Gastric cancer is the fifth most common cancer worldwide, and it is responsible for 7.7% of all cancer deaths. Despite advances in the field of oncology, where radiotherapy, neo and adjuvant chemotherapy may improve the outcome, the only treatment with curative intent is represented by surgery as part of a multimodal therapy. Two concepts may be adopted in appropriate cases, neoadjuvant treatment before gastrectomy (G) or primary surgical resection followed by chemotherapy.
- gastric cancer
- surgery
- lymphadenectomy
- survival
1. Introduction
Gastric cancer is the fifth most common cancer worldwide, and it is responsible for 7.7% of all cancer deaths. Although surgical treatment for gastric cancer has been considerably improved during recent decades, the mortality rate from gastric cancer is still high [1]. Statistical data show that the 5-year survival rate for patients treated with curative intent (gastric resection and lymphadenectomy) is 70% for stage I resected gastric cancer and less than 30% for stage IIB disease and beyond [2].
Genetic alterations responsible for the development and progression of gastric cancer such as cell adhesion, signal transduction, DNA methylation, and glycosylation changes may lead to early detection of gastric cancers using these biomarkers [6].
For patients with hereditary diffuse gastric cancer (HDGC), who carry a lifetime gastric cancer risk of approximately 70% in men and 56% in women, a prophylactic total gastrectomy at the age of 20 years is the procedure of choice [7]. Recently, there have been numerous sources of evidence establishing the importance of combining systemic chemotherapy with surgery in advanced gastric cancer. Given the latest results, there has been a shift in the paradigm of gastric cancer treatment with the increasing use of preoperative and postoperative chemotherapy [8].
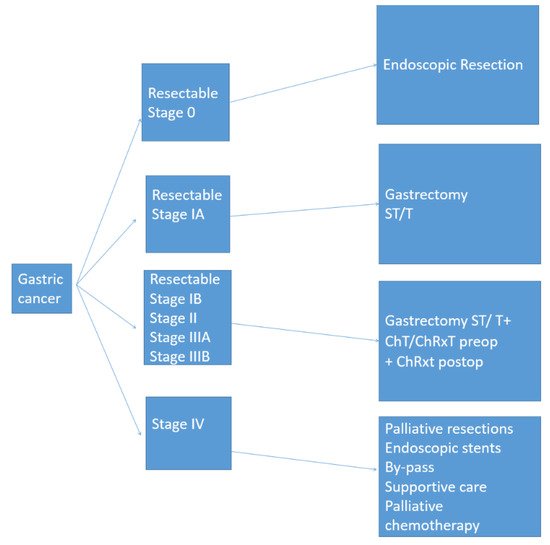
Unfortunately, malignant tumors of the stomach are often diagnosed in locally advanced or metastatic stages when the median overall survival remains poor [9]. Important surgical aspects such as optimum resection margins, surgical technique, number of harvested lymph nodes are important factors for patient outcomes. The standardization of surgical treatment of gastric cancer in accordance with the patient’s profile is of decisive importance for a better outcome (Figure 1). This review aims to summarize the current standards in the surgical treatment of gastric cancer.
2. Results and Discussion
The extent of surgical resection required to achieve surgical margins free of malignant cells, R0, depends on the size, location, and histological type of the tumor. The optimal length for the proximal margin is often suggested to be at least 3 to 5 cm depending on the tumor histology [11]. However, recent studies suggest that resection margins of 1 cm may be comparable in terms of survival and oncological outcome [12].
Since the standard approach for gastric cancer with any localization is total gastrectomy (TG), several studies have shown that the outcomes of patients with proximal tumors who underwent TG or proximal gastrectomy (PG) were similar in terms of the overall survival interval and disease-free interval [13]. Some authors suggest that distal gastrectomy can be safely performed for patients with distal lesions and TG/PG may be performed for proximal lesions [14]. [15], and the researchers showed that patients with proximal tumors who underwent PG resection had similar overall survival and disease-free intervals compared with patients who underwent TG resection. Several trials [17,18,19,20,21] addressed the issues of postoperative mortality, morbidity, and long-term outcome of TG versus subtotal gastrectomy (SG) for distal tumors.
