|
DES |
Enzyme |
API Precursor |
Amount of DES (% v/v) |
Yield (%) |
Ref |
|
[Ch]Cl–urea |
Candida rugosa lipase 1 |
p-nitrophenol |
10 |
122.0 |
[41] |
|
[Ch]Cl–glycerol |
103.0 |
||||
|
[Ch]Cl–ethylene glycol |
90.0 |
||||
|
[Ch]Cl–urea–glycerol |
155.0 |
||||
|
[Ch]Cl–glycerol–ethylene glycol |
117.0 |
||||
|
[Ch]Cl–urea–thiourea |
120.0 |
||||
|
[Ch]Cl–formamide–thiourea |
83.0 |
||||
|
[Ch]Cl–glycerol |
Candida antarctica lipase B |
(R)-1-phenylethanol |
55 |
54.6 |
[42] |
|
[Ch]Cl–lactic acid |
Lysinibacillus Fusiformis 1 CGMCC1347 |
Vanillin |
20 |
98.9 |
[43] |
|
[Ch]Cl–citric acid |
58.1 |
||||
|
[Ch]Cl–ethylene glycol |
110.7 |
||||
|
[Ch]Cl–glycerol |
117.1 |
||||
|
[Ch]Cl–sorbitol |
125.6 |
||||
|
[Ch]Cl–xylose |
129.5 |
||||
|
[Ch]Cl–glucose |
126.7 |
||||
|
[Ch]Cl–galactose |
129.9 |
1 The activity of lipase in buffer without additive was defined as 100%, results relative to DES-free solution.
2.2. DES for APIs Solubilization
The correct choice of a solvent to assist the processing of materials and drug dissolution is of extreme importance in the development of pharmaceuticals and their formulations [44]. Although water is the most desirable solvent for pharmaceuticals, the vast majority of APIs display low-water solubility. Therefore, exploring alternative solvents to organic ones for the solubilization of these APIs that can meet the requirements and be accepted by the pharmaceutical industry remains a challenge. This challenge can be tackled by the use of more benign co-solvents, such as glycerol, propylene glycol and polyethylene glycol, among others [45]. However, it has been shown that solubility enhancements achieved by the use of these co-solvents can be surpassed by several orders of magnitude by the use of DES, as reported, for instance, with anti-inflammatory and antifungal drugs [15,45]. Such effects can be verified for the solubility enhancement achieved for ibuprofen (more than 5400-fold, Figure 3) when using [Ch]Cl–levulinic acid, compared to the API’s water solubility [15]. Contrarily, by solubilizing this drug in the mixture menthol–camphor (1:1) only a 4-fold increase in water solubility is achieved [17], highlighting the need for a screening when attempting to select the correct alternative solvent. The solubility of other anti-inflammatory drugs, such as naproxen and ketoprofen, can also be increased in comparison to its aqueous solubility by using DES (up to 740- and 960-fold, respectively) [15]. High solubility enhancements can additionally be obtained by adding a third component to the mixture, as happens for [Ch]Cl–glycolic acid by adding oxalic acid (1:1.6:0.4) (up to 53,600-fold as depicted in Figure 3) [46].
DES have been widely studied as alternative solvents for the solubility enhancement of anti-inflammatory [46], antipyretic [15], analgesic [47] and antifungal [46] drugs, as well as for the solubilization of nutraceuticals [48–50]. These mixtures enable a rapid onset of action with a significant increase in the drug’s bioavailability. More recently, studies have revealed the ability of DES to improve the oral absorption of target drugs and increase their blood concentration in in vivo studies [48,49].
Figure 3. Examples of experimental solubility enhancements achieved for anti-inflammatory and antifungal APIs using DES as alternative solvents in comparison with their solubility in water.
Computational methods have proven to be a powerful tool for studying DES’ solvation ability and related molecular-level mechanisms, and can be of high importance to uncover the best DES combinations to dissolve a specific API. This possibility was used to identify DES with high ability to solubilize rutin, by applying COSMO-RS [51]. The proposed model, based on the possible ionic and neutral forms of the constituents, was validated against the experimental solubility of rutin in fifteen DES. The results revealed that the most effective DES combination comprised proline and 2,3-diaminosuccinic acid. A DES with both components might enhance rutin’s solubility by 130% when compared to the reference solvent, proline–glutamic acid. The amino acids used in the DES creation affording the highest rutin solubility were all cyclic. The results obtained with DES comprising carboxylic acids allowed the conclusion that those with two carboxylic groups, two methylene groups and two amino substituents lead to higher rutin solubility. Such results were verified to be in accordance with the experimental data determined for rutin solubilization in DES media, previously addressed in a different study [49].
