Eosinophilic pneumonia (EP), including acute EP and chronic EP, is characterized by the massive pulmonary infiltration of eosinophils into the lung. However, the mechanisms underlying the selective accumulation of eosinophils in EP have not yet been fully elucidated. We reported that bronchoalveolar lavage fluid (BALF) from EP patients induced the transmigration of eosinophils across endothelial cells in vitro. The concentrations of eotaxin-2 (CCL24) and monocyte chemotactic protein (MCP)-4 (CCL13), which are CC chemokine receptor (CCR) 3 ligands, were elevated in the BALF of EP patients, and anti-CCR3 monoclonal antibody inhibited the eosinophil transmigration induced by the BALF of EP patients. The concentration of macrophage inflammatory protein 1β (CCL4), a CCR5 ligand that induces eosinophil migration, was increased in the BALF of EP patients. Furthermore, the concentration of interleukin (IL) 5 was increased in the BALF of EP patients, and it has been reported that anti-IL-5 antibody treatment resulted in remission and the reduction of glucocorticoid use in some cases of chronic EP. The concentrations of lipid mediators, such as leukotriene (LT) B4, damage-associated molecular pattern molecules (DAMPs), such as uric acid, or extracellular matrix proteins, such as periostin, were also increased in the BALF of EP patients. These findings suggest that chemokines, such as CCR3/CCR5 ligands, cytokines, such as IL-5, lipid mediators, such as LTB4, DAMPs, and extracellular matrix proteins may play roles in the accumulation or activation of eosinophils in EP.
- chemokines
- cytokines
- eosinophilic pneumonia
- eosinophils
- pneumonia
1. Classification
Eosinophilic pneumonia is divided into different categories depending upon whether its cause can be determined or not. Known causes include certain medications or environmental triggers, parasitic infections, and cancer. Eosinophilic pneumonia can also occur when the immune system attacks the lungs, a disease called eosinophilic granulomatosis with polyangiitis. When a cause cannot be found, the eosinophilic pneumonia is termed "idiopathic". Idiopathic eosinophilic pneumonia can also be divided into acute and chronic forms, depending on the symptoms a person is experiencing.[1]
2. Signs and Symptoms
Most types of eosinophilic pneumonia have similar signs and symptoms. Prominent and nearly universal signs and symptoms include cough, fever, difficulty breathing, and night sweats. Acute eosinophilic pneumonia typically follows a rapid course. Fever and cough may develop only one or two weeks before breathing difficulties progress to the point of respiratory failure requiring mechanical ventilation. Chronic eosinophilic pneumonia usually follows a slower course. Symptoms accumulate over several months and include fever, cough, difficulty breathing, wheezing, and weight loss. Individuals with chronic eosinophilic pneumonia are often misdiagnosed with asthma before the correct diagnosis is made. Eosinophilic pneumonia due to medications or environmental exposures is similar and occurs after an exposure to a known offending agent. Eosinophilic pneumonia due to parasitic infections has a similar prodrome in addition to a host of different symptoms related to the variety of underlying parasites. Eosinophilic pneumonia in the setting of cancer often develops in the context of a known diagnosis of lung cancer, cervical cancer, or other certain types of cancer.
3. Pathophysiology
Eosinophilic pneumonia can develop in several different ways depending on the underlying cause of the disease. Eosinophils play a central role in defending the body against infection by parasites. Many diseases, such as asthma and eczema, are caused when eosinophils overreact to environmental triggers and release an excess of chemicals, e.g., cytokines and histamine. The common characteristic among different causes of eosinophilic pneumonia is eosinophil overreaction or dysfunction in the lungs.