The controversy continues in tumors of the cardia when radical resection requires supradiaphragmatic anastomosis [23]. There are three therapeutic options in such cases: some surgeons prefer PG, whereas others adopt either TG or esophagectomy with proximal cervical anastomosis as the ideal therapeutic option. The actual recommendations are to avoid the transabdominal approach only for the extent of esophageal resection in tumors involving the distal esophagus and cardia. Recent reports have indicated that, if R0 can be safely achieved, pylorus-preserving resection for gastric cancer should be considered because no difference in survival was reported compared with more extensive procedures [27,28].
The technique of anastomosis that began in 1881, when Theodor Billroth performed the first gastrectomy, has been extensively explored in numerous studies since then [29]. Although Billroth I was the method of choice for a long time, it is currently accepted that the bile reflux gastritis is best minimized by Roux-en-Y reconstruction [30]. However, until the 21st century, the general preference for TG was to use jejunum loop reconstruction; during the last two decades, Roux-en-Y reconstruction became the standard procedure worldwide [31]. The Roux-en-Y reconstruction following TG is also a preferred method of reconstruction after pancreatic and biliary resections and liver and pancreatic cysts, as well as in bariatric surgery [32].
The reconstruction using jejunal pouches has historical value, but such pouches are no longer employed because they show limited benefit. Small-bowel interposition was preferred in the past by some surgeons; today, it has less acceptance and is rarely used [33].
Extended resection (D2 resection with splenectomy and distal pancreatectomy) for advanced gastric cancer, initially performed by Japanese surgeons, has been a subject of debate for decades [34]. Although early reports showed improved survival [35], large prospective randomized control trials failed to report a real survival benefit. In patients with splenectomy and distal pancreatectomy, higher morbidity, higher mortality, and longer hospital stays were observed [36]. Importantly, in multivariate analysis, PS and S alone were found to not be independent factors for survival, strongly suggesting that PS increases morbidity rates without improving survival.
A series of 353 patients who underwent extended resection of the adjacent organs (removal of transverse colon in 45%, pancreas and spleen in 42.5%, left hepatic lobe in 28.5%, and head of the pancreas in 10.5%) was published by Shchepotin et al. TG was performed in 32.9% of patients and SG in 67.1%. The lymphadenectomy was standardly performed in all patients (lymph nodes around stomach, celiac axis, hepatic artery, and proximal splenic artery). The presented data displayed a 5-year survival rate of 25% (37% for N− and 15% for N+).
Data arising from two prospective randomized control trials that do not favor gastrectomy with additional organ resection have been published [39,40]. [41] reported the results of extended gastrectomy on 996 patients randomized to a D1 or D2 lymph node dissection. A significant increase in postoperative complications, reoperation rates, and hospital stays was seen in patients requiring a D2 lymphadenectomy [42]. We can conclude that extended resection (where R0 is feasible) of the adjacent organs can be performed by highly experienced surgeons in patients with T4 tumors.
The extent of lymphadenectomy performed along with gastrectomy has been a debated subject for decades [45,46,47,48]. The concept was first described by the Japanese Research Society for Gastric Cancer (JRSGC) in 1973 [49]. Comparisons between limited D1 (perigastric lymph nodes), extended D2 (perigastric and celiac axis lymph node stations), and D3 (perigastric, celiac axis, and para-aortic lymph node stations) lymphadenectomies have been analyzed for decades in prospective randomized trials.
Some authors suggest that the oncological benefit of extended nodal resection does not overcome the drawbacks of postoperative morbidity and mortality. Most Western surgeons consider that extended nodal dissection has no benefit for overall survival and malignant lymph nodes are prognostic indicators rather than factors of survival. Other surgeons (e.g., Japanese surgeons) think that the optimal therapy associated with better loco-regional control is radical gastrectomy with extensive lymphadenectomy [50]. These facts have also been confirmed by several experienced surgeons who performed complete D2 lymphadenectomy and showed that complications are no higher for D2 in surgeries performed by experienced surgeons; however, the 5-year survival rate because of prevention of loco-regional recurrences is significantly higher in those patients [51].
The researchers randomized D1 and D2 dissection into two groups (711 patients in total). The D1 lymphadenectomy addressed perigastric lymph nodes only, and extended D2 lymphadenectomy incorporated additional clearance of celiac axis lymph nodes. Importantly, no difference in 5-year survival between the two groups (34% in D1 vs. 33% in D2) was observed. The unanimous conclusion following this trial was that routinely performed D2 lymphadenectomy in gastric cancer patients has no benefits for long-term survival.