Similar works, i.e., while making use of computational methods, have been conducted to study the solubilization of anesthetic drugs such as lidocaine [33]. The solvation of lidocaine in [Ch]Cl–lactic acid (1:1) and alanine–lactic acid (1:1) was studied using density functional theory and molecular dynamics methods. The obtained results show that the solvation ability of these DES can be attributed to the strong solute–solvent intermolecular interactions accompanied by a slight volume expansion and minor solvent structural changes. The predicted solubilities reveal an enhancement of 104 to 105 in [Ch]Cl–lactic acid and alanine–lactic acid, respectively, when compared to the API’s aqueous solubility. In agreement with these findings, other [Ch]Cl-based DES have been studied regarding their ability to solubilize lidocaine taking advantage of computational data [52]. The results gathered, based on differences between orbital molecular energies, revealed that high solubility can be obtained by the establishment of hydrogen bonding between the API (NH site) and the chloride anion, as well as between the oxygen atoms of the hydroxyl groups present in the acids and the glycols of HBDs. Furthermore, the favorable electrostatic interactions between the API (CO site) with the cholinium cations and the hydrogen atoms attached to oxygen of acids and glycols are also responsible for this behavior. The lidocaine solubility has also been investigated in DES comprising other hydrogen bond acceptor species, rather than [Ch]Cl [53]. Furthermore, more benign components such as amino acid-based DES, namely arginine (arginine–glutamic acid, arginine–tartaric acid and arginine–oxalic acid; 1:1 molar ratio), were studied for the same purpose [53]. The same DES have been applied for the solubilization of anesthetic drugs, such as bupivacaine, prilocaine and procaine [54]. Despite the clear advantage in using organic acids as HBDs for anesthetic drugs’ solubilization, the selection of compounds such as oxalic acid must be avoided due to the compound’s toxicity, and more benign alternatives should be explored.
The results reported up to date show how the solubility of APIs in a DES can be controlled by its proper design, which may interact with relevant sites in the pharmacological compound, leading to suitable pharmacological solubilization and where computational methods can be of high advantage.
2.3. DES to Improve APIs Stability
Drug stability is usually referred to as the ability of the drug to preserve its form in a given environment, e.g., in biological conditions [55]. Several factors influence drug stability, such as structural or external factors (light, temperature, pH, oxidation or enzymes). For instance, many ester-containing APIs, such as aspirin, can undergo hydrolysis upon a long storage period in water [56]. Even though the use of organic solvents could avoid the water-mediated decomposition, this might not be a suitable alternative for pharmaceutical formulations. In addition to the solubility improvements discussed before, DES have shown to be promising solvents to enhance the chemical stability of APIs, such as aspirin, in comparison with their stability in aqueous media [15]. As an example, the cleavage of aspirin into salicylic and acetic acids is 8.2 times slower in the DES [Ch]Cl–1,2-propanediol (1:2) than in an aqueous solution, and the cleavage rate can be decreased by at least 3 times with the use of a DES aqueous solution at 50% (w/w), at high temperatures (80 °C). In the same line, β-lactam antibiotics can be very unstable as the β-lactam ring opening in an aqueous medium leads to degradation, resulting in antimicrobial activity loss [14]. To overcome this drawback, the DES betaine–urea (1:2) with 2% (w/w) of water was studied to improve the stability of imipenem and clavulanic acid. These formulations enhanced the antibiotics stability by 7-fold and 2.5-fold, respectively, compared to water in a 7-day storage period at room temperature [14].
DES also allow the prevention of thermal and light degradation of pharmaceuticals. As an example, porphyrins display photophysical properties attractive for their application in photodynamic therapy [57]. However, their poor photostability limits their application as photosensitizers in the treatment of bacterial infections [58,59]. The photostability of the neutral porphyrin 5,10,15,20-tetrakis(4-hydroxyphenyl)-porphyrin (THPP) was studied in citric acid, [Ch]Cl and glucose-based DES, and compared to their stability in organic media after 8 h of irradiation [60]. The rate of porphyrin degradation was significantly higher in methanol than in the neat DES; however, upon dilution of the DES porphyrin solution in water (1:50), the profile of degradation was inverted. However, it should be kept in mind that the application of mixtures such as citric acid–glucose is still too controversial to be considered as a DES due to the degradation of the components during the DES preparation, namely by oxidation of the carbohydrate in acidic media [61].
In addition to porphyrins, curcumin can also be applied as a photosensitizer [62]. Furthermore, due to its valuable antioxidant, anti-inflammatory, antimicrobial and anti-tumoral properties, other applications can be envisaged [63]. The poor solubility of this API and its high photo and thermal sensitivity, however, limit their research. By storing curcumin in DES media, namely [Ch]Cl–glycerol (1:2), it is possible to preserve the API stability over 2 h even when exposing the solution to sunlight, while, when stored in methanol in the same conditions, the concentration of curcumin decreases to only 5% of its initial amount [64].
DES can decrease or prevent the degradation of therapeutic proteins [65]. Due to their thermal sensitivity, most of these biological products require a cold-chain system during shipping, storage and handling processes to maintain their therapeutic activity [66], which results in increased costs while limiting their application [67]. To overcome these drawbacks, DES have been used, showing a promising ability to improve the thermal stability of pharma proteins. The stability of chondroitinase ABCI, an important clinical enzyme in the treatment of spinal lesions, has been studied in DES aqueous solutions [68]. To this end, the extent of inactivation in the presence and absence of 20% (w/w) of [Ch]Cl–glycerol (1:2) and betaine–glycerol (1:2) at −20 °C, 4 °C, and 37 °C was investigated. When using aqueous DES, the enzyme activity was retained above 95% and 80% in [Ch]Cl–glycerol and betaine–glycerol, respectively, over 15 days at −20 °C. On the other hand, in its absence the activity was lost after 5 days in aqueous media at the same temperature conditions. At 4 °C, a 6.5-fold increase in the stability was obtained in betaine–glycerol in comparison with the enzyme storage in aqueous buffer. Based on fluorescence studies, it has been observed that a more compact enzyme structure can be verified in [Ch]Cl–glycerol than in betaine–glycerol and in phosphate buffer [68].
