In contrast to exogenous electrophiles and ROS, the mechanism of Nrf2 activation by mitochondrial ROS production may be more complicated considering that superoxide and H
2O
2 produced in the mitochondrial matrix do not easily diffuse into the cytoplasm
[20][32] and that generated mitochondrial superoxide is efficiently converted to H
2O in mitochondria
[21][33]. Generally, various mitochondrial abnormalities can be signaled to the cytosol by non-ROS-related mechanisms, as seen in mitochondrial retrograde signaling, such as in the
C. elegans ATFS-1 system, in which the drop in membrane potential inhibits peptide transport activity and proteolysis, leading to the nuclear translocation of ATFS-1
[22][34]. Regarding Nrf2, it has been reported that alterations in complex I activity may determine Nrf2 gene expression via the ERK5-myocyte enhancer factor 2 (MEF2) pathway in a ROS-independent manner
[23][24][27,35]. However, several reports have shown that changes in mtROS generation through alterations of the level of SOD2
[25][36] or mitochondria-localized paraquat
[26][37] actually change the cellular response, indicating that alterations in mtROS actually signals to the cytosol using unknown signaling mediators or cascades.
It is known that mtROS activates Nrf2. Oxidation of the extracellular environment by a low cysteine/cystine ratio increases both cellular and mtROS levels and activates Nrf2 in NIH 3T3 mouse embryonic fibroblasts (MEFs)
[27][38]. Although it is unclear how ROS are produced in this system, cellular ROS elevation and Nrf2 activation are suppressed in mitochondria-specific thioredoxin-2 transgenic MEFs, indicating that Nrf2 activation is somehow induced by mtROS
[27][38]. Piantadosi et al. showed that Nrf2 is also involved in carbon monoxide (CO)-induced mitochondrial biogenesis in the heart
[16]. CO is endogenously generated by heme oxygenase-1 (HO-1), and HO-1 overexpression stimulates mitochondrial H
2O
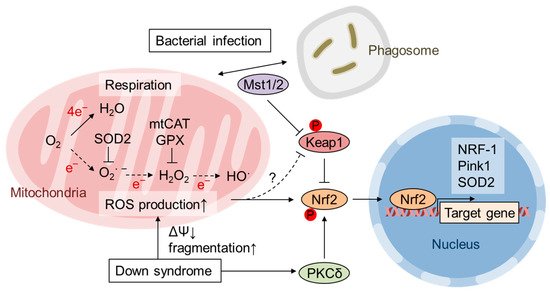
2 production, which activates the Akt-GSK3β-Nrf2 pathway. Nrf2 activates the transcription of NRF-1 by directly binding to ARE in the NRF-1 promoter. Zamponi et al. demonstrated that Nrf2 activation counteracts ROS-mediated deterioration effects in human fibroblasts from Down syndrome (DS) patients as well as in MEFs from Dp16 mice, a model of DS with segmental trisomy
[14]. DS fibroblasts and Dp16 MEFs exhibit an increase in both cytoplasmic and mtROS and impaired mitochondrial membrane potential and fragmentation. DS cells exhibit increased cellular accumulation of Nrf2 and its target gene
HO-1, and activation of PKCδ by caspase-3-dependent cleavage is responsible for Nrf2 activation via Ser40 phosphorylation. The transgenic expression of catalase fused to a mitochondrial targeting signal (mtCAT) in mice demonstrated that mitochondrial H
2O
2 elimination prolongs lifespan and suppresses age-associated diseases, including nonhematopoietic malignancy, decreased cardiac and skeletal muscle function, lipid-induced insulin resistance, and abnormal amyloid β production
[28][29][30][31][32][39,40,41,42,43]. Similarly, the expression of mtCAT in DS cells reduces both cytoplasmic and mitochondrial ROS and restores mitochondrial dysfunction as well as Nrf2 phosphorylation and accumulation
[14] (). Nrf2 is activated in macrophages during the immune response to protect them from the marked ROS production required to eliminate pathogens
[15]. Geng et al. showed that the kinases Mst1 and Mst2 are necessary for the colocalization of mitochondria and phagosomes so that sufficient ROS are produced for bactericidal activity
[33][44]. Although Mst1/Mst2-deficient macrophages fail to produce ROS in response to Toll-like receptor stimulation, they show increases in basal ROS levels, protein oxidation, DNA damage and apoptosis
[15]. Bacterial infection and mitochondrial ROS production induce the translocation of Mst1/Mst2 from the cytosol to mitochondria. Keap1 is also translocated to mitochondria and phosphorylated by Mst1/Mst2 at four Ser/Thr residues in its N-terminus that disable Keap1 dimerization and activate Nrf2
[15] (). Thus, these observations suggest that mitochondrial ROS activate Nrf2 mostly by indirect and kinase-dependent mechanisms.