The same Dutch Gastric Cancer Trial (DGCT) group recently reported data from a 15-year follow up after the above randomized nationwide Dutch D1/D2 trial and showed that disease-specific survival was significantly higher in patients receiving D2 versus D1 lymphadenectomy, but there was no improvement in overall survival [53].
In one group, 200 patients underwent D1 dissection (lymphadenectomy within 3.0 cm of the tumor survival); in the other group, the remaining 200 patients had D2 dissection (lymphadenectomy of the omental bursa, hepatoduodenal nodes, and retroduodenal nodes for distal cancers and the splenic artery/splenic pedicle nodes for proximal cancers). In this trial, the postoperative morbidity and mortality were significantly higher in the D2 group (D2 vs. D1: 46% vs. 28%,p< 0.001; 13% vs. 6.5%;p= 0.04) The obtained results were comparable in terms of 5-year survival rates (35% for D1 resection and 33% for D2), gastric cancer-specific survival (hazard ratio (HR) = 1.05, 95% confidence interval (CI): 0.79–1.39), and recurrence-free survival (HR = 1.03, 95% CI: 0.82–1.29). Based on the findings of the trial, the authors suggested that classical Japanese D2 resection offered no survival advantage over D1 resection.
Following the criticism of the Dutch trial because of the high complication rate, an Italian phase II study [55] was proposed to clarify the importance of D2 dissection. To avoid potential bias, only surgeons with extensive experience in gastric cancer surgery were allowed to participate. In 191 patients with D2 lymphadenectomy (with spleen preservation), the authors showed almost similar morbidity rates following D1 and D2 lymph node dissection (12.0% vs. 17.9%,p= 0.178); there were also comparable results in terms of the 30-day postoperative mortality rates (D1 vs. D2: 3.0% vs. 2.2%,p= 0.72).
To assess the importance of an extended D2 (para-aortic lymph nodes) resection following gastric resection for cancer, a randomized trial was conducted by East Asia Surgical Oncology [56], in which 269 patients were divided into two groups. There were 135 patients in the D2 resection group and 134 in the D2+ para-aortic lymphadenectomy group. The authors reported comparable 5-year survival intervals between the two groups (52.6% for D2 vs. 55.0% for D2 The presented data failed to impose prophylactic para-aortic lymphadenectomy as a standard technique in gastric cancer treatment.
A significantly better disease-specific survival was observed in D2 compared with D1 lymphadenectomy in a Cochrane systematic review Data analysis from the Surveillance, Epidemiology, and End-Results (SEER) database has shown that survival benefits occurred in patients with gastric resections who had >15 lymph nodes excised during gastrectomy [59]. Although D2 lymphadenectomy is not mandatory for gastric cancer treatment, it is strongly recommended. The current The National Comprehensive Cancer Network NCCN guidelines sustain that lymphadenectomy should remove at least 15 nodes to optimize oncologic outcomes in gastric cancer [60].
Anastomotic leakage, pancreatic leakage, and higher reoperation rates were associated with D2 dissection in the MRC [55] and Dutch trials [41], mainly because of inadequate surgical training in splenectomy and pancreatectomy rather than D2 itself. An Italian trial showed for the first time that D2 dissection without splenectomy and distal pancreatectomy has the same mortality and morbidity as the same surgery does for D1 dissection [61]. Routinely performed splenectomy or distal pancreatectomy may be considered efficient only when the primary tumor or metastatic lymph nodes directly invade the pancreas and spleen [62].
Recent studies have shown that the incidence of positive margins following extended resection for advanced gastric cancer is around 24% [63]. This rate includes reports from pathology examinations (R1) and macroscopic validation of malignant tissue on resection margins (R2) [64].
A retrospective study was conducted by Cho et al. [65] over a 15-year period. Of the 2740 patients included, 49 (1.8%) had positive margins (29 proximal and 20 distal), and multivariate analysis identified extragastric extension and total gastrectomy as independent risk factors for positive resection margins (p= 0.015 andp= 0.014, respectively). Long-term survival was also significantly lower in patients with positive margins than in those with negative margins (p= 0.0028 andp= 0.025, respectively).