An increase in the stability of human interferon-α2 (IFN-α2), a therapeutic protein used in the treatment of hepatitis B and C and leukemia, was verified using DES [69]. Based on the protein activity and structure analyses, the use of the DES [Ch]Cl–fructose (1:1) as a main solvent increases the stability of IFN-α2 for the short-term (2h) and long-term (3 months) storage periods at 37, 50 and 70 °C, when compared to its solubilization in phosphate buffer. High temperatures were considered in this work aiming to highlight the ability of DES to be used as temperature-stable media that can bypass the need for cold-chain systems during the shipping, storage and handling of therapeutic proteins. Structural analyses confirmed that the protein keeps its structural integrity and activity when long-term stored in the DES at 37 °C [69].
Despite the promising results achieved with the use of DES to improve drug stability, as summarized in Table 3, more extensive data are still needed so that their design can be accomplished. The variety of DES studied to this purpose is still limited and the impact of the variation of their molar ratio is unknown. Further studies are required to better understand the DES–protein interactions that trigger these structural differences and different preservation ability. In the case of solid APIs, short-term storage studies have been majorly conducted. Furthermore, a particular concentration of DES in aqueous media, or the use of the neat DES, have been investigated, with no comprehensive investigation on the most suitable DES–water–API formulation.
Table 3. Drug stability improvement in DES media under different storage conditions.
|
API |
Reference Solvent |
DES |
Storage Conditions |
Stability Improvement in DES Media |
Ref |
|
Chemical stability |
|||||
|
Aspirin |
Water |
[Ch]Cl–1,2-propanediol |
14 h at 80 °C |
Cleavage into salicylic and acetic acids is 8.2 times slower |
[15] |
|
Imipenem |
Water |
Betaine–urea |
7-day storage at 25 °C |
7-fold stability improvement |
[14] |
|
Clavulanic acid |
Water |
2.5-fold stability improvement |
|||
|
Light stability |
|||||
|
5,10,15,20-tetrakis(4-hydroxyphenyl)-porphyrin (THPP) |
Methanol |
Citric acid–glucose |
3 to 5 h exposure to 765 W∙m−2 (310–800 nm) irradiation to an endpoint of 8 h corresponding to 1.2 × 106 lux∙h (400–800 nm) |
Lower rate of photodegradation |
[60] |
|
Curcumin |
Methanol |
[Ch]Cl–glycerol |
2 h exposure to sunlight |
Preserved stability |
[64] |
|
Thermal stability |
|||||
|
Chondroitinase ABCI |
Phosphate buffer |
[Ch]Cl–glycerol Betaine–glycerol |
15 days storage at −20 °C |
Enzyme activity retention of 95% and 80%, respectively, vs loss of activity after 5 days in its absence |
[68] |
|
Human |
Phosphate buffer |
[Ch]Cl–fructose |
Short-term (2 h) and long-term (3 months) storage at 37 °C |
Preservation of structural integrity and activity |
[69] |
2.4. DES with Biological Activity
Due to the variety of possible DES and component combinations, they may be designed to incorporate compounds with biological activity. Despite this, the possibility has still not been explored greatly that the combination of a DES with biological activity can be potentially beneficial in conjugation with a given API. To this purpose it is important to know and understand the activity of each DES. Up to now, DES have been reported to present antimicrobial, antioxidant and anti-tumoral activities, as summarized in Table 4.
The antimicrobial activity of a variety of [Ch]Cl-based DES has been evaluated against Gram-positive (Staphylococcus aureus and Listeria monocytogenes) and Gram-negative (Escherichia coli and Salmonella enteritidis) bacteria [70]. Given the range of DES investigated, it is possible to verify that amine-, alcohol- and sugar-based DES are not so effective for bacteria eradication since these components can be used as nitrogen or carbon nutrient sources. On the other hand, it has been shown that the selection of DES with organic acids can lead to bacterial growth inhibition, which is also a result of the pH decrease [70–72]. DES with high acidity or basicity can indeed denature proteins located on the cell wall, resulting in cell collapse and death [70].
Table 4. DES’s biological activity and respective microorganisms and cell lines used in their study.
