A catalog of
BARD1
germline mutations/pathogenic variants (PVs) identified in large cumulative cohorts of ~48,700 breast cancer (BC) and ~20,800 ovarian cancer (OC) cases prepared based on 123 studies published over 20 years of
BARD1
gene screening. By comparing the frequency of
BARD1
PVs in the cases and ~134,100 noncancer controls from the gnomAD database, the effect of the
BARD1
PVs on BC and OC risks is estimated.
- BARD1,
- mutation
- breast cancer
- ovarian cancer
- cancer risk
1. Definition
Over the last two decades, numerous BARD1 mutations/pathogenic variants (PVs) have been found in patients with breast cancer (BC) and ovarian cancer (OC). However, their role in BC and OC susceptibility remains controversial, and strong evidence-based guidelines for carriers are not yet available.
2. Introduction
InhOverited genetic factors are responsible for a substantial portion of breast cancer (BC) and ovarian cancer (OC) cases. Multigene panel testing has revealed that germline loss-of-functionthe last two decades, numerous BARD1 mutations/pathogenic variants (PVs) in various cancer-associated genes are identified in more than 10% and 20% of patients with BC and OC, respectivelyhave [1][2][3]. Attempts have been made to define the genetic/familial risk of BC/OC associated with these genes, and subsequently, management recommendations for carriers of PVs in some of the high-penetrance genes have been established [4][5]. Despite this, several genes iound in patien which PVs confer low- or moderate-penetrance effects still require more evidence and more convincing assessments of BC/OC risk to utilize them in recommendations for carriers. A group of genes with insufficient and/or conflicting data includes the BRCA1-s with breassociatedt RING domain 1 (BARD1) gene.
The BARD1 gene encodes a protein of 777 amino acids with several functional domains, including an N-terminal RING-finger domain, three ankyrin repeats (ANK), and two C-terminal BRCT domains. The protein shows structural homology with BRCA1 within the BRCT and RING-finger domains, and through the latter domains, the two proteins form a stable heterodimer. The BARD1-BRCA1 heterodimer has E3 ubiquitin ligase activity and acts in multiple cellular processes essential for maintaining genomic stability, including DNA double-strand break repair through homologous recombination [6][7][8]ncer (BC) and ovarian cancer (OC). In additiHon to the well-established role of the BARD1-BRCA1 heterodimer, the BRCA1-independent function of BARD1 as a tumor suppressor has also been postulated, for example, in mediating p53-dependent apoptosis [9]. On the other hand, seweveral BARD1 isoforms resulting from alternative splicing that lack RING-finger and/or ANK domains were upregulated in different cancers and are suggested to have an oncogenic effect by antagonizing the function of full-length BARD1 [10][11][12][13].
Because of the abovementioned BARD1 functions, many mutation screening studies have been carried out to explore the role of BARD1 heir role in BC and OC susceptibility. As a result, hundreds of PVs were detected, mostly through the use of high-throughput next-generation sequencing (NGS; panel sequencing) in recent years. However, the PVs are scattered among many articles, which prevents the drawing of more comprehensive conclusions about their distribution over the gene, identification of recurrent PVs, and estimation of a more precise effect on cancer risk. In addition, despite multiple examples of BARD1 PVs in BC/OC patientsmains controversial, attempts to link PVs with BC/OC risk are often inconclusive and are usually not supported by statistically convincing pieces of ed strong evidence. However, these types of studies are justified due to reduced mutation penetrance and various interactions between the gene and other genetic, personal, and environmental factors. The lack of proper functional characterization of PVs and the genetic heterogeneity in different populations may be additional factors of insufficient and/or conflicting data. In addition, due to the low frequency of BARD1 PV-based guidelines (<1%), the sample sizes of the studies are still too modest to achieve sufficient statistical power, although the sizes are constantly increasing. Additionally, as the cost of whole gene testing is still relatively high and association case-control studies relying on the use of geographically matched controls are still very rare [14][15][16][17]. Therefore, coor carriers are ntrols from publicly available databases are frequently used to assess the risk, allowing to increase the study size and to improve statistical power [3][18][19][20]. Cosegregt yet availation studies can provide additional evidence for or against the association, although they may be challenging for low or moderate penetrance PVs, especially because large families with multiple BC/OC cases are becoming less availablele.
2. Introduction
To overcome the limitations mentioned above, the
BARD1
BARD1
have been cataloged
BARD1 have been determined with high confidence.
