Coenzyme Q10 (CoQ10) is a ubiquitous factor present in cell membranes and mitochondria, both in its reduced (ubiquinol) and oxidized (ubiquinone) forms. Its levels are high in organs with high metabolism such as the heart, kidneys, and liver because it acts as an energy transfer molecule but could be reduced by aging, genetic factors, drugs (e.g., statins), cardiovascular (CV) diseases, degenerative muscle disorders, and neurodegenerative diseases. As CoQ10 is endowed with significant antioxidant and anti-inflammatory features, useful to prevent free radical-induced damage and inflammatory signaling pathway activation, its depletion results in exacerbation of inflammatory processes. Therefore, exogenous CoQ10 supplementation might be useful as an adjuvant in the treatment of cardiovascular diseases such as heart failure, atrial fibrillation, and myocardial infarction and in associated risk factors such as hypertension, insulin resistance, dyslipidemias, and obesity.
1. Introduction
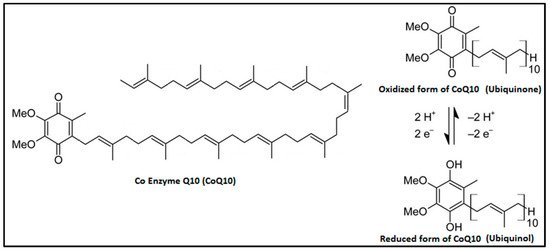
Coenzyme Q
10 (CoQ
10) is an organic molecule that was identified for the first time by Frederick Crane of Wisconsin (USA) in 1957
[1]. It is ubiquitously present in cell membranes and especially in the mitochondria in both reduced (ubiquinol) and oxidized (ubiquinone) forms (). Chemically, it is constituted of a benzoquinone group and a poly-isoprenoid side chain that is species specific. In the human, it is composed of 10 units and called CoQ
10 or ubiquinone
[2]. This molecule can sustain continuous oxidation–reduction cycles and is an excellent electron carrier. CoQ
10 concentration is particularly high in organs such as the kidneys, heart, and liver () because they need it as an efficient energy transfer molecule supporting their high metabolic rate
[3].
Figure 1. Chemical structure of CoQ10.
Table 1. Distribution of ubiquinone and ubiquinol in human tissues (modified from References
[4][5][4,5]).
| Organ |
Ubiquinone Concentration (µg/g) |
Ubiquinol Concentration (µg/g) |
| Heart |
132.0 |
61.0 |
| Kidneys |
77.0 |
75.0 |
| Liver |
63.6 |
95.0 |
| Muscle |
39.7 |
65.0 |
| Brain |
13.4 |
23.0 |
| Pancreas |
32.7 |
|
| Spleen |
24.6 |
|
| Lung |
7.9 |
25.0 |
| Thyroid |
24.7 |
|
| Testis |
10.5 |
|
| Intestine |
11.5 |
95.0 |
| Colon |
10.7 |
|
| Ventricle |
11.8 |
|
| Plasma (µmol/mL) |
1.1 |
96.0 |
Physiologically, CoQ
10 is anchored in the cell membrane through the isoprenoid tail, whereas the benzoquinone ring moves in the membrane based on its redox state. The most prominent role of CoQ
10 is to facilitate the production of ATP through participation in the electron transport chain in the mitochondria. In fact, in the respiratory chain, CoQ
10 transfers electrons from complex I (nicotinamide-adenine dinucleotide (NADH)-coenzyme Q reductase) or complex II (succinate-coenzyme Q reductase) to complex III (cytochrome c reductase), and it is also a structural component of both CI and CIII, reducing the production of reactive oxygen species (ROS)
[6][7][6,7].
Moreover, CoQ
10 is able to accept electrons from fatty acyl-coenzyme A (acyl-CoA) dehydrogenases and it is an obligatory factor in proton transport by uncoupling proteins (UCPs), thus regulating the opening of mitochondrial permeability transition pores
[8]. Other functions of CoQ
10 in the cell membrane include stabilization of calcium-dependent channels, metabolic regulation, cell signaling, and cell growth through local regulation of cytosolic redox intermediates such as dihydronicotinamide-adenine dinucleotide phosphate (NADPH)
[6].
