Bartonella henselae (B. henselae) is a gram-negative bacterium that causes cat scratch disease, bacteremia, and endocarditis, as well as other clinical presentations. B. henselae has been shown to form a biofilm in vitro that likely plays a role in the establishment and persistence of the bacterium in the host.
- Bartonella henselae
- cat flea
- sRNA
- biofilm formation
- gene regulation
1. Introduction
Since the first report of microbial biofilms nearly 40 years ago, two decades passed before interest began to grow in studies that examined the clinical significance of biofilm formation [1]. Studies that elucidate the complexity and dynamics of bacterial biofilms have continued to grow in recent years. As a result, increased data has become available establishing the intricate relationship between gene regulation, biofilm formation, and disease progression.
The genus Bartonella consists of numerous species, some of which are known to cause Trench fever, Carrion’s disease, and cat scratch disease (CSD) [2]. Trench fever, originally described more than 100 years ago as infecting nearly one million troops during World War I, is caused by B. quintana [3]. Evidence of Carrion’s disease can be traced back to pre-Inca cultures, but the illness was not attributed to infection with B. bacilliformis until the early 1900s [4]. CSD caused by B. henselae remains one of the most common infections caused by bacteria in the genus Bartonella. The Centers for Disease Control and Prevention (CDC) estimates more than 12,500 diagnosed cases of CSD annually in the US, although the disease is prevalent worldwide [5][6][7][8][5,6,7,8]. Recently, Bartonella species have been isolated from a wide array of species ranging from terrestrial animals to sea inhabitants, demonstrating the ability of Bartonella to adapt and survive in a diverse range of hosts [9][10][11][9,10,11].
Amongst the almost 50 defined or proposed Bartonella species, B. henselae is a gram-negative, intracellular zoonotic bacterium that infects both cats and humans [12]. Cats, the natural reservoir of B. henselae, generally do not show symptoms of infection. In several case reports, however, B. henselae has been isolated in cats with a variety of clinical symptoms including endocarditis, seizure disorders, ocular disease, and hyperglobulinaemia [13]. B. henselae infection occurs in humans when the bacterium is accidently transmitted through the scratch or bite of a cat, but other modes of transmission such as red ant bites have been reported [14]. Flea infestation on domestic animal reservoirs such as cats and dogs are of rising concern, as resistance to flea control insecticides is increasing [15].
B. henselae is able to adhere to host cells and form a biofilm (Figure 1) [16][17][18][16,17,18]. The ability of B. henselae or any microbe to form a biofilm has been linked to chronic diseases [19][20][19,20]. Upon diagnosis with a systemic B. henselae infection such as endocarditis, patients may be treated with ciprofloxacin or azithromycin depending on the severity of symptoms [21]. Treatment failure in patients diagnosed with B. henselae endocarditis has been largely attributed to the ability of B. henselae to form a biofilm and resist antibiotics. Recent in vitro data suggests drug combination treatments are more effective in eliminating B. henselae chronic infection, compared to current single drug treatments [22]. Despite the continued use of antibiotics, systemic cases of B. henselae infection remain difficult to treat and often require more invasive treatment courses [23]. Biofilm-associated antibiotic resistance or tolerance is a major mechanism used by pathogenic bacteria located within the extracellular matrix or extracellular polymeric substance (EPS). This EPS matrix has been shown to increase antibiotic resistance or tolerance by several mechanisms including inhibiting antibiotic penetration, secreting enzymes to degrade antibiotics, and activating signaling pathways for adaptation and survival [24]. Biofilm regulation in B. henselae consists of a complex gene regulatory system that allows the bacteria to survive in different phases of the lifecycle, resist antibiotic treatment, and persist in the human host [19][25][19,25]. The ineffectiveness of current antibiotic treatment for biofilm associated infections warrants further investigation of the mechanism by which B. henselae regulates biofilm-associated genes.
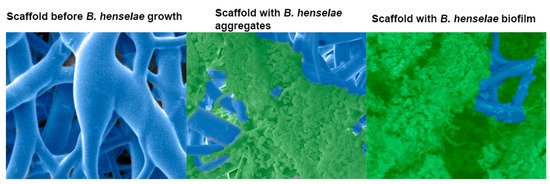
Figure 1.
Scanning electron micrograph of a 48 h
Bartonella henselae
(
B. henselae
) biofilm growing on a 3-dimensional nanofibrous scaffold. Left, scaffold before bacterial growth. Middle, bacterial growth, adhesion, and aggregation around the scaffold branches. Right,
B. henselae
biofilm covering the scaffold and eclipsing the bacterial cells. Biofilm was preserved by the addition of the cationic dye, Alcian blue.
Given the history of the Bartonella genus, the increased prevalence of Bartonella in a variety of species, and the poor treatment efficacy of systemic B. henselae infection, it is necessary to determine how B. henselae survives and persists, specifically through the formation of biofilms. Understanding such mechanism(s) will aid in the development of more effective treatments for B. henselae infection.
2. Clinical Importance
Three different Bartonella species—B. bacilliformis, B. quintana, and B. henselae—are the species most commonly associated with acute or chronic infections in humans [26]. In general, the severity of clinical outcomes correlates with the patient’s immune status; therefore, the more severe cases typically occur in immunocompromised individuals [27]. B. henselae is known to show several clinical manifestations, such as cat scratch disease (CSD), a condition characterized by lymphadenopathy and mostly reported in children [28][29][28,29], chronic lymphadenopathy [28][30][28,30], fever with persistent bacteremia [31], bacillary angiomatosis [32], neurological conditions [33], peliosis hepatitis [34], and life-threatening infective endocarditis, which is usually reported as blood-culture-negative endocarditis [31][35][36][31,35,36].
