The use of interpreters in medical education as part of the curriculum is scarce, but students have been trained in how to work with interpreters when interviewing patients to fully develop their skills. This eis a ntry discusses aboutarrative review of the relevant literature on the use of interpreters in medical and healthcare education.
1. Introduction
Medical doctors practice medicine in multicultural societies and are expected to exercise cultural competence, such as working with interpreters in order to provide the best quality of care to their patients [1][2][3][4][1,2,3,4]. There are many definitions of cultural competence, although it generally refers to knowledge regarding social and cultural factors that affect health and illness and to actions necessary for the provision of quality and accessible care [1][2][1,2]. The need for cultural competence has been recognized in literature as it may reduce health disparities [2], and doctors can improve their skills and knowledge in this area of practice [5]. Research has shown that cultural competence is associated with increased patient satisfaction and adherence to therapy [1][6][1,6] and has helped physicians enhance their cultural sensitivity [7].
Despite these findings, the integration of cultural competence in medical curricula has been underdeveloped [4][8][4,8]. Alizadeh and Chavan [1] found 18 models of cultural competence, with many training paradigms for medical practitioners revealing a link between cultural competence and enhanced patient satisfaction and adherence to therapy. However, none of these models were specifically tailored for education purposes. [9] also highlighted the importance of cultural issues and the need to integrate cultural competence in medical curricula.
One aspect of cultural competence is to work effectively with people with limited command of the language spoken by health care professionals and to recruit interpreters to assist with this task. However, Himmelstein, Wright, and Wiederman [10][13] explained that there is negligible evidence about medical students working with interpreters within the medical curricula. Third, are undergraduate medical/health care students provided with training on how to use interpreters in health care consultations when they graduate? However, one might say that if students are taught how to use professional interpreters when interviewing patients, they might be able to use the knowledge and skills when they are provided with interpreters at their clinical placements.
Based on a gap identified by Wright and Wiederman [10][13] and on the questions above, the research aim of this study focuses on understanding the extent of interpreter utilization in medical education as part of the curriculum and its effects on educational and health outcomes. To address the research aim, this study has conducted a narrative literature review as presented below.
2. Two Overarching Themes
From the coding of the articles, two overarching themes emerged, largely reflecting the types of articles identified. That is, “use of interpreters during undergraduate medical/health care curricula”, and “developing students’ skills through training in how to use interpreters in health care interviews or consultations”.
2.1. Use of Interpreters during Undergraduate Medical/Health Care Curricula
This section
is fcentrally relevant to the research aim of this study because it focuses on the use of interpreters during undergraduate medical/health care curricula. Interestingly, only five papers discussed the actual use of interpreters in medical or health care education as part of the curriculum
[10][11][12][13][14][13,18,19,20,21]. More specifically, Itaya et al. 2009
[11][18] conducted a survey with students and faculty members to understand how the limited English patients (LEP) were managed in dental education and what was the perceived impact on the quality of education. One hundred and twenty-two (122) students and fifty-six (56) faculty members from five out of six dental schools in California—United States of America (USA)—completed the survey and the results revealed that only ad hoc interpreters were used when dental students interacted with LEP patients at their clinical placements. Further, it revealed that the use of interpreters did not meet the required standards by the U.S. Department of Health and Human Services and the Commission on Dental Accreditation (CODA) and that the lack of professional interpreters in dental schools had a negative impact on the quality of dental education. For example, it increased the length of appointments and decreased the students’ ability to provide high-quality care for these patients (e.g., getting patients to accept treatment plans, gaining compliance with home oral health preventive behaviors, completing treatment plans, etc.).
Another study by Simon et al.
[12][19] with a larger sample of participants exploring what dental schools in the USA did to prepare their students to work effectively with interpreters when interacting with LEP patients during their clinical placements—and therefore improve the care of LEP patients—found the same trends. That is, students from 19 out of the 62 dental schools who completed the survey reported that there was insufficient integration of interpreters in their clinical teaching and poor-quality training for this. To elaborate, only 56.3% of the 325 respondents reported that there was some integration of interpreting services in their education. Additionally, 43.7% said that interpreting services were not used and approximately 30% of the students explained that such lack of services compromised the quality of care provided to LEP patients and the achievement of their dental education outcomes. Only 54% of the respondents agreed that they were well prepared to manage LEP patients after graduation.