CoQ
10, in its reduced form, has been shown to inhibit the peroxidation of cell membrane lipids and to reduce the oxidation of circulating lipids. Interestingly, in vitro, it inhibits the oxidation of low-density lipoprotein more than other antioxidant molecules, such as α-tocopherol or β-carotene
[9][10][9,10].
CoQ
10 is mostly synthetized in the cell, although the pathway involved is not yet completely known. A biosynthetic complex for producing CoQ
10, containing proteins, lipids, and polar small molecules (but with specific composition unknown), was recently revealed in yeast and mammals. In particular, multiple mitochondrial uncharacterized proteins (MXPs) have been linked to CoQ
10 biosynthesis and recent progress was made also toward understanding the biochemistry of a dehydrogenase, a deaminase, a lipid-binding protein, and a protein kinase-like enzyme in the CoQ
10 pathway
[11]. In mammalians, 4-hydroxybenzoate is the precursor of the quinone ring, derived from tyrosine, while the isoprenoid tail is derived from the mevalonate pathway, using the common way with cholesterol biosynthesis. The final step, rate limiting, occurs in the mitochondrial matrix
[12][13][12,13].
On the other hand, CoQ
10 can be derived from the diet; in particular, fatty fish (salmon, sardin, and tuna), soya, spinach, and nuts contain high levels of this cofactor. However, the intake from the diet is significant only in deficiency conditions
[14]. Some factors may reduce plasma concentrations of CoQ
10, such as aging, genetic factors, drugs (e.g., statins), certain diseases (e.g., cardiovascular disease and degenerative muscle disorders), and increased demand
[15].
Therefore, it is not surprising that its depletion is associated with a greater propensity to develop immune inflammatory responses through the activation of inflammatory processes such as the nuclear factor-kappa-light-chain-enhancer of activated B cell’s (NF-κB) gene expression
[16]. Worthy to note, CoQ
10 is endowed with potent antioxidant action able to prevent free radical damage by the regulation of transcriptional pathways in addition to deactivation of inflammatory pathways
[17]. Therefore, supplementation with CoQ
10 could be efficient in the prevention and/or treatment of a number of pathogenic disorders in relation to the significant reduction of inflammatory markers
[18].
Due to its important place in organisms’ functioning, there are many diseases and degenerative states associated with CoQ
10′s deficiency, such as cardiovascular disease, muscular dystrophy, Alzheimer’s disease, Parkinson’s disease, and others
[7]. However, if on the one hand clinical evidences in the cardiovascular field have demonstrated the potential role of CoQ
10, data concerning the supplementation of this nutraceutical in neurodegenerative diseases and other conditions such as cancer or muscular dystrophy are often old and still conflicting and need additional randomized controlled trials (RCTs)
[19][20][21][19,20,21].
2. CoQ10 and Cardiovascular Risk Factors
As stated above, CoQ
10 supplementation could find a role in the management of some highly prevalent cardiovascular and cerebrovascular disease risk factors, such as high blood pressure, insulin resistance, dyslipidemia, migraine, and chronic kidney disease.
2.1. High Blood Pressure
Hypertension is one of the major causes of morbidity and mortality worldwide, involving one in four men and one in five women, totalling 1.13 billion adults, who had raised blood pressure in 2015
[22]. A recent comparative assessment of the risk of health loss related to systolic blood pressure (SBP), based on 844 studies in 154 countries (published between 1980 and 2015) and 8.69 million participants, has estimated approximately 874 million of people in the world with SBP above 140 mmHg
[23]. In 2025, it is estimated that there will be approximately 1.56 billion hypertensive adults
[24].
