As a highly influential physiological factor, pH may be leveraged as a tool to diagnose physiological state. It may be especially suitable for diagnosing and assessing skin structure and wound status. Multiple innovative and elegant smart wound dressings combined with either pH sensors or drug control-released carriers have been extensively studied. Increasing our understanding of the role of pH value in clinically relevant diagnostics should assist clinicians and improve personal health management in the home. In this review, we summarized a number of articles and discussed the role of pH on the skin surface as well as the factors that influence skin pH and pH-relevant skin diseases, but also the relationship of skin pH to the wound healing process, including its influence on the activity of proteases, bacterial enterotoxin, and some antibacterial agents.
1. Introduction
Skin, the major portion of the integumentary system, is the human body’s largest organ. It spans approximately 2 m
2 and is 0.075–0.15 mm thick in the average adult
[1]. It acts as the first line of defense to shield the human body from ultraviolet radiation, infection by pathogens, and chemical irritants
[2]. Furthermore, skin plays a key role in thermoregulation, immunological function, and maintaining body water balance.
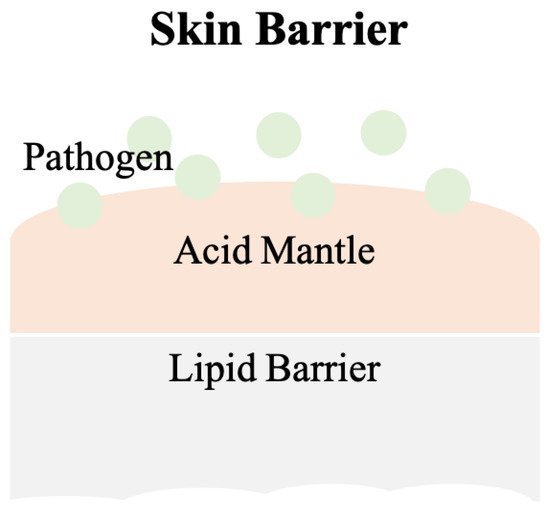
Schade and Marchionini first introduced the term “acid mantle” to describe the slight acidification of the uppermost layer of human skin
[3]. The acid mantle is characterized by a pH value of 4–6, as a result of amino acids, fatty acids, sebum secreted by the sebaceous gland, and lactate excreted from sweat. All of these compounds are acidic and when present together on the human skin, become a barrier that prevents bacterial colonization. Another critical skin barrier is the lipid barrier, the extracellular lipid matrix of the stratum corneum (SC)
[4], which is composed of free fatty acids, cholesterol and ceramides and functions as a hydrophobic barrier for human skin
[5]. A skin barrier schematic is provided in
Figure 1.
Figure 1. The scheme of the skin barrier. Lipid barrier sits atop the acid mantle and displays a pH value of 4–6. Pathogens can be various bacteria. Slight acidic environment is a disadvantage for bacterial colonization.
Most human-pathogen bacteria are inhibited by the acidic milieu on the surface of normal human skin, but this shield is disturbed when skin is wounded. The tissue beneath skin has a physiological pH of 7.4
[6], which raises the overall pH value at the wound site and provides advantages for bacterial colonization. Bacterial contaminants in wounds, e.g.,
Staphylococcus aureus, interfere with the normal wound healing process.
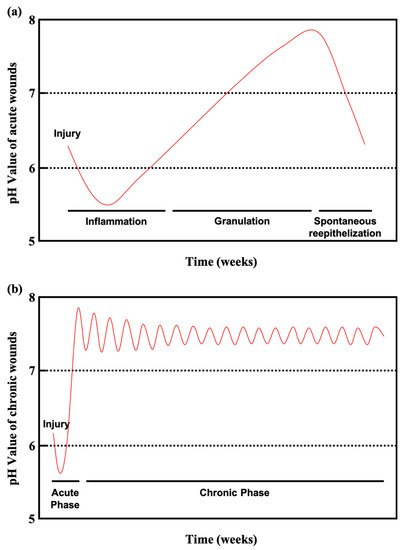
There are four phases in normal wound healing
[7][8][7,8]: hemostasis, inflammation, proliferation, and remodeling. During hemostasis the wound is filled with fibrin and coagulated blood. Clots are formed to stop bleeding and seal the wound site until tissues are repaired. During inflammation, histamine is produced by basophils and mast cells to increase capillary permeability, which allows leukocytes such as neutrophils to migrate to the infected wound site and remove dead cells and pathogens. However, a failure in eliminating pathogens or the remaining high pH environment can be primary reasons for chronic wound development. During proliferation, epithelial cells increase in number, granulation tissue forms, and angiogenesis occurs. Healthy granulation tissues should be pink in color and uneven in texture. The final phase, remodeling, may take years to complete. The wound matrix undergoes degradation by metalloproteinases and new extracellular matrix (ECM) is created during remodeling. Scar tissue can form due to degradation or ECM generation disruption. While the alkaline milieu activates protease, which facilitates the removal of damaged components, excessive amounts of protease eventually destroy newly constructed tissue
[9]. Moreover, alkaline pH values are usually found in chronic wounds, and are associated with an increased risk of bacterial colonization
[10].