|
DES |
Molar Ratio |
Microorganism/Cell Line |
Ref |
|
Antibacterial activity |
|||
|
[Ch]Cl–urea |
1:2 |
E. coli S. enteritidis S. aureus L. moncytogenes |
[70] |
|
[Ch]Cl–acetamide |
|||
|
[Ch]Cl–ethylene glycol |
|||
|
[Ch]Cl–glycerol |
|||
|
[Ch]Cl–triethylene glycol |
|||
|
[Ch]Cl–xylitol |
1:1 |
||
|
[Ch]Cl–D-sorbitol |
|||
|
[Ch]Cl–xylose/water |
1:1:1 |
||
|
[Ch]Cl–sucrose/water |
5:2: |
||
|
[Ch]Cl–fructose/water |
5:2:5 |
||
|
[Ch]Cl–glucose/water |
|||
|
[Ch]Cl–p-toluenesulfonic acid |
1:1 |
||
|
[Ch]Cl–oxalic acid |
1:1 |
||
|
[Ch]Cl–levulinic acid |
1:2 |
||
|
[Ch]Cl–malonic acid |
1:1 |
||
|
[Ch]Cl–malic acid |
|||
|
[Ch]Cl–citric acid |
|||
|
[Ch]Cl–tartaric acid |
2:1 |
||
|
Caprylic acid–myristic acid |
3:1 |
E. coli P. aeruginosa |
[73] |
|
Caprylic acid–stearic acid |
4:1 |
||
|
Caprylic acid–lauric acid |
2:1 |
S. aureus MRSA |
|
|
Antifungal activity |
|||
|
[Ch]Cl–zinc chloride |
1:2 |
P. chrysosporium A. niger L. tigrinus C. cylindracea |
[74] |
|
[Ch]Cl–malonic acid |
1:1 |
||
|
[Ch]Cl–p-toluenesulfonic acid |
1:3 |
||
|
[Ch]Cl–urea |
1:2 |
||
|
[Ch]Cl–glycerol |
1:2 |
||
|
[Ch]Cl–ethylene glycol |
1:3 |
||
|
[Ch]Cl–diethylene glycol |
1:2 |
||
|
[Ch]Cl–triethylene glycol |
1:3 |
||
|
[Ch]Cl–fructose |
2:1 |
||
|
[Ch]Cl–glucose |
|||
|
Anti-tumoral activity |
|||
|
[Ch]Cl–glycerol |
1:3 |
Human prostate cancer (PC3); Human malignant melanoma (A375); Human colon adenocarcinoma (HT29); Human breast cancer (MCF-7) |
[75] |
|
[Ch]Cl–ethylene glycol |
|||
|
[Ch]Cl–urea |
|||
|
[Ch]Cl–triethylene glycol |
|||
|
[Ch]Cl–fructose |
5:2 |
Human cervical cancer (HelaS3); |
[76] |
|
[Ch]Cl–glucose |
|||
|
[Ch]Cl–sucrose |
4:1 |
||
|
[Ch]Cl–glycerol |
1:2 |
||
|
[Ch]Cl–malonic acid |
1:1 |
||
DES based only on saturated fatty acids, namely capric acid, myristic acid, lauric acid and stearic acid have been studied as well, showing antimicrobial properties against a broad spectrum of microorganisms [73]. Capric acid–lauric acid (2:1) presented the highest antimicrobial activity against Gram-positive bacteria such as Escherichia coli and the fungal pathogen Candida albicans. This DES can be potentially effective against the biofilm formation of Escherichia coli, being capable to remove it without the need of additional physical forces.
DES can also present effects on other fungal species rather than Candida albicans, such as Phanerochaete chrysosporium, Aspergillus niger, Lentinus tigrinus and Candida cylindracea [74]. To this purpose, cholinium-based DES with alcohols, sugars, organic acids, urea and zinc chloride have been studied for their antifungal activity based on the inhibition growth. Although zinc chloride, malonic acid and p-toluenesulfonic acid-based DES are those with higher inhibition ability, it was found that their action is very similar to that obtained with the respective single components. On the other hand, an interesting behavior was observed with [Ch]Cl–urea since none of the singular components present antifungal activity. It was shown that the activity of this DES is a result of a positive synergistic effect favorable for the growth inhibition of Candida cylindracea [74].
The anti-tumoral potential of DES has been explored in vitro in several tumoral cell lines [71,75]. Cholinium chloride combined with different hydrogen bond donors, namely glycerol, ethylene glycol, triethylene glycol and urea were investigated regarding their effect on human prostate cancer (PC3), human malignant melanoma (A375), human colon adenocarcinoma (HT29) and human breast cancer (MCF-7) cell lines [75]. The investigated DES inhibited cancer cell growth at certain dosages (11–70 μg·mL−1), presenting low cell line selectivity depending on the DES composition. A375, HT29 and MCF-7 cell lines were shown to be more susceptible to [Ch]Cl–triethylene glycol and less to [Ch]Cl–urea, whereas PC3 cells were more resistant to the DES [Ch]Cl–ethylene glycol. All of these DES present, in a dose dependent manner, the ability to provoke cell death and increase reactive oxygen species (ROS) production in cancer cell lines. The anti-tumoral activity of the studied DES followed the trend: [Ch]Cl–triethylene glycol < [Ch]Cl–glycerol < [Ch]Cl–ethylene glycol < [Ch]Cl–urea for MCF-7, A375 and HT29. In terms of selectivity, [Ch]Cl–glycerol was more selective against MCF-7 and A375, whereas [Ch]Cl–triethylene glycol showed selectivity towards MCF-7, PC3 and HT29. These DES did not cause DNA damage but enhanced ROS production and induced apoptosis in treated cancer cells. However, in vivo administration studies in mice reveal that the dose concentration for administration should be carefully manipulated to avoid the toxicity to healthy tissue/organs. Sugar- and malonic acid-based DES have also been studied on MCF-7, along with human cervical cancer (HelaS3), human ovarian cancer (CaOV3) and mouse skin cancer (B16F10) cell lines [76]. This DES anti-tumoral activity followed the trend: [Ch]Cl–malonic acid > [Ch]Cl–sucrose > [Ch]Cl–fructose > [Ch]Cl–glucose > [Ch]Cl–glycerol for HelaS3, MCF-7, and B16F10. In the case of CaOV3, [Ch]Cl–glucose presented higher activity than [Ch]Cl–fructose, resulting in the trend: [Ch]Cl–malonic acid > [Ch]Cl–sucrose > [Ch]Cl–glucose > [Ch]Cl–fructose > [Ch]Cl–glycerol. Overall, all cell lines presented higher susceptibility to the DES [Ch]Cl–malonic acid. This behavior, as previously stated, can be attributed to the pH decrease, but also to the ability of malonic acid to stall several biochemical pathways within the cellular environment, contributing to cancer cell apoptosis. However, due to the toxicity associated with this organic acid for several microorganisms and cell lines, its use and concentration needs to be carefully