CoQ
10 seems to exert a direct effect on the endothelium, provoking vasodilation and lowering blood pressure
[25][26][25,26]. This effect is linked to its ability to improve nitric oxides bioavailability and to induce vasodilatation especially in patients with hypertension. In addition, CoQ
10 adjusts the angiotensin effect in sodium retention and decreases the level of aldosterone
[27][28][27,28]. Despite exciting blood pressure results observed in preliminary trials (systolic and diastolic blood pressure reduced respectively by 6 and 5 mmHg vs. placebo)
[29] and the positive results confirmed by old meta-analyses of RCTs
[30][31][30,31], a recent meta-analysis of 17 randomized controlled trials including 684 subjects showed that CoQ
10 supplementation significantly decreased systolic blood pressure (Standardized Mean Difference (SMD) −0.30; 95%CI −0.52, −0.08), but not diastolic blood pressure (SMD −0.08; 95%CI −0.46, 0.29)
[32]. However, in patients with type 2 diabetes mellitus and ischemic left ventricular systolic dysfunction, when the blood pressure is on target, the supplementation of CoQ
10 did not modify the blood pressure
[33][34][35][33,34,35]. In conclusion, despite some promising evidence, the antihypertensive effect of CoQ
10 is still unclear in patients with primary hypertension
[36][37][36,37].
2.2. Insulin-Resistance and Type 2 Diabetes
Mitochondria seem to play a key role in the development of insulin resistance. They are well known to convert nutrients from diet such as fats and sugars into ATP; however, ATP production can generate harmful intermediates such as ROS and the increase in the amount of oxidant agents produced in mitochondria has been linked to the increase of insulin resistance
[38][39][38,39]. Several studies in vitro and in vivo as well
[40] found that the concentrations of CoQ
10 were lower in mitochondria from insulin-resistant fat and muscle tissue, probably for a change in expression of mevalonate/CoQ
10 pathway proteins and thus altered CoQ
10 metabolism, suggesting a direct correlation between the low levels of CoQ
10 and the high levels of oxidants in the mitochondria. In addition, the administration of CoQ
10 in deficient and insulin resistant mice has been shown to improve the insulin sensitivity by reducing ROS levels
[40].
In patients with metabolic syndrome (MetS), a condition typically caused by insulin-resistance and strongly associated with the risk to developing cardiovascular disease, the intake of 100 mg/day of CoQ
10 for 8 weeks significantly improved Homeostatic Model Assessment of Insulin Resistance (HOMA-IR), Homeostatic Model Assessment of β-cell Function (HOMA-B), serum insulin levels, and plasma total antioxidant capacity
[41]. The effect of CoQ
10 on insulin-resistance seems to not be related to its effect on body fat. In fact, a recent meta-analysis of RCTs showed that CoQ
10 had no significant impact on body weight (
p = 0.64) and body mass index (BMI) (
p = 0.86), independent from the CoQ
10 tested dosage and trial duration
[42].
Another highly prevalent cardiovascular risk factor related to insulin-resistance is nonalcoholic fatty liver disease (NAFLD)
[43]. Despite the numerous mechanisms investigated, the exact biological one related to increased hepatic inflammation and fat accumulation in NAFLD remains largely unknown
[44][45][44,45]. However, recent studies have focused attention on the role of mitochondrial protein mitofusin 2 (Mfn2) that protects against liver disease. In fact, reduced Mfn2 expression was detected in liver biopsies from patients with nonalcoholic steatohepatitis
[46]. The loss of Mfn2 seems to impair mitochondrial respiration and to reduce ATP production, and this defective oxidative phosphorylation process seems to unexpectedly originate from a depletion of the mitochondrial CoQ
10 pool
[47].
To date, the treatment of NAFLD is essentially based on lifestyle optimization because there are currently no specific drugs approved on the market for this condition. At the same time, few nutraceuticals have been adequately studied for their effects on NAFLD
[48]. Among these, CoQ
10 is a well-known anti-adipogenic molecule and thus could have a positive impact on NAFLD, even if its exact mechanism is still unclear. It is possible that CoQ
10 downregulates the expression of fatty acid synthase (FAS), sterol regulatory element-binding protein-1c (SREBP-1c), and acetyl-CoA carboxylase (ACC), which are related to lipid synthesis, and increases in the expression of carnitine palmitoyltransferase-1 (CPT-1) and peroxisome proliferator-activated receptors α (PPARα) associated with fatty acid oxidation
[49]. In addition, CoQ
10 could change the response to inflammation through nuclear factor kappa B (NF-kB)-dependent gene expression
[50]; thus, its deficiency might have a role in increasing levels of inflammatory molecules like NF-kB
[51].