pH value is a critical factor in the wound healing process and could offer important physiological condition information regarding skin status and infection. It assists physicians with clinically relevant diagnosis and patient wounds care. It can be used, for instance, to determine whether wounds are infected, becoming chronic, provide monitored, real-time wound status, and ultimately facilitate proper treatment in a more timely manner.
2. Skin
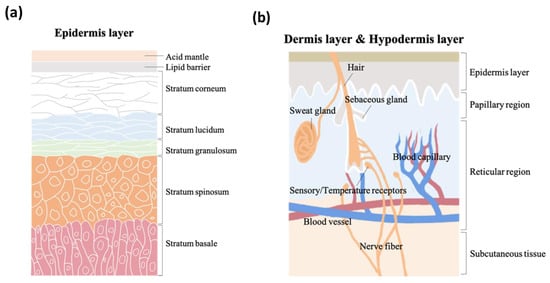
As the vital, first line of defense between the body and the environment, skin is indispensable to human life. Skin structure has been thoroughly described in the literature. It is made up of three major strata, the epidermis, the dermis, and subcutaneous tissue. The epidermis, the outermost layer in skin structure, is approximately 0.05–1 mm thick, provides barrier functions, prevents infection, and regulates transepidermal water loss (TEWL). This layer is constructed of multiple sub-layers; stratum corneum, stratum lucidum, stratum granulosum, stratum spinosum, and stratum basale. The acid mantle and lipid barrier can be found on top of the epidermis, specifically just above the stratum corneum.
Figure 2a is a schematic illustrating the structure of the epidermis. The second of the skin’s major strata, the dermis, can be divided into two layers, the papillary region and the reticular region. The papillary region is the thin and superficial area adjacent to the epidermis. The subsequent layer, the reticular region, is thick and contains arector pili muscles, sebaceous glands, sweat gland ducts, merocrine sweat glands, hair follicles, blood capillaries, sensory receptors, and nerve fibers. The dermis layer is approximately 1–2 mm thick, and comprises collagen, elastic fibers, and extrafibrillar matrix for providing support. The third and deepest of skin’s major three strata, subcutaneous tissue, contains fibroblasts, adipose cells, and macrophages. Subcutaneous tissue is also known as hypodermis and ranges in thickness from 1.65 mm to 18.20 mm depending on gender and skin site
[11][16]. The hypodermis layer is used for fat storage, but it also contains large quantities of loose connective tissue and blood vessels. The structure of the dermis and hypodermis layers are depicted in
Figure 2b.
Figure 2. The schematic structure of (a) epidermis layer, (b) dermis layer, and hypodermis layer.
2.1. pH Values on Skin Surfaces
The skin pH of newborns is weakly alkaline (pH of 7.4) as a result of being encapsulated within the amniotic fluid and the vernix caseosa. Hans, et al., determined and described skin pH characteristics from 209 newborn infants
[12][17]. However, after birth, the weakly alkaline skin becomes acidic in its quest to form the acid mantle
[13][14][18,19] and the functional maturation of stratum corneum is accelerated within 2 to 8 weeks
[15][20]. During this period, infant skin remains highly prone to damage.