3. Role of mtROS and Nrf2 in Mitohormesis
“Free radical theory” of aging by Harman et al. propose that ROS production and accumulation, which was mainly produced by the disturbed mitochondrial function during aging, causes DNA mutations and degenerative diseases
[34][45]. However, it is becoming clear that small amount of ROS act as signaling molecules in the cells and they elicit health-promoting effects. Reduced glucose metabolism or impaired insulin/IGF signaling alters mitochondrial metabolism to extend life span in various model organisms
[3]. MtROS acts as a signaling molecule in these setting to activate beneficial retrograde signaling that regulates mitochondrial dynamics, quality control, proteostasis, biogenesis, and the cellular defense system. In the field of toxicology or radiation medicine, hormesis refers to the preconditioning events in which a subtoxic dose of a substance provokes an endogenous cytoprotective response and confers resistance against later higher amounts of the same toxicants. Patrick Tapia proposed the concept of “mitohormesis” such that weak mitochondrial stress mediates beneficial outcomes of calorie restriction, intermittent fasting, exercise, and dietary phytochemicals with accompanying stoichiometric amount of ROS being essential for the response
[35][46]. The theory was supported by following studies and now multiple pathways are known to mediate the mitohormetic response
[3][36][3,47]. Mitochondrial stress accompanies not only ROS production and ATP decline, but also accumulation of unfolded protein, decrease in Ca
2+ buffering, and alteration in metabolite of TCA cycle, OxPhos, fatty acid oxidation, etc.
[37][48]. Ca
2+ release from mitochondria in muscle during exercise stimulates mitochondrial respiration and biogenesis via calmodulin-dependent protein kinase and calcineurin
[38][49]. An increase in the NAD
+/NADH and AMP/ATP ratio and a decrease in insulin/IGF signaling or mechanistic target of rapamycin (mTOR) signaling may mediate cellular adaptive responses leading to mitohormesis
[3][39][3,50]. The NAD
+-dependent deacetylase Sir2 is reported to promote longevity in yeast
[40][41][51,52] as well as
C. elegans and
Drosophila [42][43][53,54]. In mammals, there are 7 Sir2 homolog family members, SIRT1-SIRT7, which have diverse functions in various organelles
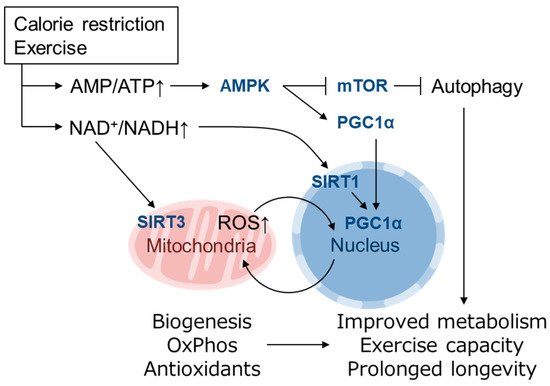
[39][50]. Mitochondrial biogenesis induced by a low energy state is mediated by PGC1α, which is a transcriptional cofactor of PPARγ, ERRα, FoxO1 as well as NRF-1
[44][45][55,56]. PGC1α is regulated by both transcriptional and posttranslational modifications, the latter of which includes phosphorylation by AMPK (activated by high AMP/ATP ratio) and deacetylation by SIRT1 (activated by high NAD
+/NADH ratio)
[39][44][50,55] (). Recently, it was reported that PGC1α activity is also regulated by oxygen availability via Lys224 demethylation by the oxygen-dependent demethylase KDM3A
[46][57]. The inhibition of mTOR complex 1 (mTORC1) by AMPK as well as amino acid starvation induces autophagy, which is also involved in longevity in yeast, invertebrates and mice
[47][58]. Mitochondrial biogenesis is also induced by physical exercise
[48][49][59,60] and has been proposed to extend lifespan, at least in part, by activating the same pathways
[3]. Increased NAD
+/NADH also activates the mitochondrially localized family member SIRT3, which up-regulates ATP synthesis by activating enzymes in the TCA cycle, ETC and fatty acid oxidation and contributes to antioxidant defense by SOD2 induction via FoxO1 deacetylation
[50][61] (). Mitochondrial unfolded protein response (UPR
MT) is also thought as a mitohormetic machinery
[51][62]. In UPR
MT, expression of mitochondrial chaperones and proteases is up-regulated in response to mtDNA depletion
[52][63] and inhibition of mitochondrial chaperone TRAP1 or protease LONP1
[53][64]. UPR
MT in nematode is mediated by ATFS-1 as described above
[22][34], whereas mammalian UPR
MT is thought to be regulated by ATF4, ATF5 and CHOP
[54][65].