CoQ
10 could serve as an adenosine monophosphate-activated protein kinase (AMPK) activator and could regulate the hepatic lipid metabolism to inhibit the abnormal accumulation of hepatic lipids as well as to prevent NAFLD progression
[49]. Finally, CoQ
10 was also found to bind and activate both PPARs alpha and gamma, suggesting a key role in relaying the states of mitochondria and peroxisomes
[52]. At the same time, the experiments performed with peroxisomal inducers indicate that nuclear receptors are involved in the regulation of CoQ
10 biosynthesis
[13].
In an RCT, 41 subjects with NAFLD were randomly divided into 2 groups to receive CoQ
10 (100 mg/day) or placebo for 12 weeks. At the end of the study, the active group benefited from a significant decrease in aspartate aminotransferase (AST), gamma-glutamyl transpeptidase (GGT), tumor necrosis factor α, high-sensitivity C-reactive protein (hs-CRP), and NAFLD grade compared to placebo (
p < 0.05 for all). In addition, patients who received the CoQ
10 supplement had higher serum levels of adiponectin (
p = 0.016) even if serum leptin levels reduced marginally (
p = 0.053)
[53]. However, CoQ
10 administration (300 mg/day for 12 weeks) in patients with coronary artery disease did not find any significant effect on serum adiponectin levels
[54], confirming previous data obtained by Gokbel et al. with the supplementation of CoQ
10 100 mg/day in healthy volunteers
[55]. In another RCT, the same dose of CoQ
10 in 44 NAFLD patients for 4 weeks was associated with significantly decreased waist circumference (WC), serum AST, and total antioxidant capacity (TAC) concentration (
p < 0.05 for all)
[56].
CoQ
10 could also improve the atherogenic dyslipidemia typically associated with NAFLD (reducing triglycerides (TG) and increasing high-density lipoprotein cholesterol (HDL-C) as well as reduce oxidized low-density lipoprotein (LDL) levels and arterial pressure with a very high safety profile and without any risk of drug interactions
[15]. In conclusion, the studies conducted to date emphasize a potential for CoQ
10 therapy in improving several anthropometric and biochemical variables in NAFLD.
A further disease typically characterized by insulin resistance is polycystic ovary syndrome (PCOS). In these women, as showed by the study of Samimi et al., the supplementation with CoQ
10 (100 mg/day) for 12 weeks could have beneficial effects on glucose metabolism and on serum total- and LDL-cholesterol levels
[57]. Afterwards, the same research group carried out another RCT on 40 women with a diagnosis of PCOS, observing that a supplementation for 12 weeks with CoQ
10 (100 mg/day), beside the positive effects on lipid and glucose levels, was responsible for a downregulation of gene expression of oxidized low-density lipoprotein (LDL) receptor 1 (
p < 0.001) and an upregulated gene expression of PPAR-γ (
p = 0.01) in peripheral blood mononuclear cells. In addition, compared to the placebo group, CoQ
10 supplementation downregulated gene expression of interleukin-1 (IL-1) (
p = 0.03), IL-8 (
p = 0.001), and tumor necrosis factor-alpha (TNF-α) (
p < 0.001) in peripheral blood mononuclear cells of subjects with PCOS
[58]. Similar results were obtained by Izadi et al. in a RCT of 85 PCO women treated with CoQ
10 and/or vitamin E or placebo. In particular, CoQ
10 alone improved the sex homone profile, specially either reduced testosterone and luteinizing hormone (LH) levels, and improved insulin resistence. Moreover, it is noteworthy that CoQ
10 in coadministration with alfa-tocopherol presented a more pronunced effect and stimulated the release of sex hormone-binding globulin (SHBG), justifing the enhancement of insulin tolerance, since an insulin resistance condition is associated with a reduced synthesis of SHBG at the hepatic level. Then, CoQ
10 might promote steroid hormone biosynthesis and normal reproductive function (among which are oocyte maturation, fertilization, and embryonic development) through the improvement of mitochondrial functionality
[59]. However, new, larger RCTs are needed to confirm the results obatined by Izadi et al.