assessed. In vitro studies of these DES in cell lines and in vivo assessment of the DES toxicity in mice reveal an anti-tumoral activity related to the DES viscosity and to an increase in the membrane porosity and redox stress [76,77]. To understand this increase in membrane porosity and the cytotoxicity associated with some DES, computational methodologies, such as COMO-RS, have been applied to simulate the interactions between DES and cellular membranes [76]. To this end a series of phospholipids were modeled and their interactions with DES were examined. DES seem to strongly interact with cell surfaces, which might possibly accumulate and/or aggregate according with the DES components. This accumulation and aggregation may lead to cellular demise through reduced growth [76]. Similar studies with [Ch]Cl- and N,N-diethylammonium chloride-based DES reveal similar trends to those observed for ILs since the alkyl chain length difference seems to have a major impact on the DES biological activity [78]. Since the increase in the alkyl chain influences hydrophobicity, as it occurs in many ILs, it leads to an increase in the membrane permeability and, subsequently, cell death. As previously stated, the biological activity of DES is strongly influenced by the selected components. Thus, selecting hydrophobic salts as an alternative to organic acids appears to stimulate hydrophobicity, whereas amine and alcohol components for this purpose have a negligible effect.
In addition to their antimicrobial and anti-tumoral activity, DES have proved to have antioxidant activity. Despite the recent application of these solvents to improve the antioxidant activity of natural extracts, the antioxidant potential of some DES themselves is less explored [79,80]. Studies have verified that DES usually present antioxidant activity if one of their components also presents antioxidant potential [71]. Cholinium-based DES with glycerol, urea or ethylene glycol, for example, do not present antioxidant activity, whereas betaine-based DES with compounds such as malic acid and proline can act as radical scavengers [71,75]. DES containing antioxidant compounds retained the antioxidant activity, following the trend: betaine–malic acid–proline > betaine–malic acid–glucose > citric acid–proline > betaine–glucose ≈ citric acid–glucose–glycerol ≈ citric acid–fructose–glycerol [71]. This trend verifies the possibility to tune the biological action of these solvents and, since the inclusion of certain compounds (e.g., amino acids, organic acids and phenolic compounds, etc.) can grant a specific biological activity to the solvent, they can be envisaged to potentiate the pharmaceutical action of a given API or nutraceutical.
2.5. API-DES Formulations
DES can be designed to comprise the API as a DES constituent aiming for a liquid form of the drug, following the API-DES strategy [18], also addressed in literature as therapeutic deep eutectic solvents (THEDES) [22]. The proper selection of the second component plays a critical role in the formation of an API–DES liquid form (at least at the human body temperature) and on the resulting therapeutic properties. These liquid forms can be obtained by the combination of APIs with a wide variety of compounds, namely metabolites (e.g., amino acids, vitamins, alcohols or organic acids) or permeation enhancers (e.g., menthol and fatty acids, among others) [18,81,82]. API–DES can also be prepared by the selection of two different APIs, resulting in dual function liquid forms[47]. These mixtures can additionally present a polymerizable character when comprising APIs with polymerizable moieties, further allowing the tuning of the delivery profile [26]. Figure 4 summarizes these API–DES strategies.
Figure 4. Possible API–DES strategies according with the forming components selection.
Most API–DES reported to date exhibit melting temperatures near or below the human body’s temperature and usually envisage topical and oral administration [18,83,84]. Initially, the majority of these liquid forms were designed for transdermal purposes and included permeation enhancers, such as terpenes and fatty acids [19,85,86]. In 1998, Stott and co-workers [83] reported a series of API–DES based on ibuprofen and different permeation enhancers, such as L-menthol, L-menthone thymol, D-limonene, 1,8-cineole and p-cymene. The described mixtures present melting temperatures below body temperature, and, since the recrystallization of the API at lower temperatures can be avoided, the API stability under storage could be potentially improved. Due to its relevance, a significant number of works are related to the characterization and drug delivery application of the DES menthol–ibuprofen (Tm = 13 °C) [22,83]. The solubility of ibuprofen in aqueous media can be increased 12-fold by converting the API into its liquid form with menthol [19]. Furthermore, this API–DES enables the improvement by 3-fold of the skin permeability of ibuprofen when compared to the pure API.
A relevant example, taking advantage of the DES biological activity modulation ability while using APIs like ibuprofen in the API–DES strategy, is the recent exploration of the anti-tumoral potential of limonene–ibuprofen (1:4) [20]. Limonene presents reported anti-tumoral activity; however, its toxicity towards healthy cells restrains its wider application. The formulation of these active ingredients into an API–DES enables the inhibition of HT29 proliferation without significant cell toxicity associated. The study of the anticancer properties of limonene–ibuprofen (1:4) revealed that the API–DES presents a different mechanism of action than the individual components, highlighting the synergic potential of this API–DES [20].