Figure 2. Mitohormesis caused by mild metabolic stress elicits an antioxidant defense response. Metabolic stress, such as caloric restriction and exercise, causes a decline in ATP levels and an increase in the NAD
+/NADH ratio that is sensed by downstream pathways that promote mitochondrial function and increase ATP synthesis
[39][44][50,55]. An increase in AMP/ATP activates AMPK, which induces mitochondrial biogenesis via PGC1α activation and enhances autophagy via mTOR inhibition. An increase in NAD
+/NADH activates the NAD
+-dependent deacetylases SIRT1 and SIRT3
[50][61]. Mitochondrially localized SIRT3 activates enzymes involved in mitochondrial ATP synthesis, whereas nuclear SIRT1 also activates PGC1α
[39][44][50,55]. PGC1α activates the expression of genes involved in mitochondrial biogenesis, fatty acid oxidation, oxidative phosphorylation (OxPhos) and the antioxidant defense system. These adaptations resolve energy shortages and improve metabolic health, exercise capacity and longevity
[3].
In
C. elegans, skinhead-1 (SKN-1) is the functional homolog of mammalian Nrf1 and Nrf2; however, SKN-1 activation by oxidative stress is mediated by p38 MAPK because Keap1 is absent in
C. elegans [55][66]. SKN-1 promotes longevity in wild-type worms and is necessary for longevity extension by multiple pathways, including reduced insulin/IGF-1 signaling (DAF2), mTOR inhibition, and dietary restriction
[55][66]. In contrast, few reports have investigated the role of Nrf2 in the mitohormesis-like response in mammals. Pulliam et al. reported Nrf2 activation in mice lacking surfeit locus protein 1 (
SURF1), an assembly factor of cytochrome c oxidase (COX/Complex IV) encoded in the nuclear genome
[56][67]. Loss-of-function mutations in the
SURF1 gene lead to mitochondrial disease and Leigh syndrome in humans
[57][68].
Surf1-KO mice exhibit decreased COX activity in most tissues and reduced endurance capacity but no neurodegeneration symptoms. Interestingly,
Surf1-KO mice are resistant to kainic acid-induced neurotoxicity and show a prolonged lifespan
[56][58][67,69].
Surf1-KO mice show a decrease in mitochondrial ROS and an increase in mitochondrial number and PGC1α expression in both heart and skeletal muscle.
Nrf2 and
HO-1 expression is elevated in the heart, whereas the expression of UPR
MT genes,
Hsp60,
ClpP, and
Lonp1, is increased in skeletal muscle
[56][67]. Cox et al. revealed that the temporary depletion of SOD2 expression in embryogenesis potentiates Nrf2 signaling in later developmental stages
[13]. The authors showed that inducible shRNA-mediated SOD2 knockdown during embryonic days 8.5-12.5 increased oxidative stress hallmarks and reduced aconitase activity without newborn lethality. The adapted mouse livers had restored SOD2 expression and aconitase activity and exhibited decreased mitochondrial respiration, decreased ROS levels, and increased mitochondrial content at 4 weeks old. The gene expression profile identified a gene subset with increased expression in which cis elements of PPARγ, PGC1α and Nrf2 were significantly enriched. These responses were also observed in SOD2-knockdown MEFs. When the down-regulated SOD2 expression was restored after transient SOD2-knockdown, MEFs exhibited increased mitochondrial content, Nrf2 target gene expression induction, and reduced maximal respiration and were resistant to menadione-induced oxidative stress. This adaptive response possibly remodels mitochondrial function so that ROS production is reduced by the increased number of mitochondria and restricted respiration rate as well as increased antioxidant defense response
[13]. The molecular mechanisms by which Nrf2 activation is achieved and is maintained for a prolonged period after transient stress stimulation remain to be clarified.