The extreme consequence of insulin-resistance is Type 2 diabetes (T2DM). A deficiency of CoQ
10 plasma levels in patients with T2DM can be observed compared to healthy people
[60][61][60,61]. In particular, the ubiquinone–ubiquinol ratio, a validated marker of oxidative stress
[62], is much higher in a patient with T2DM after breakfast and throughout the day, which suggests heightened oxidative stress in the background of postprandial hyperglycemia
[63]. In a recent pooled analysis of 14 trials including 693 overweight diabetic patients, CoQ
10 interventions significantly reduced fasting plasma glucose (FPG) (−0.59 mmol/L; 95%CI −1.05 to −0.12;
p = 0.01), HbA1c (−0.28%; 95%CI −0.53 to −0.03;
p = 0.03), and TG levels (0.17 mmol/L; 95%CI −0.32 to −0.03;
p = 0.02). Even in the subgroup analysis, the low-dose consumption of CoQ
10 (<200 mg/d) effectively reduced the values of FBG, HbA1c, fasting blood insulin, homeostatic model assessment for insulin resistance (HOMA-IR), and TG with high tolerability profile
[64]. In a rat model, the administration of metformin combined with CoQ
10 showed a better renoprotective effect than CoQ
10 or metformin alone
[65]. This is also confirmed for other oral antidiabetic drugs like sitagliptin
[66]. This brings up an important point that CoQ
10 may potentiate the protective effects of some conventional treatments, but it is yet to be demonstrated in humans.
2.3. Dyslipidemias
Several mechanisms have been proposed by which CoQ
10 supplements could improve metabolic profiles which probably might be through the induction of gene expression of PPAR-γ
[67], a nuclear receptor protein that regulates gene expression involved in insulin and lipid metabolism, differentiation, proliferation, survival, and inflammation
[68]. In human endothelial cells, the exposure to CoQ
10 is associated with downregulation of the lectin-like oxidized LDL receptors, stimulation of the AMPK, and reduction of the ROS-induced endothelial damage
[69]. In fact, the main effect of CoQ
10 on plasma lipids seems to be the increased LDL resistance to oxidative stress
[70], as also demonstrated in healthy adults after acute strenous physical exercise
[71].
In an RCT, 101 dyslipidemic subjects without taking any lipid-lowering drugs were administrated 120 mg CoQ
10 or placebo daily for 24 weeks. At the end of the study, CoQ
10 supplementation mildly reduced TG (
p = 0.020) and LDL-C (
p = 0.016), increased apolipoprotein (Apo)A-I (
p < 0.001) and serum total antioxidant capacity (TAC;
p = 0.003), while decreased homeostasis model assessment of insulin resistance index (
p = 0.009) compared to placebo
[24]. In the meta-analysis conducted by Sharifi et al.
[72], CoQ
10 administration to patients with metabolic diseases mildly but significantly reduced TG concentrations (SMD −0.28 mmol/L; 95% CI, −0.56 to −0.005,
p = 0.001). A recent meta-analysis including six clinical trials suggests that CoQ
10 could mildly reduce the lipoprotein (a) plasma level
[73]. Overall, the effect of CoQ
10 supplementation on plasma lipid levels is, however, quantitatively small and its clinical relevance has yet to be demonstrated.
2.4. Systemic Inflammation
Inflammation is considered a main process involved in atherosclerosis development
[74]. A recent meta-analysis of nine RCTs and 509 patients showed that the CoQ
10 supplementation in chronic inflammatory diseases (60–500 mg/day for 8–12 weeks) is responsible for the significant reduction in the plasma levels of tumor necrosis factor alpha (TNF-α) (SMD: −0.44, 95% CI: (−0.81 to −0.07) mg/dl;
I2 = 66.1%,
p < 0.01) and in IL-6 levels (SMD: −0.37, 95% CI: (−0.65 to −0.09),
p = 0.01)
[75]. Similar results were obtained by the metanalysis of Fan et al. that demonstrated a reduction of the C-reactive protein levels in addition to the abovementioned parameters in patients afflicted by inflammatory diseases
[76]; in elderly people with low CoQ
10 levels; and in patients with metabolic diseases characterized by chronic, low grade inflammation
[17]. However, the results are conflicting while not so evident in patients affected by metabolic syndrome
[41] and dyslipidemia
[29].
3. CoQ10 and Cardiovascular Disease
CoQ
10 supplementation has been tested in a number of overt cardiovascular diseases, with the aim to evaluate its impact on self-perceived quality of life, instrumental parameters, and sometimes clinical outcomes as well.