3. BARD1 Mutational Spectrum
In total, 144
BARD1
BARD1 detected in the BC and OC cohorts, as well as in population controls, is presented in Figure 1.
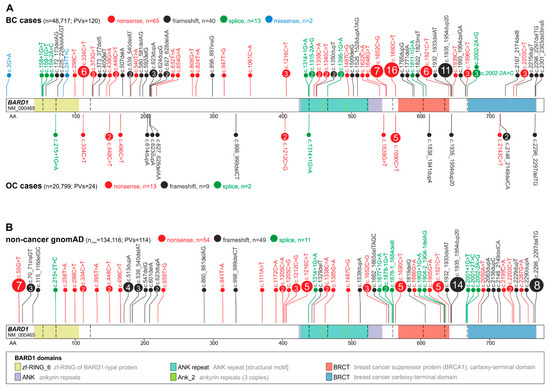
Figure 1.
BARD1
BARD1
A
B) PVs reported in noncancer gnomAD controls. The total number of detected PVs and the total number of cases and controls tested for the variants are indicated in parentheses; note that the total number of tested subjects differs substantially between groups.
Although
BARD1 PVs in BC and OC patients are distributed over the entire coding sequence, there are two regions of increased density of PVs, i.e., from exons 2 to ~230AA in exon 4, overlapping the RING-finger domain and from exon 5 to exon 10, overlapping the ANK repeat and BRCT I domains.
In the BC cohort, 10 of the PVs were identified in three or more cases (defined here as recurrent), with the highest occurrence of c.1690C>T (Q564*), c.1935_1954dup20 (E652Vfs*69), c.1652C>G (S551*), c.334C>T (R112*), and c.1921C>T (R641*) reported in 16, 11, 7, 6, and 6 cases, respectively. R112* and R641* recurrent PVs were identified in both Caucasian and Asian populations, while the remaining PVs, including the most frequent, Q564* and E652Vfs*69, were identified only in the Caucasian population. None of the recurrent PVs were specific to the Asian population. Interestingly, 10 out of 16 Q564* PVs were reported by studies analyzing mainly patients with a family history of BC/OC. Only one recurrent PV, i.e., Q564*, was reported in the OC cohort (five patients). In population controls, an additional recurrent PV was observed (not identified in BC/OC cohorts), i.e., c.55G>T (E19*). However, the PV was characteristic only for the Latino population, which represents a small proportion of the entire population of BC/OC cohorts.
4. Association of BARD1 Pathogenic Variants with Breast Cancer
The prevalence of
BARD1
p
BARD1
p
p
p = 0.0012 for Asians). The calculation was repeated excluding the three large studies from the analysis, which reported results of multigene testing of samples tested in diagnostic companies [22][23][24], as some small fractions of these samples may represent unrecognized duplicates of patients analyzed in other studies. Excluding these studies did not change the risk estimates substantially (OR = 3.14; 95% CIs:2.41–4.09;
p
p < 0.0001).
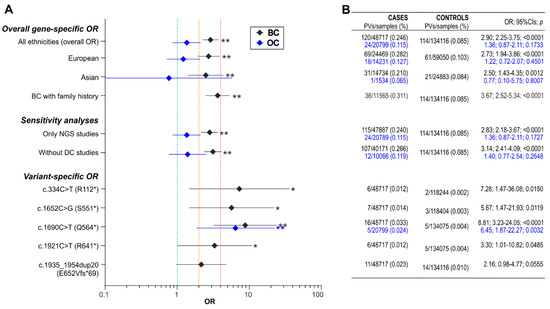
Figure 2.
BARD1
A
p
B
p-values (the values correspond to the particular OR symbols shown in the graph on the left).
The prevalence of
BARD1
p
BARD1
see Figure 2 for detailed analysis).
Funding
This work was supported by grants from the Polish National Science Centre (NCN 2015/17/B/NZ2/01182).Acknowledgments
The authors would like to thank the Genome Aggregation Database (gnomAD) and the groups that provided exome and genome variant data to this resource. A full list of contributing groups can be found at http://gnomad.broadinstitute.org/about.Author affiliations
Piotr Kozlowski & Malwina Suszynska, Department of Molecular Genetics, Institute of Bioorganic Chemistry, Polish Academy of Sciences, Noskowskiego 12/14 Street, 61-704, Poznan, PolandReferences
1.Suszynska, M.; Klonowska, K.; Jasinska, A.J.; Kozlowski, P. Large-scale meta-analysis of mutations identifiedin panels of breast/ovarian cancer-related genes—Providing evidence of cancer predisposition genes.Gynecol. Oncol.2019,153, 452–462.