Fleas are competent vectors for numerous microbial pathogens. Ctenocephalides felis (C. felis), known as cat fleas, are an opportunistic blood feeder and the arthropod vector for B. henselae; however, other vectors such as ticks have been proposed [37][38][39][40][41][42][37,38,39,40,41,42]. Cats are reported to be the predominant host for B. henselae, but B. henselae has been isolated from a variety of hosts [43][44][45][46][43,44,45,46]. Most cats are asymptomatic when infected, but the exceptions usually develop a fever and local inflammation at the site of inoculum [46][47][48][46,47,48].
Bartonella infections begin with the inoculation of the bacteria, which is usually associated with the feeding of the arthropod vector on an infected cat. Bacterial load from the flea gut is excreted in the flea fecal matter and subsequently onto the cat [49]. Human infections occur through a cat scratch inoculating the host with bacteria from the flea fecal matter.
In the life cycle of B. henselae, biofilms are implicated in both the flea and the mammalian hosts. A previous report from our laboratory showed scanning electron micrographs with bacteria in the gut and bacterial biofilm in the fecal matter of laboratory i-fected cat fleas [19]. The ability of Bartonella to form biofilms in vertebrate hosts has been reported in the literature [50][51][52][50,51,52]. A mouse model of B. tayolrii infection was shown to demonstrate persistent bacteremia, liver lesions, and eventually death [51]. The masses observed in the liver and kidney appeared embedded in an amorphous matrix, which can be defined as a biofilm, providing an experimental model to study human disease progression in an immunocompromised host. In Edouard et al. (2015) [50], a study with 106 patients provided evidence of endocarditis by B. quintana and B. henselae. The above studies provide evidence that Bartonella biofilm communities are indeed an integral part of the vegetative mass associated with infective endocarditis [50][51][52][50,51,52]. B. henselae is a fastidious bacterium with particular nutritional requirements; hence, it is challenging to isolate and culture the bacterium from clinical samples [53]. Laboratory diagnosis is usually accomplished by one or more of the following diagnostic techniques: PCR, serology, isolation with extended incubation periods, or histopathology [54][55][56][57][54,55,56,57].
Bartonella species have a noteworthy ability to evade the host immune system and resist antimicrobial agents. While some isolates are susceptible to minocycline and macrolide antibiotics such as erythromycin, clarithromycin, azithromycin, and fluoroquinolone compounds with relatively low minimal inhibitory concentrations (MICs) [58][59][60][58,59,60], clinical experience has shown that Bartonella infection treatment failures are a major concern, as most of these antimicrobial classes exhibit only bacteriostatic properties [60][61][62][60,61,62]. It is expected that growth in biofilms allows Bartonella species to persist in the face of stress including antimicrobial treatment and the host immune response. Multiple studies and guidelines support 2 to 6 weeks of treatment for endocarditis using at least two antibiotics, one of which is an aminoglycoside [58][63][64][65][58,63,64,65]. Considering the clinical manifestations and antibiotic resistance of B. henselae, understanding the mechanisms by which B. henselae initiates biofilm formation is critical to comprehend how it causes chronic disease in humans.
3. Biofilm Formation, Composition, and Life Cycle
Bacteria grow as free-floating planktonic cells or as coordinated aggregates embedded in a matrix, referred to as a biofilm [66]. Biofilms can be single or multispecies communities, can thrive on most surfaces, and may be surface associated (agar, contact lens) or submerged under a static or shear flow condition (such as those formed in an artificial cardiac valve or indwelling catheter) [67][68][67,68]. Because of the diversity of biofilm surfaces, the well-organized structures of the colonies, and a characteristic anti-microbial resistance or tolerance, biofilms have received significant attention and are currently investigated for their role in infectious diseases [20][69][20,69]. Adhesion or aggregation is the first step of biofilm formation, virulence, and host cell interactions in most bacteria [70]. Outer membrane adhesins facilitate bacterial adhesion to a biotic or abiotic substrate and self-aggregation. Bacteria first adhere, then aggregate to allow the chemical signaling and quorum sensing communication required for the aggregates to secrete the proteins, polysaccharides, and extracellular DNA (eDNA) required for the assembly of the biofilm [71]. The B. henselae biofilm has been shown to contain proteins, polysaccharides, and eDNA, and both DNase and proteinase K have been shown to result in biofilm destruction [16].
The growth of B. henselae as a biofilm was first reported by Kyme et al. [72] as an auto-aggregative phase variation later linked to the expression of a surface adhesin called BadA. In the Bartonella genus, the roles of BadA and Vomps proteins are well documented for the adhesion steps in B. henselae and B. quintana, respectively. BadA is a trimeric auto transporter (TAA), and the role of TAAs have been significantly documented in other gram-negative bacteria [73][74][75][73,74,75]. A genetic deletion of badA in different strains of B. henselae led to failure to adhere efficiently and form a biofilm [12][16][76][12,16,76].
In humans, it has been speculated that B. henselae infects erythrocytes and may persist in these cells [77]. Evidence also supports persistence in endothelial progenitor cells, which presents the possibility for host immune system evasion [78][79][80][78,79,80]. B. henselae is speculated to form biofilms in the gut of the cat flea, which helps the bacteria persist and replicate in the gut [81]. The bacterial load is excreted in the fecal matter, where it forms a biofilm that protects the bacteria, which persists about 10–12 days in the flea fecal matter before human inoculation through the cat claw [19][49][19,49]. We propose that the biofilm represents an additional niche that provides the platform for seeding planktonic cells into the bloodstream, causing host immune reactions, disease conditions, and persistence in the face of antimicrobial treatments.