3.1. CoQ10 and Heart Failure (HF)
HF is defined by the American Heart Association (AHA)/American College of Cardiology (ACC) guidelines as “a complex clinical syndrome that can result from any structural or functional cardiac disorder that impairs the ability of the ventricle to fill or eject blood”
[77][78][77,78]. It affects 23 million people worldwide
[79], and the HF prevalence in the USA is 5 million people
[80]. At the same time, this disease is also the main component for disability and hospitalization in the elderly and it is the cause of one in nine deaths in the USA
[1]. In Europe, the prevalence and incidence of HF and the related costs are quite similar
[81][82][81,82]. Despite that, in the last decades, the prevention and treatment of HF have improved significantly, quality of life is often impaired, and mortality rates are greater than 10% per year, reaching 20%–50% in more serious patients
[83]. In the last years, a number of clinical studies have investigated the possibility that CoQ
10 can contribute to the prevention of incident HF and to the improvement of related symptoms and instrumental parameters. Being an essential cofactor of the mitochondrial respiratory chain used for production of adenosine triphosphate (ATP), it is not surprising that the highest concentration compared to other tissues is focused on myocardium mitochondria
[84].
A relative tissue CoQ
10 deficiency could then play an etiopathogenic role in the development and progression of HF: some evidence suggests that the depletion of CoQ
10 is proportional to the reduction of CoQ
10 myocardial tissue concentrations and to the severity of the disease developed
[85][86][87][85,86,87]. In fact, the lowest levels of myocardial CoQ
10 have been observed in patients of New York Heart Association (NYHA) class IV compared to patients of NYHA class I
[88][89][88,89]. Of course, one of the most important studies in the field of nutraceuticals, the Q-SYMBIO multicentre, randomized placebo-controlled trial, was used to assess the impact of the daily intake of CoQ
10 on total mortality and not just on the surrogate endpoints. Patients with moderate or severe HF currently treated with the pharmacological gold standard treatments (420 patients) were randomized to a daily intake of 300 mg of CoQ
10 (
n = 202) or placebo (
n = 218). After two years, a significant reduction in Major Adverse Cardiac Events (MACE) rate (15% in the CoQ
10 group vs. 26% in the placebo group, HR: 0.50; 95%CI: 0.32 to 0.80;
p = 0.003), CV mortality (9% vs. 16%,
p = 0.026), all-cause mortality (10% vs. 18%,
p = 0.018), and incidence of hospital stays for HF (
p = 0.033) were registered in CoQ
10-treated patients vs. the placebo treated ones
[90]. This result was confirmed in a subsequent meta-analysis of 14 RCTs including 2149 patients. It has shown that administration of CoQ
10 reduces mortality (RR= 0.69; 95%CI: 0.50–0.95;
p = 0.02;
I2= 0%) and improves exercise capacity (SMD = 0.62; 95%CI: 0.02–0.30;
p = 0.04;
I2= 54%) compared to the placebo. However, no significant difference was observed in the endpoints of left ventricular ejection fraction (LVEF) between “active group” and placebo (SMD = 0.62; 95% CI: 0.02–1.12;
p = 0.04;
I2 = 75%)
[91]. The effect on LVEF could be more relevant in patients with preserved ejection fraction (EF)
[92] (net change: 4.8% vs. subjects with EF < 30%) and patients untreated with statins and/or angiotensin converting enzyme inhibitors (ACEi) (+6.7%) compared to the subgroup of patients treated with these drugs (+1.2%)
[93]. One of the possible explanations of the heterogeneity in results on EF may be the diversity of CoQ
10 supplemented through different pharmaceutical forms and dosages. In fact, plasma concentrations of this molecule are extremely variable in relation to pharmaceutical form and administered dosages but were reported in few RCTs
[94][95][96][94,95,96]. In addition, the diversity of HF grade of patients enrolled (NYHA I-II-III-IV), duration of treatments, and cotreatment with conventional therapies might be other factors that could explain the heterogeneity of results about EF
[97].