Medications and environmental exposures
Medications, substance abuse, and environmental exposures may all trigger eosinophil dysfunction. Medications such as nonsteroidal anti-inflammatory drugs (e.g., ibuprofen), nitrofurantoin, phenytoin, L-tryptophan, daptomycin[2] and ampicillin, and drugs of abuse such as inhaled heroin and cocaine may trigger an allergic response which results in eosinophilic pneumonia. Chemicals such as sulfites, aluminum silicate, and cigarette smoke can cause eosinophilic pneumonia when inhaled. A New York City firefighter developed eosinophilic pneumonia after inhalation of dust from the World Trade Center on September 11, 2001.[3]
Parasitic infections
Parasites cause eosinophilic pneumonia in three different ways. Parasites can either invade the lungs, live in the lungs as part of their life cycle, or be spread to the lungs by the bloodstream. Eosinophils then migrate to the lungs in order to fight the parasites, and cause eosinophilic pneumonia when they release their contents. Important parasites that invade the lungs include Paragonimus lung flukes and the tapeworms Echinococcus and Taenia solium. Important parasites which inhabit the lungs as part of their normal life cycle include the worms (helminths) Ascaris lumbricoides, Strongyloides stercoralis and the hookworms Ancylostoma duodenale and Necator americanus. When eosinophilic pneumonia is caused by helminths, it is often called "Löffler's syndrome". The final group of parasites cause eosinophilic pneumonia when their eggs are carried into the lungs by the bloodstream. This can include Trichinella spiralis, Strongyloides stercoralis, Ascaris lumbricoides, the hookworms, and the schistosomes.[4]
Acute and Chronic Eosinophilic Pneumonia
The causes for both acute and chronic eosinophilic pneumonia are unknown as of 2005. There is some suspicion that at least the acute form is the result of the body's response to some unidentified environmental agent.
4. Diagnosis
Eosinophilic pneumonia is diagnosed in one of three circumstances: when a complete blood count reveals increased eosinophils and a chest X-ray or computed tomography identifies abnormalities in the lungs, when a biopsy identifies increased eosinophils in lung tissue, or when increased eosinophils are found in fluid obtained by a bronchoscopy (bronchoalveolar lavage fluid). Association with medication or cancer is usually apparent after review of a person's medical history. Specific parasitic infections are diagnosed after examining a person's exposure to common parasites and performing laboratory tests to look for likely causes. If no underlying cause is found, a diagnosis of acute or chronic eosinophilic pneumonia is made based upon the following criteria. Acute eosinophilic pneumonia is most likely with respiratory failure after an acute febrile illness of usually less than one week, changes in multiple areas and fluid in the area surrounding the lungs on a chest X-ray, and eosinophils comprising more than 25% of white blood cells in fluid obtained by bronchoalveolar lavage. Other typical laboratory abnormalities include an elevated white blood cell count, erythrocyte sedimentation rate, and immunoglobulin G level. Pulmonary function testing usually reveals a restrictive process with reduced diffusion capacity for carbon monoxide. Chronic eosinophilic pneumonia is most likely when the symptoms have been present for more than a month. Laboratory tests typical of chronic eosinophilic pneumonia include increased levels of eosinophils in the blood, a high erythrocyte sedimentation rate, iron deficiency anemia, and increased platelets. A chest X-ray can show abnormalities anywhere, but the most specific finding is increased shadow in the periphery of the lungs, away from the heart.
Differential diagnosis
This includes:
- Asthma
- Environmental allergic reaction
- Granulomatosis with polyangiitis
- Allergic bronchopulmonary aspergillosis
- Churg–Strauss syndrome
- Loeffler's syndrome
- Acute eosinophilic pneumonia
- Chronic eosinophilic pneumonia (Carrington's disease)
- Polyarteritis nodosa
- Parasitic infections
- Tropical pulmonary eosinophilia
- Tuberculosis
- Fungal infection
- Sarcoidosis
- Drug reaction with eosinophilia and systemic symptoms
- Mastocytosis
- Lymphoproliferative hypereosinophilic syndrome
- Myeloproliferative hypereosinophilic syndrome
5. Treatment
When eosinophilic pneumonia is related to an illness such as cancer or parasitic infection, treatment of the underlying cause is effective in resolving the lung disease. When due to acute or chronic eosinophilic pneumonia, however, treatment with corticosteroids results in a rapid, dramatic resolution of symptoms over the course of one or two days. Either intravenous methylprednisolone or oral prednisone are most commonly used. In acute eosinophilic pneumonia, treatment is usually continued for a month after symptoms disappear and the X-ray returns to normal (usually four weeks total). In chronic eosinophilic pneumonia, treatment is usually continued for three months after symptoms disappear and the X-ray returns to normal (usually four months total). Inhaled steroids such as fluticasone have been used effectively when discontinuation of oral prednisone has resulted in relapse.[5] Because eosinophilic pneumonia affects the lungs, individuals develop difficulty breathing. If enough of the lungs are involved, it may not be possible for a person to breathe without support. Non-invasive machines such as a bilevel positive airway pressure machine may be used. Otherwise, placement of a breathing tube into the mouth may be necessary and a ventilator may be used to help the person breathe.
