Hand exoskeletons are still an active research field due to challenges that engineers face and are trying to solve. Each hand exoskeleton has certain requirements to fulfil to achieve their aims.
- hand exoskeletons
- rehabilitation
- active assistive devices
- robotic orthosis
- hand exoskeleton requirements
1. Basic Requirements for Hand Exoskeletons
What is a hand exoskeleton? Hand exoskeletons are wearable robotic devices that have the aim of assisting the fingers, of the human hand, to complete its range of motion (ROM), amplify power, rehabilitating impaired hands or in today’s society gives haptic feedback for virtual or teleoperation applications. The word “exoskeleton” actually refers to the hard-outer shell of certain animals that serves the purpose of protecting and supporting their body. We as humans have endoskeletons that are located inside the body [1]. Therefore, the robotic devices up to this stage were designed to be fitted on the dorsal, palmar, or lateral side of the hand/fingers.
Certain requirements need to be kept in mind upon designing an exoskeleton, whether it is for assistive, rehabilitative, augmentative, or haptic purposes (
1). Each class of exoskeleton has over the years defined certain requirements to suit their purpose.
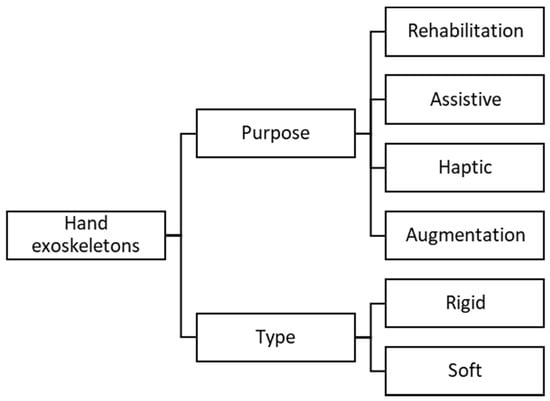
Figure 51. This diagram is an outline of the hierarchy structure identified for the various types of hand exoskeletons, in different fields, as well as the type of existing hand exoskeleton technologies.
There are mainly two types of hand exoskeletons developed over the years, which are classified as rigid and soft exoskeletons (Figure 51) or a combination of the two. Rigid exoskeletons are mechanisms where the force or torques are transmitted to the required joints through a mechanical structure. To ensure that the exoskeleton joints are aligned with the finger joints, ideally, the mechanical structure aligns with each joint (usually on the lateral side of the fingers) (Figure 62a). This can be considered to be the most intuitive design method, but it restricts the size due to the space between the fingers, and custom fits are usually required. This method is also known as the matched axis design [32,33][2][3]. Many exoskeletons were designed to reduce the size and add more DOF for the hand, which led to the remote center of rotation design [34][4] (Figure 62b). This design is usually fitted on the dorsal side of the fingers and transmits the forces to the joints through the phalanges. The bar mechanisms include parallelogram mechanisms and circular-prismatic joints [35,36,37,38][5][6][7][8]. Another design created over the years is mechanisms using four-bar linkages or other mechanisms to actuate the joints. These mechanisms also attach to the phalanges after the required joint and are usually a bit larger than the remote center of rotation mechanisms. These are also known as redundant linkages [39,40,41,42][9][10][11][12] (Figure 62c). A mechanism known as the base to distal topology (Figure 62d) has also been explored. This mechanism has only one contact point with the finger, usually the distal phalange or proximal phalange, and is coupled together through linkages connected in series. This design has the advantage of actuating several joints at the same time with less active control over each joint. This design is commonly referred to as the base-to-distal mechanism [43,44][13][14] and is also mostly found at assistive-related exoskeletons.