3.2. CoQ10 and Myocardial Infarction
HF could be related to different causes: one of the most frequent is ischemic damage. As highlighted before, treatment with CoQ
10 in HF could prevent myocardial cell damage and could restore tissue CoQ
10 deficiency, especially in myocardial tissue, with the final result being significant improvement in HF
[98][99][100][101][98,99,100,101]. The degree of deficiency of this molecule has also been found to correlate directly with the degree of impairment in left ventricular function
[102]. For these reasons, another possible indication of CoQ
10 supplementation is acute myocardial infarction (AMI). In fact, CoQ
10 is an ATP-sparing agent and regenerable antioxidant capable of protecting cell structures from oxidative damage during ischemia and reperfusion injury
[103][104][103,104].
AMI is typically characterized by complications such as left ventricular dysfunction related to necrosis and loss of functioning myocardium and consequently by pathological remodelling, which seem to be related to reperfusion-induced free radical damage, lipid peroxidation, and decreased energy production and thus the lack of CoQ
10 [105][106][107][108][105,106,107,108]. Cardiac remodelling may be defined as “a group of molecular, cellular, and interstitial alterations that manifest clinically as changes in size, mass, geometry, and function of the heart after injury”
[105]. These structural changes in ventricular remodelling in conjunction to tissue CoQ
10 deficiency may result in poor prognosis for its negative association with HF, which is the major cause of morbidity and mortality in patients with AMI
[109].
Oxidative stress may be important in the pathogenesis of remodelling which may begin via subcellular remodelling leading to HF
[110]. Therefore, any agent which can prevent remodelling in patients with AMI would be an important therapeutic aid for prevention of complications altering AMI
[111][112][111,112]. In a recent RCT of 55 patients with LVEF < 50% after AMI, the effects of CoQ
10 (120 mg/day) or placebo were studied for 24 weeks. The results revealed that wall thickness opposite the site of infarction decreased from 12.2 ± 2.0 mm to 10.0 ± 1.8 mm with CoQ
10 compared with 12.8 ± 2.2 mm to 13.3 ± 2.3 mm with the placebo (
p < 0.01). Left ventricular mass changed from 236 ± 72 g to 213 ± 61 g with CoQ
10 compared with 230 ± 77 g to 255 ± 86 g with placebo (
p < 0.01). In addition, treatment with CoQ
10 also prevented alteration of the sphericity index (from 1.61 ± 0.28 to 1.63 ± 0.30 with CoQ
10 compared with 1.61 ± 0.32 to 1.41 ± 0.31 with placebo (
p < 0.05)) and alteration of the wall thickening abnormality at the infarct site (from 9.4 ± 3.0 cm
2 to 9.1 ± 2.8 cm
2 compared with 10.1 ± 3.1 to 13.7 ± 4.2 cm
2 with placebo (
p < 0.05)). Finally, end diastolic and systolic volumes and serum ACE also showed significant reduction with CoQ
10 compared to the control group
[107]. The findings suggest that CoQ
10 administered early after AMI may be protective against left ventricular remodelling in patients with persistent left ventricular dysfunction. However, long-term RCTs are needed to confirm preliminary data.
3.3. CoQ10 and Atrial Fibrillation
Atrial fibrillation (AF) is considered a frequent atrial arrhythmia in patients diagnosed with HF or ischemic heart disease, and its prevalence has been growing worldwide in the last years. It is associated with an increase in morbidity and mortality
[113][114][115][113,114,115]. As underlined for HF, CoQ
10 plays an important role in the production of ATP and its bioenergetic function associated to with antioxidant and scavenge ROS function which is essential for proper heart functioning
[116][117][116,117]. A meta-analysis of eight RCTs found that patients treated with CoQ
10 were significantly less likely to develop ventricular arrhythmias (OR (95% CI) 0.05 (0.01–0.31)) and to require inotropic drugs after surgery (OR 95% CI 0.47 (0.27–0.81)). Twelve patients (22.2%) in the control group and three patients (6.3%) in the CoQ
10 group had episodes of AF after 12 months of treatment (
p = 0.02).
[118] Similar results were obtained by other authors, concluding that CoQ
10 as adjuvant treatment in patients with HF may attenuate the incidence of AF. The exact mechanisms of the effect are still unclear, even if one of the possible explanations could be attributed to the reduction of serum levels of malondialdehyde (MDA)
[119].