6. Prognosis
Eosinophilic pneumonia due to cancer or parasitic infection carries a prognosis related to the underlying illness. Acute and chronic eosinophilic pneumonia, however, have very little associated mortality as long as intensive care is available and treatment with corticosteroids is given. Chronic eosinophilic pneumonia often relapses when prednisone is stopped; therefore, some people require lifelong therapy. Long-term use of prednisone has many side effects, including increased infections, osteoporosis, stomach ulcers, Cushing's syndrome, and changes in appearance.[6]
7. Epidemiology
Eosinophilic pneumonia is a rare disease. Parasitic causes are most common in geographic areas where each parasite is endemic. Acute eosinophilic pneumonia can occur at any age, even in previously healthy children, though most patients are between 20 and 40 years of age. Men are affected approximately twice as frequently as women. Acute eosinophilic pneumonia has been associated with smoking. Chronic eosinophilic pneumonia occurs more frequently in women than men and does not appear to be related to smoking. An association with radiation for breast cancer has been described.[7]
History
Chronic eosinophilic pneumonia was first described by Carrington[8] in 1969, and it is also known as Carrington syndrome. Prior to that, eosinophilic pneumonia was a well-described pathologic entity usually associated with medication or parasite exposures. Acute eosinophilic pneumonia was first described in 1989.[9][10]
1. Introduction
2. Mechanisms for the Development of Eosinophilic Airway Inflammation
Eosinophils accumulate at sites of allergic inflammation and play important roles in the pathogenesis of diseases, including EP, through the release of a variety of mediators, including specific granule proteins, such as major basic protein, cysteinyl leukotrienes (cysLTs), radical oxygen species, and cytokines [5]. Among them, IL-5 is a well-recognized cytokine associated with eosinophilic inflammation. The in vitro effects of IL-5 on eosinophils include the priming of the eosinophils and the enhancement of their survival [6]. Recently, the roles of IL-5 in the pathogenesis of eosinophilic diseases, such as eosinophil-dominant severe asthma and EGPA, have been established. In severe asthmatics with persistent blood or sputum eosinophilia, anti-IL-5 monoclonal antibody (mAb) treatment reduced both the blood eosinophil count and acute exacerbations [7][8][9]. In EGPA, anti-IL-5 mAb treatment resulted in a higher proportion of remission, thus allowing for the reduced use of glucocorticoid [10]. The concentration of IL-5 is increased in the BALF of EP patients, as described above. In this context, several case reports have suggested a positive effect for mepolizumab (anti-IL-5 mAb) on remission and the reduction of glucocorticoid use in CEP [11][12]. Eosinophils must adhere to and migrate across vascular endothelial cells to accumulate in airways [13][14]. These processes are mainly regulated by cytokines, especially IL-4/IL-13, or chemokines from a variety of cells, such as T helper (Th) 2 cells or group 2 innate lymphoid cells. The interaction between eosinophils and endothelial cells via the α4 integrins/vascular cell adhesion molecule (VCAM)-1 pathway is an important step for selective eosinophil recruitment [13][14]. IL-4 and IL-13 induce VCAM-1 expression on endothelial cells, and blood eosinophils spontaneously adhere to VCAM-1 [15][16]. This interaction between eosinophils