Ventricular tachycardia is a type of arrhythmia (heart rhythm disorder) characterized by fast heart rate (exceeding 100 beats per minute), originating from abnormal electrical impulse localized in heart ventricles. The electrophysiology-guided noninvasive cardiac radioablation, also known as STAR (stereotactic arrhythmia radioablation), is an emerging treatment method of non-invasive treatment for ventricular tachycardia persistent after conventional methods of ablation.
- ablation
- noninvasive
- radiosurgery
- stereotactic body radiation therapy
- substrate ablation
- ventricular tachycardia
1. What is STAR?
Ventricular arrhythmias, including ventricular tachycardias (VT), are a major cause of sudden cardiac death (SCD) [1], which globally contributes to 4.25 million deaths every year [2].
The guidelines-driven management of VTs consists of antiarrhythmic drugs (AADs), placement of implantable cardiac defibrillators (ICDs), and the ablation of the arrhythmogenic substrate [3][4][5][3,4,5]. Despite the significant clinical improvement, results of conventional radiofrequency ablation (RFA) strategy can be limited especially in case of challenging anatomy and subepicardial substrate location. Post-RFA recurrence rate ranges from 12–17% at 1 year follow-up [6], and, although rarely directly associated with procedural complications (0.6%), RFA is associated with up to ~5% short-term mortality in ischemic VT cases [7].
A need to deliver better care for patients makes VT ablations one of the most dynamically growing areas in the field of cardiac electrophysiology (EP) [8]. The increasing number of patients with refractory VT leveraged by the implementation of new technologies has already improved clinical results [9]. Specifically, stereotactic arrhythmia radioablation (STAR) aims to reduce the burden of arrhythmia [10][11][12][10,11,12] through a combination of 3D electrophysiological mapping (EAM), noninvasive myocardial scar imaging (computed tomography (CT), positron emission tomography (PET), cardiac magnetic resonance (cMR) [13][14][13,14]), and noninvasive delivery of ablative radiation doses [15], as presented in Figure 1. STAR faces everyday clinical challenges associated with the extension of indications for VT ablations, including advanced ischemic and nonischemic cardiomyopathies [16][17][18][16,17,18]. As a routine step of the STAR methodology, cardiac imaging showed that a substantial number of VT patients have fibrotic scars located intramurally and epicardially, thus not being accessible with endocardial ablation approaches [19]. New insights confirm the necessity to co-register anatomical and functional data reassuring integration of imaging techniques with electrophysiological studies.
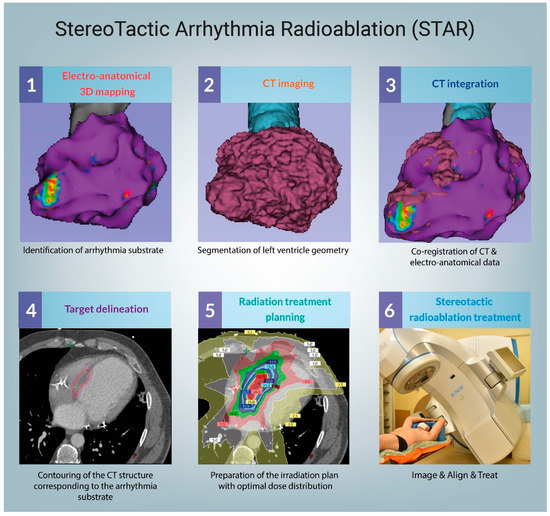
Figure 1. Procedural workflow. CT–computed tomography.
2. Unique challenges
For the majority of radiotherapeutic history, the collaboration with cardiologists mainly focused on the subject of damage control of radiation sequelae, including late (i.e., coronary disease) and early (i.e., ICD damage, thrombosis) toxicity. The introduction of curative radiosurgery into a strictly cardiological field caused a major paradigm shift and forced the development of many new and innovative strategies, including the necessity to integrate the EP maps with the data available in the radiotherapy treatment planning systems, as well as develop strategies for the delivery of high, curative doses to the heart.
3. Current status
The future of STAR is still undetermined. Despite many promising results, the methodology of this emerging treatment method is significantly different between studies, including a significant lack of agreement in terms of the treatment volumes. Despite the favorable early toxicity profile, studies have shown clinically relevant late toxicities at significantly later timepoints than the follow-up available in the majority of the reports. Nevertheless, considering a significant amount of promising data, we believe that the development of optimal STAR workflow is possible and could help to address a specific and clinically important problem of the post-ablation VT recurrences.
The future of STAR is still undetermined. Despite many promising results, the methodology of this emerging treatment method is significantly different between studies, including a significant lack of agreement in terms of the treatment volumes. Despite the favorable early toxicity profile, studies have shown clinically relevant late toxicities at significantly later timepoints than the follow-up available in the majority of the reports. Nevertheless, considering a significant amount of promising data, we believe that the development of optimal STAR workflow is possible and could help to address a specific and clinically important problem of the post-ablation VT recurrences.