3.4. CoQ10 and Nonischemic Cardiomyopathies
Cardiomyopathies are a number of debilitating conditions responsible for poor quality of life and high risk of mortality. Both in vitro and animal studies suggest a link between cardiomyopathies and oxidative stress
[120]. CoQ
10 deficiency appears to be frequent in people with dilated cardiomyopathy, and its supplementation may be able to restore plasmatic and myocardial levels
[121]. However, new studies are needed to confirm this evidence.
In children with dilated cardiomyopathy, CoQ
10 may improve the cardiothoracic ratio and shorten ventricular depolarization and NYHA class
[122]. In a prospective RCT (duration 6 months) in children with dilated cardiomyopathy, the administration of CoQ
10 resulted in a lower mean score for the index of cardiac failure (
p < 0.024 compared to placebo) and in improvement of diastolic function (
p < 0.011 compared to placebo)
[123]. In subjects with hypertrophic cardiomyopathy treated with an average of 200 mg/day of CoQ
10, a significant improvement in symptoms of fatigue and dyspnoea with no side effects was noted. In addition, the mean interventricular septal thickness (from 1.51 ± 0.17 cm to 1.14 ± 0.13 cm, a 24% reduction,
p < 0.002) and mean posterior wall thickness improved significantly (from 1.37 ± 0.13 cm to 1.01 ± 0.15 cm, a 26% reduction,
p < 0.005)
[124]. There is also a significant improvement in quality of life (on a 6-min walk test) and NYHA class (≥1)
[125].
In the last years, many studies have focused on the role of CoQ
10 in iatrogenic cardiomiopathies induced by some drugs like anthracycline antibiotics used in the chemotherapy of hematological cancers as leukemias and lymphomas and in solid malignancies such as carcinomas and sarcomas
[126]. Doxorubicin is used for the treatment of early-stage breast cancer, and it is known to improve overall survival. However, side effects such as cardiomyopathy and HF can occur in some patients, probably also for a raised ROS generation. Today, there is data indicating that CoQ
10 did not have any influence on doxorubicin cell toxicity, thus making further studies urgent
[127]. Nevertheless, the administration of CoQ
10 and L-carnitine in combination showed protection against oxidative stress by reducing levels of malondialdehyde and nitric oxide if started within 5 days before doxorubicin use. In addition, it also improved heart functions and decreased IL-1 and TNF-α Troponin-l and Troponin-T levels
[128].
3.5. CoQ10 and Ischemic Stroke
In the pathophysiology of ischemic stroke, some factors such as inflammation, excitotoxicity, and oxidative stress were demonstrated to play a pivotal role
[129][130][129,130]. A recent study demonstrated the decrement of CoQ
10 in the acute phase of ischemic stroke and also the significant negative correlation between serum CoQ
10 levels and the scores of the NIHSS and MRS (respectively National Institutes of Health Stroke Scale and Modified Ranking Scale)
[131]. Ischemia/Reperfusion (I/R) injury may induce oxidative stress and low levels of protective antioxidants such as CoQ
10 in the brain. In particular, it seems that a decrease of CoQ
10 induced by I/R overcomes the aging process
[132]. In vivo studies (with symptomatic vasospasm model) have reported that pretreatment with CoQ
10 reduces the incidence of ischemic lesions and can alleviate the pathological outcomes following a stroke incidence
[133].
In the last years, the relation between CoQ
10 and inflammation and oxidative stress has been reported in cell and animal models. Glial fibrillary acidic protein (GFAP), MDA, and superoxide dismutase (SOD) activity are important biomarkers in oxidative stress and neuroinflammatory processes after stroke, and they can predict functional outcomes
[134][135][136][134,135,136]. In a short RCT, 60 patients with acute ischemic stroke were randomly assigned to a placebo or CoQ
10-supplemented group (300 mg/day) for 4 weeks. At the end of treatment, CoQ
10 supplementation improved NIHSS and MMSE scores significantly (
p = 0.05,
p = 0.03 respectively) even if there were no significant differences in MRS score, SOD, MDA, and GFAP levels between the two groups. These results could be partially explained by the low dose and short duration of supplementation
[137].