and VCAM-1 induces superoxide anion (O2−) generation and the degranulation of eosinophils, and can be considered the initial step of eosinophil activation [13][14][15][16][17]. Eosinophil chemoattractants can induce the effective migration of eosinophils after adhesive interaction with endothelial adhesion molecules, such as VCAM-1 [13][14]. CC chemokines, especially CC chemokine receptor (CCR) 3 ligands, such as those regulated upon activation, normal T-expressed and secreted (RANTES; CCL5), eotaxin (CCL11), eotaxin-2 (CCL24), monocyte chemotactic protein (MCP)-3 (CCL7), and MCP-4 (CCL13), all effectively induce eosinophil transmigration across endothelial cells that express VCAM-1 [18]. Several studies have confirmed that CCR3 ligands are upregulated in the airways of bronchial asthma or EP patients [19][20][21][22]. Furthermore, the role of CCR5 and its ligands in the development of eosinophilic inflammation has been reported [23]. The concentration of macrophage inflammatory protein (MIP) 1β (CCL4), a CCR5 ligand, is increased in the BALF of EP patients [23]. Eosinophils can be activated and degranulated by cytokine/eosinophil growth factors, especially IL-5, IL-3, or granulocyte-macrophage colony-stimulating factor (GM-CSF), after migration across endothelial cells [6][13][14]. The important role of IL-5 in the development of eosinophilic inflammation has been established, as described above. GM-CSF also plays roles in eosinophil activation. For example, GM-CSF induces eosinophil O2− generation and degranulation in the presence of VCAM-1 or intercellular cell adhesion molecule 1 in vitro [16]. Furthermore, the airway eosinophils obtained after segmental allergen challenge in allergic subjects can be activated by GM-CSF, but not by IL-5, mainly because IL-5 receptor (R) α is downregulated [24][25]. Moreover, lipid mediators, such as leukotriene (LT) B4, cysLTs, and platelet-activating factor, may contribute to the accumulation of tissue eosinophils in the airways. As for cysLTs, LTE4 inhalation increases the accumulation of eosinophils [13][14]. LTD4 enhances the expression of β2 integrins on human eosinophils in vitro, and thus augments eosinophil adhesion [26]. Moreover, LTD4 directly induces transendothelial migration, respiratory burst, and degranulation, mainly via the cysLT1 receptor and β2 integrin [27]. These findings suggest that, in addition to the type 2 network, lipid mediators, including cysLTs, can induce eosinophilic infiltration and activation in the airways.3. Role of CCR3 Ligands or CCR5 Ligands in the Eosinophil Accumulation in EP
The constitutive and/or inducible expression of CCR1, CCR3, CCR5, CXC chemokine receptor (CXCR) 1, CXCR2, CXCR3, and CXCR4 in human peripheral blood eosinophils has been reported [23][28][29][30]. However, proteomic studies of eosinophils found or described only CCR1, CCR3, and CXCR4 as being present on human blood eosinophils [31][32]. Although the reason for this discrepancy is unknown, it may be due to differences in the methods of receptor expression measurement or eosinophil purification, or the characteristics of the donors, and so on. Among these receptors, CCR3 is highly and constitutively expressed on eosinophils. CCR3 ligands, such as eotaxin (CCL11), eotaxin-2 (CCL24), eotaxin-3 (CCL26), RANTES (CCL5), MCP-2 (CCL8), MCP-3 (CCL7), and MCP-4 (CCL13), can induce eosinophil recruitment in allergic inflammation [28]. Pretreatment of eosinophils with anti-CCR3 antibody diminishes their chemotactic response to CCR3 ligands in vitro [28]. Cellular sources of CC chemokines are likely epithelial cells, fibroblasts, and mononuclear cells [13][14][18][33]. Furthermore, Katoh et al. reported that the concentration of eotaxin was elevated in the BALF of EP patients [20]. Tateno et al. also reported that the concentration of eotaxin was increased in the BALF of CEP patients [21]. Therefore, CCR3 ligands, including eotaxin, may contribute to the pathogenesis of EP (Figure 1).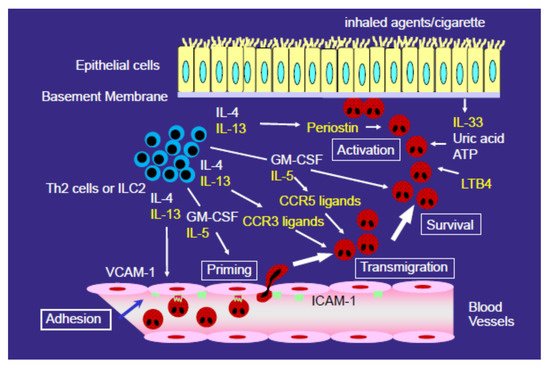