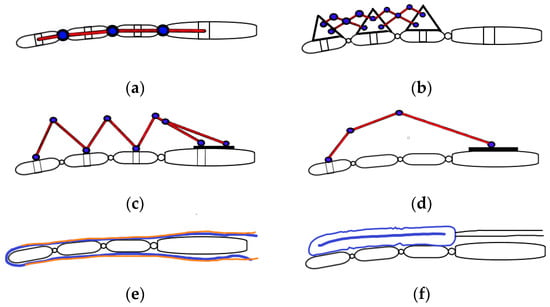
Figure 6. Different existing hand exoskeleton designs. Various designs exist for each category, although the fundamental design idea is illustrated. (a) Matched-axis design. (b) Remote center of rotation (RCR) design. (c) Redundant mechanism (four-bar link mechanisms). (d) Base-to-distal design. (e) Tendon driven glove (complaint). The tendon/cables are illustrated in orange, and the blue represents a glove or flexible base structure. (f) Jointless structure. Can either be actuated from compressed air (pneumatics) or hydraulic fluids.
One of the predicted future trend exoskeleton designs is known as compliant systems or “soft” hand exoskeletons. These systems are designed in the form of a glove with flexible materials or elastic structures to transmit the forces to the joints of the fingers. Many avenues have been and are still being explored such as artificial muscles [45][15], tendon-driven devices (Figure 62e) [46,47,48[16][17][18][19],49], and pneumatically actuated jointless structures (Figure 62f) [50,51,52,53,54][20][21][22][23][24]. These devices can be lightweight and compact at the hand but usually require cables or air tubes situated remotely to the actuating unit. Special design care must be taken, especially for rehabilitation and assistance purposes, because there is no rigid structure to guide the finger and transmit the required torques to the joint. The flexible structure usually relies on the rigid skeleton bone structure to guide the fingers in flexion and extension or abduction and adduction motions. Therefore, any misaligned forces may cause secondary injuries over time or cause discomfort to the users.
There was a study done in 2018 by [55][25] to determine the design requirements for hand assistive powered exoskeletons. This study interviewed clinicians and patients with hand impairments to determine the most suitable requirements for an assistive hand exoskeleton. The clinicians emphasized the importance of obtaining opposition with the thumb and how it will increase the patient’s ability to become more independent. The patients indicated the tasks that they would like the hand exoskeletons to assist them with such as hold utensils to eat, write, carry a bag, drink something, use a computer, etc. (many referring to pinch, power, and hook grip formations); there are many tasks identified through the interviews, which all are basic and everyday tasks. Many have indicated that the hand exoskeleton must at least be strong enough to hold a 750 mL can or mug and operate the device continuously for at least 6 h. Patients also indicated that a weight of 200 g on the hand will be manageable, and an open palm would be preferred. Figure 73 indicates the average weight of each exoskeleton design type and can be compared to the preferred weight mentioned above.
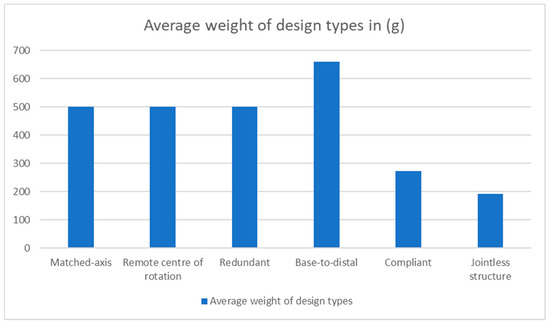
Figure 73. This graph shows the average weight of each exoskeleton design type by only considering the weight of the exoskeleton on the hand.
This is a very useful paper to gather firsthand information on the possible end-user and determining the desired requirements to fulfill.
2. General Requirements
2.1.Safety
Safety is the most crucial requirement for all hand exoskeletons and exoskeletons in general, especially for active systems. These systems can cause harm to the user; therefore, caution must be taken when designing such a mechanism. The mechanical actuation and control system must ensure that the natural movements of the fingers are executed and do not induce secondary injuries to the users, especially for rehabilitation and assistive mechanisms. Mechanical stops, force limits, or limited rotation can be used for such systems to ensure that there will be no excessive range of motion movements. Designs incorporating such safety mechanisms are [26][2][3][5][6][7][9][10][11][12][14][15][20][21][23][24][27][28][29][30][31][32][33][34][35][36][37][38][39][40][41].