More recently, the search for API–DES aiming for oral application has increased, with this strategy improving the API’s solubility and bioavailability while avoiding a drug’s polymorphism. These API–DES for oral administration generally employ two different APIs or an API and a metabolite-derived compound, and the resulting melting temperatures are far below the body’s temperature [18,21]. To date, the lack of molecular-level understanding to better identify the most suitable second component that will result in liquid API–DES, and to rely only on heuristic decisions, has shortened and delayed the research on promising liquid forms of APIs. The application of predictive models to this purpose, that take into account intermolecular interactions and provide melting temperature and melting enthalpy insights, can be a promising tool to start the screening of those components that are the most suitable to be combined with a given API [34,87]. To this purpose, the functional group activity coefficients (UNIFAC(Do)) thermodynamic model has been applied for the screening of compounds to pair with lidocaine, ibuprofen and phenylacetic acid, in which thymol, vanillin, lauric acid, p-methylbenzoic acid, benzoic acid and cinnamic acid have been considered [87]. The results obtained allow us to conclude that the component combination should be selected according with the following rules: the second component melting temperature should be similar to that of the API; the melting enthalpy of the second component should be as low as possible; the thermodynamic activity coefficients of the API and of the second component should be as low as possible over the entire composition range. From the studied compounds, the most suitable combinations with lidocaine can be obtained selecting lauric acid, thymol and ibuprofen for a dual action API–DES [87].
The application of COSMO-RS can be helpful to scan a wide variety of combinations aimed at identifying the most promising to obtain a liquid mixture at a given temperature [34]. In this sense, the possibility of a combination of [Ch]Cl with acetylsalicylic acid, ibuprofen, ketoprofen and paracetamol was explored [34]. The predictions obtained through COSMO-RS were fairly accurate, revealing that the proposed mixtures would present melting temperatures above 40 °C (with a mean average error of 6 °C). From the studied options, [Ch]Cl–ibuprofen seems to present the highest deviation from the predicted eutectic composition, showing a good agreement with experimental data [34].
The impact of ionic and non-ionic excipients on API–DES formation was also investigated attempting to understand what type of compounds should be preferably selected. To this purpose, thymol, coumarin and quaternary ammonium chloride salts were studied in combination with acetylsalicylic acid, acetaminophen, ibuprofen, ketoprofen and lidocaine [88]. By using COSMO-RS, it was possible to predict the solid–liquid equilibrium phase diagrams of the API and excipients mixtures. Based on the same diagrams, it was possible to verify that quaternary ammonium chloride salts, such as tetraalkylammonium chlorides, do not allow temperature depressions (from the melting temperature of the API) in the same degree as the non-ionic compounds studied. Regarding the use of non-ionic excipients, while the systems containing coumarin follow a quasi-ideal behavior, the strong interactions between these APIs and thymol lead to negative deviations to thermodynamic ideality [88]. Despite the study of non-ionic excipients by computational methods being seen as a promising tool to be considered for the design of API–DES formulations, more experimental data on this topic is still necessary.
Despite these promising results, the study of API–DES is in its infancy and fundamental parameters, such as drug solubility, dissolution rate, bioavailability, cytotoxicity and therapeutic efficacy need to be evaluated, while also addressing in vivo studies so that their application in the pharmaceutical field can become a reality.
2.6. DES in Drug Delivery Systems
In the area of drug delivery, DES have been applied as novel solvents, as novel API formulations (API–DES) or as agents with specific activity that can fit the needs for the design of drug delivery systems in several routes of administration [89–91]. These mixtures have been conjugated with different polymers and biopolymers producing different drug delivery systems, such as hydrogels, particles and nanofibers, among others [90–92]. Figure 5 summarizes the DES’ application in drug delivery systems and their function in the development of the systems and therapeutic action.
The possibility of preparing API–DES with a polymerizable component character stands out as an appealing alternative for the development of drug delivery systems. In this field, the API–DES exerts multiple actions by providing the API for drug release, acting as the monomer and being itself the solvent media for the polymerization process [26,93]. These mixtures are considered conventional DES, being liquid at low temperatures; nevertheless, upon polymerization, the DES concept is lost due to the development of a new polymer-based delivery system with an API incorporated in the matrix. Despite their significant potential, more profound research into and characterization of these mixtures is still required to enable a more detailed understanding and design of these drug delivery systems.
Figure 5. Schematic representation of the type of DES-based drug delivery systems developed (left) and the DES function in the design and efficacy of these systems (right).
DES have been mainly studied as vehicles for topical applications. In vivo studies on albino rabbits have confirmed that topical application of DES, such as capric acid–menthol, do not cause skin irritation [94]. The use of these systems for the solubilization of fluconazole and mometasone, antifungal and anti-allergic drugs, respectively, and their formulation and application as a topical cream has been studied as well [94]. It was found that the drug, the DES and cream components do not cause skin edema or inflammation after topical application.
The use of API–DES in transdermal drug delivery systems was recently explored with the combination of rotigotine, used in the treatment of Parkinson’s disease, with lactic acid, aiming to avoid the drug’s first-pass metabolism [89]. This API–DES was incorporated in a silicone pressure sensitive adhesive with high hydroxyl group content and its drug loading was investigated by an in vitro skin permeation study, whereas the optimized patch was evaluated by pharmacokinetics studies. The formulation of the drug into an API–DES allowed improvement of not only the drug skin permeability but also the drug–polymer miscibility, thus improving the transdermal drug delivery process. In addition, the in vivo pharmacokinetic study showed that the optimized formulation presented a comparable pharmacokinetic behavior with the commercial product [89].