4. Role of Type 2 Cytokines (IL-4 and IL-13) in the Development of EP
IL-4 and IL-13 contribute to eosinophil accumulation in the airway; however, the accumulation is thought to be induced by an indirect mechanism, as it is generally accepted that IL-4 and IL-13 with physiological concentration do not activate eosinophils directly. We also confirmed that IL-4 and IL-13 do not activate eosinophil functions, such as adhesion or O2− generation, in vitro in eosinophils obtained from the blood of healthy volunteers (unpublished data). In contrast, IL-4 and IL-13 induced VCAM-1 expression in endothelial cells and the production of CCR3 ligands from epithelial cells, fibroblasts, and mononuclear cells (Figure 1), as described above. The levels of IL-13 and, in some reports, IL-4 are increased in the BALF of EP patients [39][40][41][42]. Therefore, IL-4 and IL-13 play roles in the accumulation of eosinophils in the lung, not by directly activating eosinophils, but by inducing VCAM-1 expression in endothelial cells and CCR3 ligand expression. In eosinophil-dominant severe asthma, anti-IL-4Rα mAb, which blocks both IL-4 and IL-13 signaling, strongly reduced acute exacerbations and increased lung function [43]. Furthermore, in severe chronic rhinosinusitis with nasal polyps, anti-IL-4Rα mAb reduced polyp sizes, sinus opacification, and the severity of symptoms [44]. Considering the role of IL-4/IL-13 in the development of eosinophilic airway inflammation, anti-IL-4/IL-13 treatment likely suppresses the accumulation of eosinophils in tissues in vivo, although it has not yet been established.References
- Cottin, V.; Cordier, J.F. Eosinophilic pneumonias. Allergy 2005, 60, 841–857.
- Suzuki, Y.; Suda, T. Eosinophilic pneumonia: A review of the previous literature, causes, diagnosis, and management. Allergol. Int. 2019, 68, 413–419.
- Allen, J.N.; Pacht, E.R.; Gadek, J.E.; Davis, W.B. Acute eosinophilic pneumonia as a reversible cause of noninfectious respiratory failure. N. Engl. J. Med. 1989, 321, 569–574.
- Carrington, C.B.; Addington, W.W.; Goff, A.M.; Madoff, I.M.; Marks, A.; Schwaber, J.R.; Gaensler, E.A. Chronic eosinophilic pneumonia. N. Engl. J. Med. 1969, 280, 787–798.
- O’Sullivan, J.A.; Bochner, B.S. Eosinophils and eosinophil-associated diseases: An update. J. Allergy Clin. Immunol. 2018, 141, 505–517.
- Yanagibashi, T.; Satoh, M.; Nagai, Y.; Koike, M.; Takatsu, K. Allergic diseases: From bench to clinic-Contribution of the discovery of interleukin-5. Cytokine 2017, 98, 59–70.
- Nair, P.; Pizzichini, M.M.; Kjarsgaard, M.; Inman, M.D.; Efthimiadis, A.; Pizzichini, E.; Hargreave, F.; O’Byrne, P.M. Mepolizumab for prednisone-dependent asthma with sputum eosinophilia. N. Engl. J. Med. 2009, 360, 985–993.
- Haldar, P.; Brightling, C.E.; Hargadon, B.; Gupta, S.; Monteiro, W.; Sousa, A.; Marshall, R.P.; Bradding, P.; Green, R.H.; Wardlaw, A.J.; et al. Mepolizumab and exacerbations of refractory eosinophilic asthma. N. Engl. J. Med. 2009, 360, 973–984.