2.2. Comfort
Hand exoskeleton must be comfortable for the user, especially for rehabilitation, assistive, and haptic devices. These devices are made to be worn for long periods. The hand exoskeleton is required to have an ergonomic structure and fit the hand to perform tasks. Soft exoskeletons are generally classified as more comfortable than rigid systems but can introduce discomfort when in operation if the forces are not transmitted correctly.
The interaction between the hand and the device is the most important aspect for comfort. Devices that utilize the construction of remote center of rotation, redundant, and base-to-distal generally have the interaction of the device with the respective phalanges of the fingers on the dorsal (backside) of the finger. Foam pads and Velcro or silicone straps are the most popular method for securing these devices to the fingers [26][5][8][9][10][11][13][29][30][32][34][42][43]. The foam acts as a damper and increases the comfort for the user. Some redundant devices are attached to a material glove such as in [12][35], while other base-to-distal devices such as [14][27] have custom-made thimbles to comfortably fit the user’s fingertip. Compliant and jointless structures mostly use gloves as the interaction point between the fingers and the tendons or artificial muscles. This is one main reason for the higher comfort in “soft” exoskeletons due to the lack of “rigid” structures.
Most devices are in the prototyping phase, and generally, the “rigid” structures are constructed from polylactic acid (PLA) polymer, which is biodegradable and is generally used in 3D printing. The minority devices that were released for clinical environments are constructed from aluminum metal for durability [5]. “Soft” exoskeletons are generally made from soft materials such as silicone to reduce weight and increase comfort for the users.
2.3. Affordability
Hand exoskeletons and exoskeletons in general tend to be very expensive. This is due to the technology and materials available as well as this being a relatively new area of research. The development of technology as the field progresses makes the devices more affordable in today’s society. Rapid prototyping such as 3D printing and software modeling enables devices to be made relatively efficient and cost-effective, but there is still a search for a design to accommodate all requirements with the best execution. The devices must be affordable to the patient and the clinicians if it is to be used in a clinical setting. Devices custom-designed for a patient are generally more expensive than a device that is transparent to various users. Low maintenance and ease of use is also generally a kind of mandatory requirement.
2.4. Adaptability
The devices are preferable to be designed for multiple end-users and to fit various hand sizes. This is especially necessary for augmentation, haptic, and rehabilitation devices due to various users that will use the device each with a different hand structure and size.
The hand exoskeletons reviewed in this paper have been designed for adult-size hands, and many can adjust to the varying sizes in this range (refer to
). Sandoval-Gonzalez et al. conducted an anthropometric study of the hand to obtain an average hand size from the combination of males and females from the ages of 16 to 70 [34], for hand exoskeleton design. This can be a good reference for future designs.
3 (along with
), indicates the distribution of the design topologies found in the literature.

The pie chart indicates the distribution of the exoskeleton design type according to the literature.
Captures the interaction between the human and the device as well as indicating the adaptability of the reviewed devices.
| Design Type | Wearability | Adaptability | Devices | |
|---|---|---|---|---|
| Matched-axis | The exoskeleton generally has concave-shaped clips inlined with foam, which attaches to the finger phalange through Velcro or silicone straps. These clips are designed to fit the finger ergonomics, hence the concave shape. | To adjust to different finger sizes, these are generally designed to have the proximal and middle phalange clips to slide in or out to align the joint axis to the exoskeleton axis. These are usually passive prismatic joints. | [32,33] | [2][3] |
| Remote centre of rotation, redundant and Base-to-distal | These devices are similar in the way they attached to the fingers. Usually, the section attached to the phalange has a concave shape to the phalange and attaches to the finger through a Velcro or silicone strap. Some devices have custom rigid rings the phalanges interact with, and others have thimbles for the distal phalanges. Some exoskeletons have their interaction points with the finger attached to a glove for a more comfortable and convenient fitting. | These are designed to be adjustable to various hand sizes by simply adjusting the phalange clips to the center of the phalanges. The only drawback to the device using a glove will be that a different size glove has to be used to for different hand sizes. | [12,35,37,38,39,40, | |
| 24 | ||||
| ] | [ | 50 | ] |
3. Specific Requirements
As mentioned previously, there are multiple areas where the use of a hand exoskeletons can be beneficial, but the main focus is placed on rehabilitation and assistive devices.
