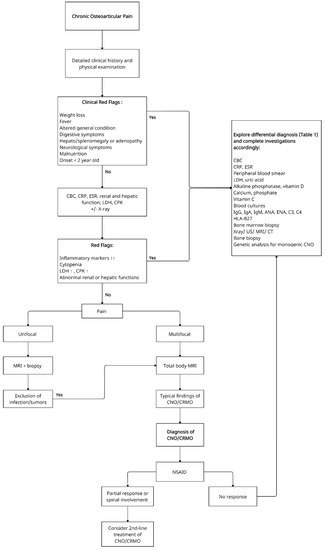
Chronic nonbacterial osteomyelitis (CNO) is an auto-inflammatory bone disorder with a wide spectrum of clinical manifestations, from unifocal to multifocal lesions. When it manifests with multifocal lesions, it is also referred to as chronic recurrent multifocal osteomyelitis (CRMO). CNO/CRMO can affect all age groups, with the pediatric population being the most common. Patients may present with systemic inflammation, but there is no pathognomonic laboratory finding. Magnetic resonance imaging (MRI) is the gold standard radiological tool for diagnosis. In the absence of validated diagnostic criteria, CNO/CRMO remains an exclusion diagnosis. Bone biopsy does not show a specific disease pattern, but it may be necessary in unifocal or atypical cases to differentiate it from malignancy or infection. First-line treatments are non-steroidal anti-inflammatory drugs (NSAIDs), while bisphosphonates or TNF-α blockers can be used in refractory cases. The disease course is unpredictable, and uncontrolled lesions can complicate with bone fractures and deformations, underlying the importance of long-term follow-up in these patients.
- chronic nonbacterial osteomyelitis (CNO)
- chronic recurrent multifocal osteomyelitis (CRMO)
- chronic nonbacterial osteitis
- SAPHO
- DIRA
- PAPA syndrome
- Majeed syndrome
- monogenic
- auto-inflammatory bone disease
Note: The following contents are extract from your paper. The entry will be online only after author check and submit it.
1. Introduction
2. Incidence and Demographics
3. Clinical Presentation
4. Laboratory Findings
5. Radiological Assessment
6. Bone Biopsy
7. Diagnosis
| Common Differential Diagnosis of CNO/CRMO: |
|---|
Primary malignant bone diseases:
|
References
- Giedion, A.; Holthusen, W.; Masel, L.F.; Vischer, D. Subacute and chronic “symmetrical” osteomyelitis. Ann. Radiol. 1972, 15, 329–342.
- Girschick, H.J.; Raab, P.; Surbaum, S.; Trusen, A.; Kirschner, S.; Schneider, P.; Papadopoulos, T.; Müller-Hermelink, H.K.; Lipsky, P.E. Chronic non-bacterial osteomyelitis in children. Ann. Rheum. Dis. 2005, 64, 279–285.
- Borzutzky, A.; Stern, S.; Reiff, A.; Zurakowski, D.; Steinberg, E.A.; Dedeoglu, F.; Sundel, R.P.; Nelson, K.B.; Bingham, P.; Edwards, E.M.; et al. Pediatric chronic nonbacterial osteomyelitis. Pediatrics 2012, 130, e1190–e1197.
- Gamalero, L.; Belot, A.; Zajc Avramovic, M.; Giani, T.; Filocamo, G.; Guleria, S.; Ferrara, G.; Minoia, F.; Hofer, M.; Larbre, J.-P.; et al. Chronic non-bacterial osteomyelitis: A retrospective international study on clinical manifestations and response to treatment. Clin. Exp. Rheumatol. 2020, 38, 1255.
- Beck, C.; Morbach, H.; Beer, M.; Stenzel, M.; Tappe, D.; Gattenlöhner, S.; Hofmann, U.; Raab, P.; Girschick, H.J. Chronic nonbacterial osteomyelitis in childhood: Prospective follow-up during the first year of anti-inflammatory treatment. Arthritis Res. Ther. 2010, 12, R74.
- Wipff, J.; Costantino, F.; Lemelle, I.; Pajot, C.; Duquesne, A.; Lorrot, M.; Faye, A.; Bader-Meunier, B.; Brochard, K.; Despert, V.; et al. A large national cohort of French patients with chronic recurrent multifocal osteitis. Arthritis Rheumatol. 2014, 67, 1128–1137.