A more extensive study of DES has enabled different administration routes to be considered, as is the case of using these mixtures for nasal drug delivery [90,92]. The correct selection of DES based on properties such as melting temperature and viscosity can be an advantage when considering the drug delivery application. For example, the low melting temperature of the mixture of [Ch]Cl and malic acid (−59.1 °C), its high viscosity and ability to solubilize insulin are appealing properties for the preparation of controlled released systems that can be compared to insulin hydrogels based on sodium carboxymethylcellulose [90]. The DES is not only capable of preserving the insulin structure but also enables a near-zero order kinetic release of the drug in vitro. Most insulin in the upper phase of the DES media is released by diffusion into aqueous media, with a fast release profile before 1 h and with a slower release after this point. The in vivo study of insulin penetration across nasal mucosal epithelium after administration was assessed for the formulations with the DES and the carboxymethylcellulose-based hydrogels. DES could enhance the nasal absorption of insulin significantly in comparison with the cellulose-based hydrogels. Additionally, the hypoglycemic trends of the DES-based formulations of insulin after nasal administration were found to be similar to those obtained by subcutaneous insulin administration; the residence time of insulin at the administration site was improved by the DES due to its high viscosity [90]. Additionally, the possibility to combine DES with several techniques such as supercritical CO2 (SC-CO2) can be beneficial for the development of drug delivery systems compliant with the nasal administration [92]. Aqueous solutions of DES (70–80% w/w), namely citric acid–arginine (1:1), were studied aiming to develop an alternative treatment for tuberculosis. For this purpose, glycerol monostearate was used as a model carrier to encapsulate DES aqueous solutions by using the particle from gas saturated solutions (PGSS) technique. The phase equilibrium study of DES solutions and supercritical CO2 allowed the selection of particles from the gas saturated solution method for encapsulation of the DES, achieving an encapsulation efficiency of 75%. The obtained particles exhibited a fast release profile dependent on the DES concentration in the aqueous solution and ranged from 0 to 5 h of complete release. Furthermore, in vitro studies on cell viability in L929 fibroblasts have shown that the prepared particles were non-cytotoxic [92].
Given the DES’ solvation ability, these mixtures can also be advantageous in the processing and dissolution of biopolymers, as reported for agar [95], chitin [96] and starch [22]. Due to their biocompatible and versatile character, upon the biopolymer’s dissolution in DES media, they can be directly applied as delivery systems [92,93]. The use of these solvents has proven to exert a plasticizer and porosity enhancer effect on the resulting delivery systems [27,28]. If well designed, the inclusion of these solvents in the delivery system can be beneficial for the overall properties and allow the tuning of the API’s release profile. In this sense, DES have been used in the preparation of several drug delivery systems and have proven to be able to be applied in different (bio)polymer-based drug delivery systems. Due to the versatility of DES design and application, these mixtures can be incorporated into polymer or biopolymer-based systems, and can even be used as drug vehicles for direct oral administration [49,50 91].
Polymer-based nanofibers prepared from DES media have been reported as fast-dissolving drug delivery systems that could potentially be applied as oral ulcer stickers [91]. The DES [Ch]Cl–mannose (2:1) was used as media to solubilize the polymer poly(vinyl alcohol) (PVA) for the preparation of the nanofibers through electrospinning. Given the therapeutic purpose of these systems, acetylsalicylic acid, selected as a model drug, and honey were added due to the anti-inflammatory and antibacterial action of both compounds, respectively. The nanofiber materials presented a rapid dissolution in artificial saliva and a significant antibacterial against E. coli and S. aureus (circa 37% bacterial reduction). Moreover, in vivo studies proved that the PVA–DES–honey nanofibers improved the wound healing rate (85.2%) on rat skin after 6 days of surgery, in comparison to the control PVA (68.2%) and PVA–DES nanofibers (76.3%) [91].
In addition to nanofibers, ion gel systems comprising DES and monomers such as 2-hydroxyethyl methacrylate (HEMA) have also been explored [97]. The DES [Ch]Cl–ascorbic acid was used not only to solubilize sunitinib malate, a drug used in the treatment of gastrointestinal stromal tumors, but also to allow the polymerization of HEMA at room temperature. The obtained ion gels were stable over a 6-month period with a pH-dependent release profile and presented no significant toxicity towards healthy or cancer cells. The release of the API in simulated stomach fluid (pH 1.2) is faster than that observed for simulated intestinal fluid (pH 6.8) and simulated blood fluid (pH 7.4) and, for a longer time period [97], as depicted in Figure 5.
From a different perspective, the use of these mixtures as functionalizing agents has been recently investigated for the delivery of anticancer agents. The use of DES in this context aims to substitute conventional functionalizing agents and improve the anti-tumoral activity of functionalized over non-functionalized graphene materials [98]. Doxorubicin has been loaded onto DES-functionalized graphene nanomaterials using aqueous solutions of DES, namely as [Ch]Cl–sucrose (4:1) and [Ch]Cl–glycerol (1:2) [99]. The results obtained exhibited significant ability to enhance the drug entrapment efficiency (EE ≈ 51%) and drug loading capacity (DLC ≈ 25%) for doxorubicin in comparison with the unfunctionalized graphene (EE ≈ 39%, DLC ≈ 19%). Furthermore, the use of [Ch]Cl–sucrose as a functionalizing agent exhibited higher anticancer activity and higher selectivity against MCF-7 cells than [Ch]Cl–glycerol, illustrating the potential application of this DES in drug delivery systems as a functionalizing agent [99].