- Pavord, I.D.; Korn, S.; Howarth, P.; Bleecker, E.R.; Buhl, R.; Keene, O.N.; Ortega, H.; Chanez, P. Mepolizumab for severe eosinophilic asthma (DREAM): A multicentre, double-blind, placebo-controlled trial. Lancet 2012, 380, 651–659.
- Wechsler, M.E.; Akuthota, P.; Jayne, D.; Khoury, P.; Klion, A.; Langford, C.A.; Merkel, P.A.; Moosig, F.; Specks, U.; Cid, M.C.; et al. EGPA Mepolizumab Study Team. Mepolizumab or Placebo for Eosinophilic Granulomatosis with Polyangiitis. N. Engl. J. Med. 2017, 376, 1921–1932.
- Sarkis, E.; Patel, S.; Burns, K.; Batarseh, H.; Mador, M.J. Anti-interleukin (IL)-5 as a steroid-sparing agent in chronic eosinophilic pneumonia. J. Asthma. 2018, 57, 1–5.
- To, M.; Kono, Y.; Yamawaki, S.; Soeda, S.; Katsube, O.; Kishi, H.; To, Y. A case of chronic eosinophilic pneumonia successfully treated with mepolizumab. J. Allergy Clin. Immunol. Pract. 2018, 6, 1746–1748.
- Nakagome, K.; Nagata, M. Involvement and Possible Role of Eosinophils in Asthma Exacerbation. Front. Immunol. 2018, 18, 2220.
- Nakagome, K.; Nagata, M. Pathogenesis of airway inflammation in bronchial asthma. Auris. Nasus. Larynx. 2011, 38, 555–563.
- Nagata, M.; Sedgwick, J.B.; Bates, M.E.; Kita, H.; Busse, W.W. Eosinophil adhesion to vascular cell adhesion molecule-1 activates superoxide anion generation. J. Immunol. 1995, 155, 2194–2202.
- Nagata, M.; Sedgwick, J.B.; Kita, H.; Busse, W.W. Granulocyte macrophage colony-stimulating factor augments ICAM-1 and VCAM-1 activation of eosinophil function. Am. J. Respir. Cell Mol. Biol. 1998, 19, 158–166.
- Nagata, M.; Sedgwick, J.B.; Vrtis, R.; Busse, W.W. Endothelial cells upregulate eosinophil superoxide generation via VCAM-1 expression. Clin. Exp. Allergy. 1999, 29, 550–561.
- Nagata, M.; Yamamoto, H.; Tabe, K.; Sakamoto, Y. Eosinophil transmigration across VCAM-1-expressing endothelial cells is upregulated by antigen-stimulated mononuclear cells. Int. Arch. Allergy Immunol. 2001, 125 (Suppl 1), 7–11.
- Ying, S.; Robinson, D.S.; Meng, Q.; Rottman, J.; Kennedy, R.; Ringler, D.J.; Mackay, C.R.; Daugherty, B.L.; Springer, M.S.; Durham, S.R.; et al. Enhanced expression of eotaxin and CCR3 mRNA and protein in atopic asthma. Association with airway hyperresponsiveness and predominant co-localization of eotaxin mRNA to bronchial epithelial and endothelial cells. Eur. J. Immunol. 1997, 27, 3507–3516.
- Katoh, S.; Matsumoto, N.; Fukushima, K.; Mukae, H.; Kadota, J.I.; Kohno, S.; Matsukura, S. Elevated chemokine levels in bronchoalveolar lavage fluid of patients with eosinophilic pneumonia. J. Allergy Clin. Immunol. 2000, 106, 730–736.
- Tateno, H.; Nakamura, H.; Minematsu, N.; Amakawa, K.; Terashima, T.; Fujishima, S.; Luster, A.D.; Lilly, C.M.; Yamaguchi, K. Eotaxin and monocyte chemoattractant protein-1 in chronic eosinophilic pneumonia. Eur. Respir. J. 2001, 17, 962–968.
- Nakagome, K.; Shoda, H.; Shirai, T.; Nishihara, F.; Soma, T.; Uchida, Y.; Sakamoto, Y.; Nagata, M. Eosinophil transendothelial migration induced by the bronchoalveolar lavage fluid of acute eosinophilic pneumonia. Respirology 2017, 22, 913–921.