In addition to dental schools, a more recent study was conducted using medical schools in the USA
[10][13]. Out of the 147 schools that received a survey link, 38 responded with 29 schools reporting their curriculum addressed the use of interpreters. However, only 10 of these 29 schools had used simulated environments for students’ learning or used didactic teaching sessions. The rest of the schools did not have any relevant curriculum. The majority of the schools (22) offered such training during the first two years of education, while seven schools offered the training later: during years three and four. Eighteen (18) of these schools started training their students how to work with interpreters in the last 10 years. However, this study did not explore whether the medical schools provided trained interpreters or ad hoc interpreters to their students when meeting LEP patients at their clinical placements.
The fourth relevant study by Omoruyi et al.
[13][20] developed and evaluated a curriculum to teach medical students how to use telephone interpreter services during their 8-week outpatient pediatric clinical rotation. This is the only study we found to evaluate medical students’ ability to use interpreter skills in actual patient encounters. The researchers used a case-cohort comparison to investigate “behavioral outcomes of the exposed learners to evaluate if the training had an impact on actual patient encounters.” The results of the study suggested that this type of interventions increased medical students’ perceived self-efficacy in using interpreters in actual patient encounters. More specifically, the students who went through the curriculum were more likely to use effectively the skills below than the students who did not receive the curriculum:
-
The trainee asked the patient one question at a time.
-
The trainee presented information at a pace that was easy to follow for both patient and interpreter—that is, information was given in digestible chunks
-
The trainee addressed the patient as “you” and not as “he” or “she.”
-
The trainee appropriately closed the encounter: at a minimum, asked the patient if he or she had any questions.
The fifth relevant study by Mazori et al.
[14][21] evaluated a program of working with interpreters at a free clinic. Of the 76 medical students, 40 were allocated to the intervention group and 36 were allocated to the control group. The results of the study were very similar to those of Omoruyi et al. (2018) in that when medical students in the intervention group interviewed a LEP patient in their clinical placements (family medicine clerkship), they were able to improve their communication skills such as:
-
Asked patient one question at a time
-
Addressed patient directly
-
Maintained direct eye contact with patient
-
Listened to interpreter without unnecessary interruption
-
Asked interpreter questions about incomplete interpretations
-
Spoke in short, simple sentences with pauses for interpretation
The findings from these five papers show that the use of interpreters in clinical settings in medical education is scarce—or has not yet been documented—and when interpreting services were used, they were underdeveloped in the sense that a few schools used these services or used them on an ad hoc basis. These papers provided some insights into the use of interpreters in medical education in the USA, but we still do not know the extent of the use of interpreters in medical education globally; what patients think about the services; and how students and interpreters feel about it. Although Omoruyi et al.’s
[13][20] and Mazori et al.’s
[14][21] studies discussed the impact of using interpreters on students’ skills, there is no study included in this review which presents information about long-term educational outcomes, student satisfaction, and the impact of interpreting services in medical education on patients and their health outcomes. Such lack of evidence highlights a huge gap in improving medical education in multicultural environments and the need to empirically explore the impact of interpreting services on educational and health outcomes. Finally, we did not find any studies focusing on students’, patients’, interpreters’, or doctors’ perspectives on interpreting services, and on the facilitators and barriers for utilizing interpreters in medical and health care education. However, despite these gaps, students at some schools have been trained in how to work with interpreters, as discussed below.
2.2. Developing Students’ Skills through Training in How to Use Interpreters in Health Care Interviews or Consultations
Fifteen (15) articles were not centrally located in theour research topicaim because they did not discuss the direct use of interpreters in clinical settings as part of the curriculum. However, they indirectly addressed the training of students in using interpreters. That is, these trainings have largely involved interpreters through scenarios or in simulated environments rather than in actual clinical placements or as part of the existing curriculum like the studies discussed in the previous section. Such trainings indirectly relate to theour research topicaim because it is important to know whether they have helped students, thereby informing decisions about the integration of interpreters in medical education.