During sexual maturation, the pH of skin in the axillary vault climbs from around 5.0 to near 7.0, and then returns to a lower pH during sexual involution
[16][17][21,22]. A. Zlotogorski
[18][23] measured the pH distribution on the surface of the skin (forehead and cheek) of 574 men and women aged 18 to 95, and found that those over the age of 80 had higher skin surface pH values compared to the other groups, which displayed skin surface pH values between 4.0 and 5.5 on the forehead and between 4.2 and 5.9 on the cheek. There was no significant pH difference based on gender. Irvin H. Blank
[19][24] obtained skin surface pH values (forearm, antecubital, elbow, upper arm, forehead, and back of neck) from 100 males and 100 females aged 19–27 and found pH values varying from 4.0 to 7.0, with the most frequent readings being between 4.2 and 5.6, and evidence suggesting that females have a slightly higher skin pH (0.5 higher) than males. C. Ehlers and coworkers
[20][25] found that there was a statistically significant difference in skin pH (arm) between men and woman. Notably, measurements could not be conducted close to the wrist because most people wash their hands several times each day, and soaps can make the skin more alkaline. Another study conducted by S. Luebberding and coworkers
[21][26] followed strict criteria and found pH differences between males and females in TEWL, SC hydration, sebum content, and at the skin surface (forehead, forearm, hand and cheek).
Table 1 (adapted from
[21][26]) displays gender-related data showing that the pH values from five skin sites and across all age groups were higher in females compared to males. This data also shows that the mean evaporimetry and corneometry values were higher for the females of this group, while the mean sebumetry values were higher for the males.
Table 1. Mean values (MV ± SD) arranged by age groups and localization (adapted from [21]).
| |
AG I |
AG II |
AG III |
AG IV |
AG V |
Mean |
| |
♀ |
♂ |
♀ |
♂ |
♀ |
♂ |
♀ |
♂ |
♀ |
♂ |
♀ |
♂ |
| F |
5.01 ± 0.42 |
4.31 ± 0.28 |
4.98 ± 0.50 |
4.47 ± 0.33 |
4.92 ± 0.40 |
4.50 ± 0.36 |
5.10 ± 0.49 |
4.56 ± 0.30 |
4.67 ± 0.32 |
4.57 ± 0.35 |
4.94 ± 0.45 |
4.48 ± 0.33 |
| C |
5.33 ± 0.32 |
4.66 ± 0.38 |
5.27 ± 0.44 |
4.77 ± 0.33 |
5.19 ± 0.29 |
4.74 ± 0.36 |
5.35 ± 0.46 |
4.82 ± 0.27 |
5.21 ± 0.41 |
4.93 ± 0.32 |
5.27 ± 0.39 |
4.78 ± 0.34 |
| N |
5.09 ± 0.32 |
4.62 ± 0.37 |
5.09 ± 0.36 |
4.72 ± 0.36 |
5.08 ± 0.34 |
4.63 ± 0.34 |
5.37 ± 0.49 |
4.76 ± 0.28 |
5.05 ± 0.41 |
4.73 ± 0.29 |
5.13 ± 0.40 |
4.69 ± 0.33 |
| A |
5.12 ± 0.31 |
4.49 ± 0.42 |
5.22 ± 0.40 |
4.50 ± 0.36 |
5.17 ± 0.38 |
4.53 ± 0.30 |
5.44 ± 0.45 |
4.62 ± 0.37 |
5.12 ± 0.43 |
4.58 ± 0.37 |
5.21 ± 0.41 |
4.54 ± 0.36 |
| H |
5.10 ± 0.37 |
4.33 ± 0.36 |
5.19 ± 0.40 |
4.41 ± 0.32 |
5.03 ± 0.35 |
4.38 ± 0.31 |
5.25 ± 0.38 |
4.55 ± 0.42 |
4.88 ± 0.41 |
4.46 ± 0.40 |
5.09 ± 0.40 |
4.42 ± 0.37 |
| |
Female (Age ± SD) |
Male (Age ± SD) |
| AG I |
24.73 ± 2.59 |
25.70 ± 2.48 |
| AG II |
33.30 ± 2.92 |
33.23 ± 2.90 |
| AG III |
43.63 ± 2.81 |
44.23 ± 3.09 |
| AG IV |
55.17 ± 2.84 |
54.20 ± 3.13 |
| AG V |
66.57 ± 4.31 |
66.63 ± 2.61 |