3.1. Rehabilitation
These exoskeletons are designed to rehabilitate patients with disabilities and assist therapists to treat these patients. These devices are designed with the focus of executing repetitive actions and motions. This includes the flexion and extension of the fingers to mimic the activities of daily living or to execute continuous passive motion (CPM) for patients after surgery to prevent stiffness of the joints and tendons. These devices generally do not have to be portable due to it being used in a clinical or medical environment. It usually contains sensors for feedback to the therapists to track the patient’s progress and to determine the severity of the impairment. These devices are mostly active devices with a relatively high output force projected to the patient’s fingers depending on the training or rehabilitation given by the therapist as well as to overcome stiff joints if the patient suffers from that (
).
These requirements are only the identified general important factors and may differ for certain applications.
| Type | Requirements | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Rehabilitation | Safety High output force Transparent Active or passive actuation Easy wearable Finger tracking/sensor feedback Comfortable Combined or independent finger control Backdrivable |
|||||||||||
| Assistive | Safety Easy wearable Transparent Active actuation Portable Lightweight Comfortable Combined or independent finger control Interaction with objects Intention detection is preferable Backdrivable | 41 | ,42,43,73,74] | [26][5][7][8][9][10][11][12][ | 44,56,57, | 13][14][27][ | 58,60,61, | 28][29][31][ | 63, | 32][34] | 64, | [35][38][40][43][44][45] |
| Affordable | 67 | ,69,72, | Compliant | Most of the compliant devices use gloves to anchor the actuating mechanisms to the appropriate joints or phalanges. Others make use of a custom silicone-based sleeve that enables custom interactions with the finger. | Gloves are adjustable to only a certain hand size before a different glove is required. This is a common issue with compliant devices. Custom silicone-based designs can adjust to a greater number of hand sizes. | |||||||
| Haptic | Safety Transparent Easy wearable Portable Lightweight Independent finger movement Finger tracking Comfortable Affordable | [ | 46, | ] | 47,48, | [ | 49,66, | 17][18][19] | 75,76,77,78] | [16[37][46][47][48][49] | ||
| Jointless structures | Gloves are the most popular method for attaching jointless structures or artificial muscles. Velcro is used to attach the actuating device to the glove. | |||||||||||
| Augmentation | Safety | This method of actuation cannot generally adjust to various hand sizes and are usually custom made for the end-user. | Easy wearable Comfortable Portable Transparent High output force | [45,50,51,52,54,79] | [15][20][21][22][ |
3.2. Assistive
These types of exoskeletons are designed with the main purpose to assist the user to accomplish activities of daily living (ADL), such as making coffee, eating, holding a bag, etc. (refer to the interview conducted by [25] for more information). This type of hand exoskeleton is preferred to be portable, lightweight, easily wearable, and transparent, as the patient will operate this device in their home setting or a public area. The device is active and must allow a patient to interact with their environment actively. Sensory feedback information is not a requirement, but some devices have been designed to serve both rehabilitation and assistive purposes, which contains sensors for progress and finger tracking as well as force sensing for manipulating objects (
).
3.3. Haptic
These types of exoskeletons are developed for healthy individuals with the main purpose to give haptic feedback for virtual and teleoperation applications. It allows the individual to interact with objects in the virtual environment and feel the objects through the exoskeleton. These devices are usually underactuated and contain sensors for finger tracking. The amount of output force to control the fingers is not as crucial as in other applications. Due to the device being worn by healthy individuals, adjustability is recommended for an affordable device, and individual finger movement is required (
).