The findings of these articles indicated that there has been a variety of training paradigms utilized, especially during the pre-clinical years, such as web-based modules
[15][16][17][22,23,24], workshops
[18][25], and evaluation of a longitudinal program
[19][26]. The majority of these paradigms were effective because they helped students develop their skills of using interpreters in their health care interviews/consultations. Specifically, the results demonstrated students had improved their skills in working and collaborating with interpreters
[15][16][17][18][19][20][22,23,24,25,26,27], had improved attitudes
[16][23], were more careful while working with people from other cultures, and appreciated patients’ immigration status
[16][23]. In addition, their self-confidence
[21][22][28,29] and self-efficacy
[23][24][30,31] were enhanced. Students also became more familiar with the relevant procedures used when working with interpreters and LEP patients
[22][29], enhanced their cultural competence skills
[25][26][27][28][32,33,34,35], and managed to match what they practiced with their curriculum
[21][28].
Moreover, Kalet, Gany, and Senter’s
[15][22] and Kalet et al.’s
[16][23] studies indicated that students greatly appreciated the training paradigms they used and expressed a strong interest in learning to collaborate with interpreters. In addition to the use of professional interpreters, two studies focused on the use of medical students as interpreters
[14][27][21,34]. The results revealed that these students improved their skills and enhanced their cultural competency, but were challenged when attempting to separate the two roles in educational settings.
All these findings highlight that various training programs have helped students become more fluent in working with interpreters for the benefit of health care praxis and subsequently for patients. Interestingly, these training programs also suggested that occasionally student skills did not improve and that new paradigms should be explored to further develop the curricula. For instance, Lie, Bereknyei, and Vega’s
[19][26] study found that the skills “ask one question at a time”, “listen without interruption”, and “invited questions” deteriorated over time. The authors postulated several reasons for this. They suggested that relying on ad hoc or temporal training paradigms should be avoided because students’ skills may deteriorate if they do not immerse themselves in life-long reflective development
[13][19][20,26]. In other words, students should engage in repeated utilization of interpreters during their medical studies as part of the curriculum to enhance their fluency. Lie, Bereknyei, and Vega’s study further suggested that without linking this to the formal curriculum, which combined didactic teaching and reflective practices, skills may not be sustainable. Finally, the skill of using interpreters should be taught separately initially for students to master the relevant skills before integrating them with other competencies
[19][26].
3. Framework for Integrating Interpreting Services in Medical Education
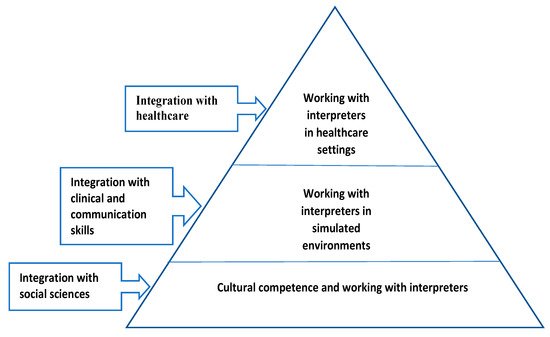
Based on the findings of this study and the identified need to integrate interpreting services in medical education and scientifically explore its impact, we propose a framework for achieving such integration. As per Figure 12, working with interpreters should be under the cultural competence curriculum whereby students acquire knowledge in social and cultural determinants of health and skills in how to work with diverse patients and interpreters. During this stage, training in cultural competence and working with interpreters could be achieved by integration with social sciences and through lectures, interactive cases, and interactive videos. As students move into their medical program and develop their skills, learning how to work with interpreters should be integrated with already-acquired clinical and communication skills. Mastering these skills to work with interpreters could be achieved in simulated environments whereby students learn and practice in small groups utilizing clinical scenarios aided by real simulated patients. Later in their studies, during medical practice or clerkships in hospitals, students could activate the knowledge and skills they gathered from previous years and work effectively with interpreters in health care settings. On this note, this proposed framework suggests that integration of working with interpreters in medical education should be longitudinal and learning should be developed through constructivist and spiral learning approaches.
Figure 12. Longitudinal integration of the use of interpreters in medical education.