Multiple prospective randomized trials regarding the influence of the R1 margin on gastric cancer survival have been conducted in Asian and Western populations, but the results have been controversial [66,67,68]. Several authors found that positive margins are an independent risk factor for survival following gastric resection for cancer [69]. A multivariate regression analysis performed by Bickenbach [70] showed that R1 margins were associated with poor survival, but this association was only observed in patients with fewer than three positive lymph nodes or T1–2 disease. [69] obtained controversial results via a systematic review, but they agreed that re-resection should be performed to eliminate the R1 margin whenever feasible [71].
It has been stated in previous studies that high-volume departments are significantly associated with better survival, lower mortality and morbidity, and lower reoperation rates following resection for gastric cancer [72,73,74,75]. An intergroup trial [76] that assessed the implementation of D2 lymphadenectomy in US hospitals showed that in 556 patients with adjuvant chemoradiotherapy and gastric resection, 54% had incomplete lymphadenectomy (less than D1), 37% had D1, and only 9% had D2. The underlying factor was the surgeon’s experience. It has been proven using computer-based models that poor dissections of lymph nodes because of inadequate surgical techniques lead to poor survival in these patients [79,80].
An extensive meta-analysis analyzed 28 papers describing the relationship between hospital volume and surgeons’ experience; the 5-year survival showed that high-volume hospitals have fewer complications and better outcomes following gastric resection for cancer [81]. The number of procedures (gastric resection with D2) and the surgeons’ level of training and supraspecialization are key factors related to low postoperative complications, low gastrectomy-related mortality, and better five-year survival.
Studies suggest that procedure-related mortality is significantly higher in US hospitals, ranging from 5% to 13% [82]. Large statistical data examining more than 600 hospitals in the US over a 5-year period showed that the average perioperative mortality rate was 7.2%. Therefore, based on the above results and from our personal experience, we state that D2 lymphadenectomy and gastric surgery for cancer should be performed in tertiary surgical centers where surgeons are routinely performing this type of operation and have very low operative morbidity and mortality rates.
Laparoscopic resection of gastric cancer is routinely performed worldwide [83] and has become a popular approach for treating gastric cancer in Asian countries (representing 25% of all gastric resections for cancer in Japan and South Korea) [84,85]. The surgical techniques and postoperative outcome have been well established in two prospective trials (KLASS 01 and JCOG 0703) for early gastric cancer [86,87].
A Japanese study (LOC-1) included 3630 patients with early gastric cancer treated with laparoscopic gastrectomy (LG) or open gastrectomy (OG) between 2006 and 2012. [88]. There was no significant difference in the 5-year overall survival (97.1% for LG vs. 96.3% for OG) or local recurrence rate (2.3% vs. 2.4%).
In 2006–2010, a trial developed in South Korea (KLASS-1), which involved 1400 patients with invasive distal gastric cancer limited to the submucosa, analyzed the feasibility of laparoscopic distal gastrectomy [88]. The LG group had a lower morbidity rate (13% vs. 20%) and lower wound infections (3.6% vs. 7%) compared with the OG group. Major intra-abdominal complications and perioperative mortality rates were similar between the two groups. The overall 5-year survival rate was comparable between the two groups (LG: 94.2%; OG: 93.3%), as were the cancer-specific survival rates
LG is a complicated procedure that requires training and experience [90,91]; it also necessitates support from the staff and hospital. The technical pitfalls make LG controversial for the resection of locally advanced tumors, mainly because of concerns regarding the R0 acquisition and adequate D2 dissection [92]. However, patients with LGs report a better quality of life in the early postoperative period. Ultimately, patients with invasive gastric cancer that invades no more deeply than the submucosa, regardless of lymph node metastasis (T1, any N, M0), and who are free of significant cardiopulmonary diseases, obesity, and previous upper abdominal surgery, are most suitable for LG.
3. Conclusions
The standardization of surgical resection in accordance with tumor stage is of decisive importance for a better outcome. As gastrectomy and adequate lymph node resection may be challenging, the treatment must be provided by a multidisciplinary team in a high-volume center. If R0 is technically feasible, distal gastrectomy can be safely performed for patients with distal lesions while TG/PG may be performed for proximal lesions. As surgical centers with higher volume have very low operative morbidity and mortality rates, patients proposed for D2 lymphadenectomy and gastric resection for cancer should be referred to these hospitals.