- Kobayashi, Y.; Konno, Y.; Kanda, A.; Yamada, Y.; Yasuba, H.; Sakata, Y.; Fukuchi, M.; Tomoda, K.; Iwai, H.; Ueki, S. Critical role of CCL4 in eosinophil recruitment into the airway. Clin. Exp. Allergy. 2019, 49, 853–860.
- Liu, L.Y.; Sedgwick, J.B.; Bates, M.E.; Vrtis, R.F.; Gern, J.E.; Kita, H.; Jarjour, N.N.; Busse, W.W.; Kelly, E.A. Decreased expression of membrane IL-5 receptor alpha on human eosinophils: I. Loss of membrane IL-5 receptor alpha on airway eosinophils and increased soluble IL-5 receptor alpha in the airway after allergen challenge. J. Immunol. 2002, 169, 6452–6458.
- Liu, L.Y.; Sedgwick, J.B.; Bates, M.E.; Vrtis, R.F.; Gern, J.E.; Kita, H.; Jarjour, N.N.; Busse, W.W.; Kelly, E.A. Decreased expression of membrane IL-5 receptor alpha on human eosinophils: II. IL-5 down-modulates its receptor via a proteinase-mediated process. J. Immunol. 2002, 169, 6459–6466.
- Nagata, M.; Saito, K.; Tsuchiya, T.; Sakamoto, Y. Leukotriene D4 upregulates eosinophil adhesion via the cysteinyl leukotriene 1 receptor. J. Allergy Clin. Immunol. 2002, 109, 676–680.
- Saito, K.; Nagata, M.; Kikuchi, I.; Sakamoto, Y. Leukotriene D4 and eosinophil transendothelial migration, superoxide generation, and degranulation via β2 integrin. Ann. Allergy Asthma Immunol. 2004, 93, 594–600.
- Kitaura, M.; Nakajima, T.; Imai, T.; Harada, S.; Combadiere, C.; Tiffany, H.L.; Murphy, P.M.; Yoshie, O. Molecular cloning of human eotaxin, an eosinophil-selective CC chemokine, and identification of a specific eosinophil eotaxin receptor, CC chemokine receptor 3. J. Biol. Chem. 1996, 271, 7725–7730.
- Nagase, H.; Miyamasu, M.; Yamaguchi, M.; Fujisawa, T.; Ohta, K.; Yamamoto, K.; Morita, Y.; Hirai, K. Expression of CXCR4 in eosinophils: Functional analyses and cytokine-mediated regulation. J. Immunol. 2000, 164, 5935–5943.
- Jinquan, T.; Jing, C.; Jacobi, H.H.; Reimert, C.M.; Millner, A.; Quan, S.; Hansen, J.B.; Dissing, S.; Malling, H.J.; Skov, P.S.; et al. CXCR3 expression and activation of eosinophils: Role of IFN-γ-inducible protein-10 and monokine induced by IFN-γ. J. Immunol. 2000, 165, 1548–1556.
- Wilkerson, E.M.; Johansson, M.W.; Hebert, A.S.; Westphall, M.S.; Mathur, S.K.; Jarjour, N.N.; Schwantes, E.A.; Mosher, D.F.; Coon, J.J. The Peripheral Blood Eosinophil Proteome. J. Proteome Res. 2016, 15, 1524–1533.
- Larose, M.C.; Archambault, A.S.; Provost, V.; Laviolette, M.; Flamand, N. Regulation of Eosinophil and Group 2 Innate Lymphoid Cell Trafficking in Asthma. Front Med. 2017, 4, 136.
- Fujisawa, T.; Kato, Y.; Atsuta, J.; Terada, A.; Iguchi, K.; Kamiya, H.; Yamada, H.; Nakajima, T.; Miyamasu, M.; Hirai, K. Chemokine production by the BEAS-2B human bronchial epithelial cells: Differential regulation of eotaxin, IL-8, and RANTES by TH2- and TH1-derived cytokines. J. Allergy Clin. Immunol. 2000, 105, 126–133.
