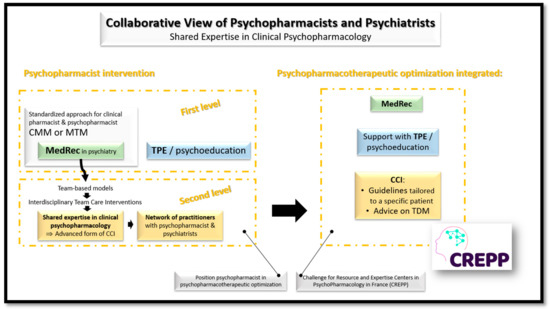
Although clinical pharmacy is a discipline that emerged in the 1960s, the question of precisely how pharmacists can play a role in therapeutic optimization remains unanswered. In the field of mental health, psychiatric pharmacists are increasingly involved in medication reconciliation and therapeutic patient education (or psychoeducation) to improve medication management and enhance medication adherence, respectively. However, psychiatric pharmacists must now assume a growing role in team-based models of care and engage in shared expertise in psychopharmacology in order to truly invest in therapeutic optimization of psychotropics.
- clinical pharmacy
- mental health
- psychiatry
- expertise
- psychopharmacology
1. Introduction
Twenty-five years ago, the ESCP questioned how clinical pharmacists could play a role in optimizing pharmacotherapy [6][1]. Three scenarios have been proposed for describing the position of the clinical pharmacist and named "clerk", "controller" and "care manager". Only the last one referred to a proactive model, centered on the patient with a real partnership with physicians, and appeared to be the most desirable scenario for the future of clinical pharmacy [6][1].
However, in psychiatry, it clearly appears that knowledge in psychopharmacology is paramount to the quality of clinical practice and thus, pharmacists could be privileged interlocutors for forging a link between pharmacological knowledge and clinical practice. This connection between clinical pharmacology and clinical pharmacy had been thought of by the pioneers of this discipline—Paul Parker (pharmacist) and Charles Walton (pharmacologist)—and was still later relayed by another father of the discipline, Russell R Miller [2].
While recent publications continue to demonstrate the interest and scalability of clinical pharmacy in psychiatry [4,8,9[3][4][5][6],10], its deployment continues to be held back for various reasons [3,4,11,12][7][3][8][9].
2. Medication Reconciliation Process in Psychiatry
3. Global Collaborative View of Psychiatric Pharmacists and Psychiatrists
4. Conclusions
References
- Leufkens, H.; Hekster, Y.; Hudson, S. Scenario analysis of the future of clinical pharmacy. Pharm. World Sci. 1997, 19, 182–185.
- Miller, R.R. History of clinical pharmacy and clinical pharmacology. J. Clin. Pharmacol. 1981, 21, 195–197.
- Javelot, H.; Dizet, S.; Straczek, C.; Langrée, B.; Michel, B.; Haffen, E.; Bertschy, G. Enhancing the role played by clinical pharmacists in psychiatric settings to better integrate clinical psychopharmacology into the decision-making process. Therapie 2021, 76, 149–156.
- Elbe, D.; Chapman, A. Formal Psychiatry Resident Rotations with a Clinical Pharmacy Specialist: Preliminary Experience at BC Children’s Hospital. J. Can. Acad. Child. Adolesc. Psychiatry 2019, 28, 7–8.
- Mohiuddin, A.K. Psychiatric Pharmacy: New Role of Pharmacists in Mental Health. Sch. J. Psychol. Behav. Sci. 2019, 2, 219–223.
- Macdonald, O.; Smith, K.; Marven, M.; Broughton, N.; Geddes, J.; Cipriani, A. How pharmacist prescribers can help meet the mental health consequences of COVID-19. Evid. Based Ment. Health 2020, 23, 131–132.
- Tanty, A.; Dantigny, R.; Bardet, J.D.; Chanoine, S.; Bedouch, P.; Allenet, B. French hospital clinical pharmacy: An identity crisis? Ann. Pharm. Fr. 2021, 79, 431–439.
- Goldstone, L.W.; DiPaula, B.A.; Caballero, J.; Park, S.H.; Price, C.; Zasadzki Slater, M. Improving medication-related outcomes for patients with psychiatric and neurologic disorders: Value of psychiatric pharmacists as part of the health care team. Ment. Health Clin. 2015, 5, 1–28.
- Rubio-Valera, M.; Chen, T.F.; O’Reilly, C.L. New roles for pharmacists in community mental health care: A narrative review. Int. J. Environ. Res. Public Health 2014, 11, 10967–10990.
- Dizet, S.; Varnier, V. La conciliation médicamenteuse en psychiatrie. Medication conciliation in psychiatry. Santé Mentale 2016, Août, 38–40.
- Mekonnen, A.B.; McLachlan, A.J.; Brien, J.A.E. Effectiveness of pharmacist-led medication reconciliation programmes on clinical outcomes at hospital transitions: A systematic review and meta-analysis. BMJ Open 2016, 6, e010003.
- Paton, C.; McIntyre, S.; Bhatti, S.F.; Shingleton-Smith, A.; Gray, R.; Gerrett, D.; Barnes, T.R.E. Medicines Reconciliation on Admission to Inpatient Psychiatric Care: Findings from a UK Quality Improvement Programme. Ther. Adv. Psychopharmacol. 2011, 1, 101–110.
- Brownlie, K.; Schneider, C.; Culliford, R.; Fox, C.; Boukouvalas, A.; Willan, C.; Maidment, I.D. Medication reconciliation by a pharmacy technician in a mental health assessment unit. Int. J. Clin. Pharm. 2014, 36, 303–309.
- Keers, R.N.; Williams, S.D.; Vattakatuchery, J.J.; Brown, P.; Miller, J.; Prescott, L.; Darren, M.; Ashcroft, D.M. Prevalence, nature and predictors of prescribing errors in mental health hospitals: A prospective multicentre study. BMJ Open 2014, 4, e006084.
- Noblot-Rossignol, M.; Vailleau, J.L.; Hamad, M.; Denis, F.; Beye, F. Conciliation des traitements médicamenteux à l’admission: Expérimentation en établissement de santé mentale et éligibilité des patients pouvant en bénéficier en priorité. Pharm. Hosp. Clin. 2017, 52, 177–185.
- Leherle, A.; Kowal, C.; Toulemon, Z.; Dalle-Pecal, M.; Pelissolo, A.; Leboyer, M.; Paul, M.; Diviné, C. Is the medication reconciliation achievable and relevant in Psychiatry?: Feedback on the implementation of medication reconciliation on hospital admission. Ann. Pharm. Fr. 2020, 78, 252–263.
- Choi, S.J.; Storey, R.; Parikh, S.V.; Bostwick, J.R. The Impact of Completing Medication Reconciliation and Depression Treatment History in an Outpatient Depression Clinic. Psychopharmacol. Bull. 2019, 49, 44–55.
- Keers, R.N.; Williams, S.D.; Vattakatuchery, J.J.; Brown, P.; Miller, J.; Prescott, L.; Ashcroft, D.M. Medication safety at the interface: Evaluating risks associated with discharge prescriptions from mental health hospitals. J. Clin. Pharm. Ther. 2015, 40, 645–654.
- Austin, Z.; Gregory, P.A.; Martin, J.C. Negotiation of interprofessional culture shock: The experiences of pharmacists who become physicians. J. Interprof. Care 2007, 21, 83–93.
- Yeung, E.Y.H. Pharmacists Becoming Physicians: For Better or Worse? Pharmacy 2018, 6, 71.