3.4. Augmentation
These types of hand exoskeletons serve the purpose to amplify the user’s power. This is made for healthy individuals and portability is favorable. These types of exoskeletons are generally produced for military purposes, but it is also used in the space program to help astronauts flex and extend their fingers through the stiff spacesuit [51][52]. High power output is required for these types of hand exoskeletons with maximum safety precautions implemented, as these devices can cause serious harm to the user if malfunctioned (
).
References
- Cempini, M.; Cortese, M.; Vitiello, N. A Powered finger–thumb wearable hand exoskeleton with self-aligning joint axes. IEEE/ASME Trans. Mechatron. 2014, 20, 705–716.
- Chiri, A.; Vitiello, N.; Giovacchini, F.; Roccella, S.; Vecchi, F.; Carrozza, M.C. Mechatronic Design and Characterization of the Index Finger Module of a Hand Exoskeleton for Post-Stroke Rehabilitation. IEEE/ASME Trans. Mechatron. 2011, 17, 884–894.
- Cempini, M.; De Rossi, S.M.M.; Lenzi, T.; Cortese, M.; Giovacchini, F.; Vitiello, N.; Carrozza, M.C. Kinematics and design of a portable and wearable exoskeleton for hand rehabilitation. In Proceedings of the 2013 IEEE 13th International Conference on Rehabilitation Robotics (ICORR), Seattle, WA, USA, 24–26 June 2013; pp. 1–6.
- Battezzato, A. Kinetostatic analysis and design optimization of an n-finger underactuated hand exoskeleton. Mech. Mach. Theory 2015, 88, 86–104.
- Tong, K.; Ho, S.; Pang, P.; Hu, X.; Tam, W.; Fung, K.; Wei, X.; Chen, P.; Chen, M. An intention driven hand functions task training robotic system. In Proceedings of the 2010 Annual International Conference of the IEEE Engineering in Medicine and Biology, Buenos Aires, Argentina, 31 August–4 September 2010; pp. 3406–3409.
- Ockenfeld, C.; Tong, R.K.Y.; Susanto, E.A.; Ho, S.-K.; Hu, X.-L. Fine finger motor skill training with exoskeleton robotic hand in chronic stroke: Stroke rehabilitation. In Proceedings of the 2013 IEEE 13th International Conference on Rehabilitation Robotics (ICORR), Seattle, WA, USA, 24–26 June 2013; pp. 1–4.
- Cui, L.; Phan, A.; Allison, G. Design and fabrication of a three dimensional printable non-assembly articulated hand exoskeleton for rehabilitation. In Proceedings of the 2015 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Milan, Italy, 25–29 August 2015; pp. 4627–4630.
- Wang, D.; Meng, Q.; Meng, Q.; Li, X.; Yu, H. Design and Development of a Portable Exoskeleton for Hand Rehabilitation. IEEE Trans. Neural Syst. Rehabil. Eng. 2018, 26, 2376–2386.
- Tang, T.; Zhang, D.; Xie, T.; Zhu, X. An exoskeleton system for hand rehabilitation driven by shape memory alloy. In Proceedings of the 2013 IEEE International Conference on Robotics and Biomimetics (ROBIO), Shenzhen, China, 12–14 December 2013; pp. 756–761.
- Lambercy, O.; Schröder, D.; Zwicker, S.; Gassert, R. Design of a thumb exoskeleton for hand rehabilitation. Presented at the International Convention on Rehabilitation Engineering and Assistive Technology (i-CREATe), Zurich, Switzerland, 13 September 2013; Available online: (accessed on 4 June 2020).
- Conti, R.; Meli, E.; Ridolfi, A. A novel kinematic architecture for portable hand exoskeletons. Mechatronics 2016, 35, 192–207.
- Jo, I.; Bae, J. Design and control of a wearable and force-controllable hand exoskeleton system. Mechatronics 2017, 41, 90–101.
- Iqbal, J.; Khan, H.; Tsagarakis, N.G.; Caldwell, D.G. A novel exoskeleton robotic system for hand rehabilitation—Conceptualization to prototyping. Biocybern. Biomed. Eng. 2014, 34, 79–89.