- Bhat, C.S.; Roderick, M.; Sen, E.S.; Finn, A.; Ramanan, A.V. Efficacy of pamidronate in children with chronic non-bacterial osteitis using whole body MRI as a marker of disease activity. Pediatr. Rheumatol. 2019, 17, 1–5.
- Girschick, H.; Finetti, M.; Orlando, F.; Schalm, S.; Insalaco, A.; Ganser, G.; Nielsen, S.; Herlin, T.; Koné-Paut, I.; Martino, S.; et al. The multifaceted presentation of chronic recurrent multifocal osteomyelitis: A series of 486 cases from the Eurofever international registry. Rheumatology 2018, 57, 1203–1211.
- Buch, K.; Thuesen, A.C.B.; Brøns, C.; Schwarz, P. Chronic non-bacterial osteomyelitis: A Review. Calcif. Tissue Int. 2019, 104, 544–553.
- Bhat, C.S.; Anderson, C.; Harbinson, A.; McCann, L.J.; Roderick, M.; Finn, A.; Davidson, J.E.; Ramanan, A.V. Chronic non bacterial osteitis—A multicentre study. Pediatr. Rheumatol. 2018, 16, 74.
- Concha, S.; Hernández-Ojeda, A.; Contreras, O.; Mendez, C.; Talesnik, E.; Borzutzky, A. Chronic nonbacterial osteomyelitis in children: A multicenter case series. Rheumatol. Int. 2019, 40, 115–120.
- Mallya, P.P.; Rao, A.P.; Ranjani, S.; Raghuram, J. Chronic recurrent multifocal osteomyelitis—A case series from India. Indian J. Orthop. 2018, 52, 672–677.
- Zhao, Y.; Wu, E.Y.; Oliver, M.S.; Cooper, A.M.; Basiaga, M.L.; Vora, S.S.; Lee, T.C.; Fox, E.; Amarilyo, G.; Stern, S.M.; et al. Consensus treatment plans for chronic nonbacterial osteomyelitis refractory to nonsteroidal antiinflammatory drugs and/or with active spinal lesions. Arthritis Rheum. 2018, 70, 1228–1237.
- Hofmann, S.R.; Kapplusch, F.; Girschick, H.J.; Morbach, H.; Pablik, J.; Ferguson, P.J.; Hedrich, C.M. Chronic recurrent multifocal osteomyelitis (CRMO): Presentation, pathogenesis, and treatment. Curr. Osteoporos. Rep. 2017, 15, 542–554.
- Jansson, A.F.; Grote, V.; ESPED Study Group. Nonbacterial osteitis in children: Data of a German incidence surveillance study. Acta Paediatr. 2011, 100, 1150–1157.
- Zhao, D.Y.; McCann, L.; Hahn, G.; Hedrich, C.M. Chronic nonbacterial osteomyelitis (CNO) and chronic recurrent multifocal osteomyelitis (CRMO). J. Transl. Autoimmun. 2021, 4, 100095.
- Skrabl-Baumgartner, A.; Singer, P.; Greimel, T.; Gorkiewicz, G.; Hermann, J. Chronic non-bacterial osteomyelitis: A comparative study between children and adults. Pediatr. Rheumatol. 2019, 17, 1–8.
- Watanabe, T.; Ono, H.; Morimoto, Y.; Otsuki, Y.; Shirai, M.; Endoh, A.; Naito, M.; Inoue, Y.; Hongo, T. Skull involvement in a pediatric case of chronic recurrent multifocal osteomyelitis. Nagoya J. Med. Sci. 2015, 77, 493–500.
- Taddio, A.; Ferrara, G.; Insalaco, A.; Pardeo, M.; Gregori, M.; Finetti, M.; Pastore, S.; Tommasini, A.; Ventura, A.; Gattorno, M. Dealing with chronic non-bacterial osteomyelitis: A practical approach. Pediatr. Rheumatol. 2017, 15, 1–8.
- Kostik, M.M.; Kopchak, O.L.; Maletin, A.S.; Mushkin, A.Y. The peculiarities and treatment outcomes of the spinal form of chronic non-bacterial osteomyelitis in children: A retrospective cohort study. Rheumatol. Int. 2019, 40, 97–105.