2.Walsh, T.; Casadei, S.; Lee, M.K.; Pennil, C.C.; Nord, A.S.; Thornton, A.M.; Roeb, W.; Agnew, K.J.; Stray, S.M.;Wickramanayake, A.; et al. Mutations in 12 genes for inherited ovarian, fallopian tube, and peritonealcarcinoma identified by massively parallel sequencing.Proc. Natl. Acad. Sci. USA2011,108, 18032–18037.
3.Couch, F.J.; Shimelis, H.; Hu, C.; Hart, S.N.; Polley, E.C.; Na, J.; Hallberg, E.; Moore, R.; Thomas, A.;Lilyquist, J.; et al. Associations Between Cancer Predisposition Testing Panel Genes and Breast Cancer.JAMA Oncol.2017,3, 1190–1196.
4.Daly, M.B.; Pilarski, R.; Yurgelun, M.B.; Berry, M.P.; Buys, S.S.; Dickson, P.; Domchek, S.M.; Elkhanany, A.;Friedman, S.; Garber, J.E.; et al. NCCN Guidelines Insights: Genetic/Familial High-Risk Assessment: Breast,Ovarian, and Pancreatic, Version 1.2020.J. Natl. Compr. Canc. Netw.2020,18, 380–391.
5.Daly, M.B.; Pilarski, R.; Berry, M.; Buys, S.S.; Farmer, M.; Friedman, S.; Garber, J.E.; Kauff, N.D.; Khan, S.;Klein, C.; et al. NCCN Guidelines Insights: Genetic/Familial High-Risk Assessment: Breast and Ovarian,Version 2.2017.J. Natl. Compr. Canc. Netw.2017,15, 9–20.
6.Hashizume, R.; Fukuda, M.; Maeda, I.; Nishikawa, H.; Oyake, D.; Yabuki, Y.; Ogata, H.; Ohta, T. The RINGheterodimer BRCA1-BARD1 is a ubiquitin ligase inactivated by a breast cancer-derived mutation.J. Biol. Chem.2001,276, 14537–14540.
7.Irminger-Finger, I.; Ratajska, M.; Pilyugin, M. New concepts on BARD1: Regulator of BRCA pathways andbeyond.Int. J. Biochem. Cell Biol.2016,72, 1–17.
8.Tarsounas, M.; Sung, P. The antitumorigenic roles of BRCA1-BARD1 in DNA repair and replication.Nat. Rev.Mol. Cell Biol.2020,21, 284–299.
9.Irminger-Finger, I.; Leung, W.C.; Li, J.; Dubois-Dauphin, M.; Harb, J.; Feki, A.; Jefford, C.E.; Soriano, J.V.;Jaconi, M.; Montesano, R.; et al. Identification of BARD1 as mediator between proapoptotic stress andp53-dependent apoptosis.Mol. Cell2001,8, 1255–1266.
10.Cimmino, F.; Formicola, D.; Capasso, M. Dualistic Role of BARD1 in Cancer.Genes2017,8, 375.
11.Li, L.; Ryser, S.; Dizin, E.; Pils, D.; Krainer, M.; Jefford, C.E.; Bertoni, F.; Zeillinger, R.; Irminger-Finger, I.Oncogenic BARD1 isoforms expressed in gynecological cancers.Cancer Res.2007,67, 11876–11885.
12.Zhang, Y.Q.; Bianco, A.; Malkinson, A.M.; Leoni, V.P.; Frau, G.; De Rosa, N.; Andre, P.A.; Versace, R.;Boulvain, M.; Laurent, G.J.; et al. BARD1: An independent predictor of survival in non-small cell lung cancer.Int. J. Cancer2012,131, 83–94.
13.Bosse, K.R.; Diskin, S.J.; Cole, K.A.; Wood, A.C.; Schnepp, R.W.; Norris, G.; Nguyen le, B.; Jagannathan, J.;Laquaglia, M.; Winter, C.; et al. Common variation at BARD1 results in the expression of an oncogenicisoform that influences neuroblastoma susceptibility and oncogenicity.Cancer Res.2012,72, 2068–2078.