- Sarakoglou, I.; Brygo, A.; Mazzanti, D.; Hernandez, N.G.; Caldwell, D.G.; Tsagarakis, N.G. HEXOTRAC: A highly Un-der-Actuated Hand Exoskeleton for Finger Tracking and Force Feedback. Presented at the IEEE/RSJ International Conference on Intelligent Robots and Systems (IROS), Daejeon, Korea, 9–14 October 2016; Available online: (accessed on 5 June 2020).
- Tjahyono, A.P.; Aw, K.C.; Devaraj, H.; Surendra, W.; Haemmerle, E. A five-fingered hand exoskeleton driven by pneumatic artificial muscles with novel polypyrrole sensors. Ind. Robot Int. J. 2013, 40, 251–260.
- Yang, J.; Xie, H.; Shi, J. A novel motion-coupling design for a jointless tendon-driven finger exoskeleton for rehabilitation. Mech. Mach. Theory 2016, 99, 83–102.
- In, H.; Kang, B.B.; Sin, M.; Cho, K.-J. Exo-Glove: A Wearable Robot for the Hand with a Soft Tendon Routing System. IEEE Robot. Autom. Mag. 2015, 22, 97–105.
- Popov, D.; Gaponov, I.; Ryu, J.-H. Portable Exoskeleton Glove with Soft Structure for Hand Assistance in Activities of Daily Living. IEEE/ASME Trans. Mechatron. 2016, 22, 865–875.
- Kazeminasab, S.; Hadi, A.; Alipour, K.; Elahinia, M. Force and motion control of a tendon-driven hand exoskeleton actuated by shape memory alloys. Ind. Robot. Int. J. 2018, 45, 623–633.
- Polygerinos, P.; Wang, Z.; Galloway, K.C.; Wood, R.J.; Walsh, C.J. Soft robotic glove for combined assistance and at-home rehabilitation. Robot. Auton. Syst. 2015, 73, 135–143.
- Yap, H.K.; Lim, J.H.; Nasrallah, F.; Goh, J.C.H.; Yeow, R.C.H. A soft exoskeleton for hand assistive and rehabilitation application using pneumatic actuators with variable stiffness. Presented at the International Conference on Robotics and Automation, Seattle, WA, USA, 26–30 May 2015; Available online: (accessed on 2 June 2020).
- Yap, H.K.; Ang, B.W.K.; Lim, J.H.; Goh, J.C.H.; Yeow, C.-H. A fabric-regulated soft robotic glove with user intent detection using EMG and RFID for hand assistive application. In Proceedings of the 2016 IEEE International Conference on Robotics and Automation (ICRA), Stockholm, Sweden, 16–21 May 2016; pp. 3537–3542.
- Haghshenas-Jaryani, M.; Carrigan, W.; Nothnagle, C.; Wijesundara, M.B.J. Sensorized soft robotic glove for continuous passive motion therapy. In Proceedings of the 2016 6th IEEE International Conference on Biomedical Robotics and Biomechatronics (BioRob), Singapore, 26–29 June 2016; pp. 815–820.
- Al-Fahaam, H.; Davis, S.; Nefti-Meziani, S.; Theodoridis, T. Novel soft bending actuator-based power augmentation hand exoskeleton controlled by human intention. Intell. Serv. Robot. 2018, 11, 247–268.
- Boser, Q.A.; Dawson, M.R.; Schofield, J.S.; Dziwenko, G.Y.; Hebert, J.S. Defining the design requirements for an assistive powered hand exoskeleton: A pilot explorative interview study and case series. Prosthet. Orthot. Int. 2020.
- Schabowsky, C.N.; Godfrey, S.B.; Holley, R.J.; Lum, P.S. Development and pilot testing of HEXORR: Hand EXOskeleton Rehabilitation Robot. J. Neuroeng. Rehabil. 2010, 7, 36.
- Iqbal, J.; Tsagarakis, N.G.; Caldwell, D.G. A multi-DOF robotic exoskeleton interface for hand motion assistance. In Proceedings of the 2011 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Boston, MA, USA, 30 August–3 September 2011; Volume 2011, pp. 1575–1578.