- Zhao, Y.; Dedeoglu, F.; Ferguson, P.J.; Lapidus, S.K.; Laxer, R.M.; Bradford, M.C.; Li, S.C. Physicians’ perspectives on the diagnosis and treatment of chronic nonbacterial osteomyelitis. Int. J. Rheumatol. 2017, 2017, 1–7.
- Hedrich, C.M.; Hofmann, S.R.; Pablik, J.; Morbach, H.; Girschick, H.J. Autoinflammatory bone disorders with special focus on chronic recurrent multifocal osteomyelitis (CRMO). Pediatr. Rheumatol. 2013, 11, 47.
- Kostik, M.M.; Kopchak, O.L.; Chikova, I.A.; Isupova, E.A.; Mushkin, A.Y. Comparison of different treatment approaches of pediatric chronic non-bacterial osteomyelitis. Rheumatol. Int. 2018, 39, 89–96.
- Dougados, M.; Baeten, D. Spondyloarthritis. Lancet 2011, 377, 2127–2137.
- Kaiser, D.; Bolt, I.; Hofer, M.; Relly, C.; Berthet, G.; Bolz, D.; Saurenmann, T. Chronic nonbacterial osteomyelitis in children: A retrospective multicenter study. Pediatr. Rheumatol. 2015, 13, 25.
- Hofmann, S.R.; Böttger, F.; Range, U.; Lück, C.; Morbach, H.; Girschick, H.J.; Suttorp, M.; Hedrich, C.M. Serum Interleukin-6 and CCL11/Eotaxin may be suitable biomarkers for the diagnosis of chronic nonbacterial osteomyelitis. Front. Pediatr. 2017, 5.
- Kostik, M.M.; Makhova, M.A.; Maletin, A.S.; Magomedova, S.M.; Sorokina, L.S.; Tsukasaki, M.; Okamoto, K.; Takayanagi, H.; Vasiliev, D.S.; Kozlova, D.I.; et al. Cytokine profile in patients with chronic non-bacterial osteomyelitis, juvenile idiopathic arthritis, and insulin-dependent diabetes mellitus. Cytokine 2021, 143, 155521.
- LeClair, N.; Thörmer, G.; Sorge, I.; Ritter, L.; Schuster, V.; Hirsch, F.W. Whole-body diffusion-weighted imaging in CHRONIC recurrent multifocal osteomyelitis in children. PLoS ONE 2016, 11, e0147523.
- Zhao, Y.; Sato, T.S.; Nielsen, S.M.; Beer, M.; Huang, M.; Iyer, R.S.; McGuire, M.; Ngo, A.-V.; Otjen, J.P.; Panwar, J.; et al. Development of a scoring tool for chronic nonbacterial osteomyelitis magnetic resonance imaging and evaluation of its interrater reliability. J. Rheumatol. 2019, 47, 739–747.
- Arnoldi, A.P.; Schlett, C.; Douis, H.; Geyer, L.L.; Voit, A.M.; Bleisteiner, F.; Jansson, A.F.; Weckbach, S. Whole-body MRI in patients with non-bacterial osteitis: Radiological findings and correlation with clinical data. Eur. Radiol. 2016, 27, 2391–2399.
- Zhao, Y.; Chauvin, N.A.; Jaramillo, D.; Burnham, J.M. Aggressive therapy reduces disease activity without skeletal damage progression in chronic nonbacterial osteomyelitis. J. Rheumatol. 2015, 42, 1245–1251.
- Roderick, M.R.; Shah, R.; Rogers, V.; Finn, A.; Ramanan, A.V. Chronic recurrent multifocal osteomyelitis (CRMO)—advancing the diagnosis. Pediatr. Rheumatol. 2016, 14, 1–5.
- Jansson, A.; Renner, E.D.; Ramser, J.; Mayer, A.; Habán, M.; Meindl, A.; Grote, V.; Diebold, J.; Schneider, K.; Belohradsky, B.H. Classification of non-bacterial osteitis: Retrospective study of clinical, immunological and genetic aspects in 89 patients. Rheumatology 2007, 46, 154–160.