- White, J.R.; Imburgia, C.; Dul, E.; Appelbaum, E.; O’Donnell, K.; O’Shannessy, D.J.; Brawner, M.; Fornwald, J.; Adamou, J.; Elshourbagy, N.A.; et al. Cloning and functional characterization of a novel human CC chemokine that binds to the CCR3 receptor and activates human eosinophils. J. Leukoc. Biol. 1997, 62, 667–675.
- Lamkhioued, B.; Garcia-Zepeda, E.A.; Abi-Younes, S.; Nakamura, H.; Jedrzkiewicz, S.; Wagner, L.; Renzi, P.M.; Allakhverdi, Z.; Lilly, C.; Hamid, Q.; et al. Monocyte chemoattractant protein (MCP)-4 expression in the airways of patients with asthma. Induction in epithelial cells and mononuclear cells by proinflammatory cytokines. Am. J. Respir. Crit. Care Med. 2000, 162, 723–732.
- Mueller, A.; Strange, P.G. The chemokine receptor, CCR5. Int. J. Biochem. Cell Biol. 2004, 36, 35–38.
- Wells, T.N.; Power, C.A.; Shaw, J.P.; Proudfoot, A.E. Chemokine blockers-therapeutics in the making? Trends Pharmacol. Sci. 2006, 27, 41–47.
- Fuchimoto, Y.; Kanehiro, A.; Miyahara, N.; Koga, H.; Ikeda, G.; Waseda, K.; Tanimoto, Y.; Ueha, S.; Kataoka, M.; Gelfand, E.W.; et al. Requirement for chemokine receptor 5 in the development of allergen-induced airway hyperresponsiveness and inflammation. Am. J. Respir. Cell Mol. Biol. 2011, 45, 1248–1255.
- Katoh, S.; Matsumoto, N.; Matsumoto, K.; Fukushima, K.; Matsukura, S. Elevated interleukin-18 levels in bronchoalveolar lavage fluid of patients with eosinophilic pneumonia. Allergy 2004, 59, 850–856.
- Miyazaki, E.; Nureki, S.; Fukami, T.; Shigenaga, T.; Ando, M.; Ito, K.; Ando, H.; Sugisaki, K.; Kumamoto, T.; Tsuda, T. Elevated levels of thymus- and activation-regulated chemokine in bronchoalveolar lavage fluid from patients with eosinophilic pneumonia. Am. J. Respir. Crit. Care Med. 2002, 165, 1125–1131.
- Mato, N.; Bando, M.; Kusano, A.; Hirano, T.; Nakayama, M.; Uto, T.; Nakaya, T.; Yamasawa, H.; Sugiyama, Y. Clinical significance of interleukin 33 (IL-33) in patients with eosinophilic pneumonia. Allergol. Int. 2013, 62, 45–52.
- Nakagome, K.; Nakamura, Y.; Kobayashi, T.; Ohta, S.; Ono, J.; Kobayashi, K.; Ikebuchi, K.; Noguchi, T.; Soma, T.; Yamauchi, K.; et al. Elevated Periostin Concentrations in the Bronchoalveolar Lavage Fluid of Patients with Eosinophilic Pneumonia. Int. Arch. Allergy Immunol. 2019, 178, 264–271.
- Castro, M.; Corren, J.; Pavord, I.D.; Maspero, J.; Wenzel, S.; Rabe, K.F.; Busse, W.W.; Ford, L.; Sher, L.; FitzGerald, J.M.; et al. Dupilumab Efficacy and Safety in Moderate-to-Severe Uncontrolled Asthma. N. Engl. J. Med. 2018, 378, 2486–2496.
- Bachert, C.; Han, J.K.; Desrosiers, M.; Hellings, P.W.; Amin, N.; Lee, S.E.; Mullol, J.; Greos, L.S.; Bosso, J.V.; Laidlaw, T.M.; et al. Efficacy and safety of dupilumab in patients with severe chronic rhinosinusitis with nasal polyps (LIBERTY NP SINUS-24 and LIBERTY NP SINUS-52): Results from two multicentre, randomised, double-blind, placebo-controlled, parallel-group phase 3 trials. Lancet 2019, 394, 1638–1650.