Despite all of the promising results described, pharmacokinetic and pharmacodynamic studies are essential to evaluate the DES performance in combination with other compounds such as (bio)polymers in the drug delivery context. Data on the therapeutic efficacy on the intended target is still insufficient and must be further acquired for the expansion of these novel therapeutics while envisioning their latter pharmaceutical approval.
- Conclusions and Future Perspectives
Due to the acceptance and commercialization, already, of eutectic mixtures within the pharmaceutical industry, as is the case of the commercialized cream ELMA that is a mixture of lidocaine–prilocaine, DES represent a promising option to improve drugs’ characteristics and their therapeutic action and delivery. The possibility of using DES as alternative solvents and co-solvents in the production of APIs precursors, to improve the solubility and stability of APIs and to improve the biological activity of pharmaceutical formulations offers these mixtures a high advantage in this field, where they can be ultimately applied in drug delivery systems. Additionally, these mixtures can be used as novel liquid forms of APIs (API–DES) presenting all the DES advantages and allowing for higher therapeutic efficacy.
Despite having been only recently addressed in the literature for the preparation of API’s precursors, the use of DES in biocatalysis represents a step forward in the development of more sustainable and effective strategies for APIs synthesis. The verified possibility to recover and reuse DES without compromising the efficacy of the reactions reinforces the advantageous use of these mixtures to this purpose while taking advantage of their designer solvents ability. However, features such as eco/cytotoxicity and biodegradability, combined with life-cycle and technoeconomic analyses, are essential to support the application of DES at a larger scale. Furthermore, as already addressed for the use of organic solvents in the field of APIs and APIs precursors synthesis, the amount of residual DES in the final product must be quantified and limited in order to guarantee the safety of the synthesized intermediates.
The remarkable solubilization ability of DES for a variety of APIs (up to 53,600-fold), combined with the expected increased bioavailability, support their application in drug formulations and synthesis, particularly with the goal of replacing less benign volatile organic solvents. However, these formulations require, as any other techniques, the assessment of their final cytotoxicity. Some of the more recent studies on this area are starting to screen aqueous solutions of DES instead of pure mixtures, and to understand their impact on the solubilization mechanisms. This type of fundamental study, along with the recent development of predictive models that can be applied to select the most relevant DES for a specific API solubilization, is key towards their application in the pharmaceutical field and commercialization. In addition to the reported solubility enhancement, DES have been highlighted for their ability to improve the chemical and physical stability of APIs in short- and long-term storage. These mixtures enable the prevention of degradation reactions that are commonly observed in water, resulting in the stabilization of the drug in the DES media. In the future, the application of DES as alternative solvents and co-solvents for API solubilization should be accompanied by the study of the API stability in the new formulation.
DES can display biological activities, which, despite their relevance per se, can be designed to be incorporated in pharmaceutical formulations to provide a particular effect or dual therapeutic/biological action. So far, DES have been studied in vitro regarding their antimicrobial, anti-tumoral and antioxidant activities, being mainly reported for cholinium-based mixtures. To expand this area of research, it is necessary to study more DES combinations and understand their interactions with biological membranes. Research on the affinities between chaotropic and kosmotropic agents in DES can be a promising tool, not only for the prediction of the toxicity of DES but also to forecast their biological activity. Furthermore, the use of the pure mixture without an API or a delivery vehicle can potentially increase their toxicity towards healthy cells. To this purpose, the combination of DES with biological activity with a specific API and a targeted delivery system should be considered.
The API–DES strategy appears to be an appealing alternative to avoid drug polymorphism and enhance drug solubility and permeation through biological membranes while exerting single or even dual therapeutic action. Despite their wider application for transdermal delivery, advances in this field have enabled the application of these liquid API forms in oral and nasal administrations. However, insufficient information on their phase diagrams and stability over time are still a drawback. The use of predictive models will allow researchers to select the best DES components that will result in true API–DES with melting temperatures below the body’s temperature. Future studies are expected to include the therapeutic action of API–DES at the target along with bioavailability, dissolution, skin permeation and irritancy tests. Before considering clinical assays that are several years ahead, in vitro and model in vivo applications of API–DES formulations should be first considered and priority should be given to these assays.
The combination of DES and API–DES formulations with polymers and biopolymers has allowed us to expand the possibilities of enhancing the delivery of APIs. Due to the ability of DES to increase the solubility of APIs and biopolymers in aqueous media, they have successfully allowed new administration routes and different types of materials to be prepared. Regardless of the potential of DES in this field, there is still an insufficient number of works to fully understand the interaction of DES with polymers and biopolymers that could contribute to the conscious development of more effective drug delivery systems. In the future, stimulus-responsive systems, comprising DES and API–DES, such as pH and temperature-driven systems, are expected to be developed.
There is a wide range of opportunities to apply DES in the pharmaceutical field, for which the already reported promising studies will continue to motivate researchers to go further to increase their vast implementation in different applications.