14.Suszynska, M.; Kluzniak, W.; Wokolorczyk, D.; Jakubowska, A.; Huzarski, T.; Gronwald, J.; Debniak, T.;Szwiec, M.; Ratajska, M.; Klonowska, K.; et al. BARD1 is A Low/Moderate Breast Cancer Risk Gene: EvidenceBased on An Association Study of the Central European p.Q564X Recurrent Mutation.Cancers2019,11, 740.
15.Weber-Lassalle, N.; Borde, J.; Weber-Lassalle, K.; Horvath, J.; Niederacher, D.; Arnold, N.; Kaulfuss, S.;Ernst, C.; Paul, V.G.; Honisch, E.; et al. Germline loss-of-function variants in the BARD1 gene are associatedwith early-onset familial breast cancer but not ovarian cancer.Breast Cancer Res.2019,21, 55.
16.Ramus, S.J.; Song, H.; Dicks, E.; Tyrer, J.P.; Rosenthal, A.N.; Intermaggio, M.P.; Fraser, L.; Gentry-Maharaj, A.;Hayward, J.; Philpott, S.; et al. Germline Mutations in the BRIP1, BARD1, PALB2, and NBN Genes in WomenWith Ovarian Cancer.J. Natl. Cancer Inst.2015,107, djv214.
17.Lu, H.M.; Li, S.; Black, M.H.; Lee, S.; Hoiness, R.; Wu, S.; Mu, W.; Huether, R.; Chen, J.; Sridhar, S.; et al.Association of Breast and Ovarian Cancers With Predisposition Genes Identified by Large-Scale Sequencing.JAMA Oncol2019,5, 51–57. [CrossRef]
18.Lilyquist, J.; LaDuca, H.; Polley, E.; Davis, B.T.; Shimelis, H.; Hu, C.; Hart, S.N.; Dolinsky, J.S.; Couch, F.J.;Goldgar, D.E. Frequency of mutations in a large series of clinically ascertained ovarian cancer cases tested onmulti-gene panels compared to reference controls.Gynecol. Oncol.2017,147, 375–380.
19.Norquist, B.M.; Harrell, M.I.; Brady, M.F.; Walsh, T.; Lee, M.K.; Gulsuner, S.; Bernards, S.S.; Casadei, S.; Yi, Q.;Burger, R.A.; et al. Inherited Mutations in Women With Ovarian Carcinoma.JAMA Oncol.2016,2, 482–490.
20.Slavin, T.P.; Maxwell, K.N.; Lilyquist, J.; Vijai, J.; Neuhausen, S.L.; Hart, S.N.; Ravichandran, V.; Thomas, T.;Maria, A.; Villano, D.; et al. The contribution of pathogenic variants in breast cancer susceptibility genes tofamilial breast cancer risk.NPJ Breast Cancer2017,3, 22.
21.Karczewski, K.J.; Francioli, L.C.; Tiao, G.; Cummings, B.B.; Alfoldi, J.; Wang, Q.; Collins, R.L.; Laricchia, K.M.;Ganna, A.; Birnbaum, D.P.; et al. The mutational constraint spectrum quantified from variation in 141,456humans.Nature2020,581, 434–443.
22.Tung, N.; Battelli, C.; Allen, B.; Kaldate, R.; Bhatnagar, S.; Bowles, K.; Timms, K.; Garber, J.E.; Herold, C.;Ellisen, L.; et al. Frequency of mutations in individuals with breast cancer referred for BRCA1 and BRCA2testing using next-generation sequencing with a 25-gene panel.Cancer2015,121, 25–33.
23.Susswein, L.R.; Marshall, M.L.; Nusbaum, R.; Vogel Postula, K.J.; Weissman, S.M.; Yackowski, L.; Vaccari, E.M.;Bissonnette, J.; Booker, J.K.; Cremona, M.L.; et al. Pathogenic and likely pathogenic variant prevalenceamong the first 10,000 patients referred for next-generation cancer panel testing.Genet. Med.2016,18,823–832.
24.LaDuca, H.; Stuenkel, A.J.; Dolinsky, J.S.; Keiles, S.; Tandy, S.; Pesaran, T.; Chen, E.; Gau, C.L.; Palmaer, E.;Shoaepour, K.; et al. Utilization of multigene panels in hereditary cancer predisposition testing: Analysis ofmore than 2,000 patients.Genet. Med.2014,16, 830–837.