- Li, J.; Zheng, R.; Zhang, Y.; Yao, J. iHandRehab: An interactive hand exoskeleton for active and passive rehabilitation. In Proceedings of the 2011 IEEE International Conference on Rehabilitation Robotics, Zurich, Switzerland, 29 June–1 July 2011; pp. 1–6.
- Rahman, A.; Al-Jumaily, A. Design and Development of a Hand Exoskeleton for Rehabilitation Following Stroke. Procedia Eng. 2012, 41, 1028–1034.
- Zhang, F.; Hua, L.; Fu, Y.; Chen, H.; Wang, S. Design and development of a hand exoskeleton for rehabilitation of hand injuries. Mech. Mach. Theory 2014, 73, 103–116.
- Heo, P.K.J. Power-Assistive Finger Exoskeleton with a Palmar Opening at the Fingerpad. IEEE Trans. Biomed. Eng. 2014, 61, 2688–2697.
- Agarwal, P.; Fox, J.; Yun, Y.; O’Malley, M.K.; Deshpande, A.D. An index finger exoskeleton with series elastic actuation for rehabilitation: Design, control and performance characterization. Int. J. Robot. Res. 2015, 34, 1–26.
- Bataller, A.; Cabrera, J.A.; Clavijo, M.; Castillo, J.J. Evolutionary synthesis of mechanisms applied to the design of an exoskeleton for finger rehabilitation. Mech. Mach. Theory 2016, 105, 31–43.
- Sandoval-Gonzalez, O.; Jacinto-Villegas, J.M.; Herrera-Aguilar, I.; Portillo-Rodiguez, O.; Tripicchio, P.; Hernandez-Ramos, M.; Flores-Cuautle, A.; Avizzano, C. Design and development of a hand exoskeleton robot for active and passive rehabilitation. Int. J. Adv. Robot. Syst. 2016, 13, 66.
- Ben Abdallah, I.; Bouteraa, Y.; Rekik, C. Design and development of 3d printed myoelectric robotic exoskeleton for hand rehabilitation. Int. J. Smart Sens. Intell. Syst. 2017, 10, 341–366.
- Bianchi, M.; Cempini, M.; Conti, R.; Meli, E.; Ridolfi, A.; Vitiello, N.; Allotta, B. Desing of a Series Elastic Transmission for hand exoskeletons. Mechatronics 2018, 51, 8–18.
- Randazzo, L.; Iturrate, I.; Perdikis, S.; Millan, J.D.R. Mano: A wearable hand exoskeleton for activities of daily living and neurorehabilitation. IEEE Robot. Autom. Lett. 2018, 3, 500–507.
- Jo, I.; Park, Y.; Lee, J.; Bae, J. A portable and spring-guided hand exoskeleton for exercising flexion/extension of the fingers. Mech. Mach. Theory 2019, 135, 176–191.
- Li, M.; He, B.; Liang, Z.; Zhao, C.G.; Chen, J.; Zhuo, Y.; Xu, G.; Xie, J.; Althoefer, K. An attention-controlled hand exoskeleton for the rehabilitation of finger extension and flexion using a rigid-soft combined mechanism . Front. Neurorobot 2019, 13, 1–13.
- Marconi, D.; Baldoni, A.; McKinney, Z.; Cempini, M.; Crea, S.; Vitiello, N. A novel hand exoskeleton with series elastic actuation for modulated torque transfer. Mechatronics 2019, 61, 69–82.
- Bützer, T.; Lambercy, O.; Arata, J.; Gassert, R. Fully wearable actuated soft exoskeleton for grasping assistance in everyday activities. Soft Robot. 2020, 1–16.
- Wang, S.; Li, J.; Zheng, R. Active and passive control algorithm for an exoskeleton with bowden cable transmission for hand rehabilitation. In Proceedings of the 2010 IEEE International Conference on Robotics and Biomimetics, Tianjin, China, 14–18 December 2010; pp. 75–79.
- Akgun, G.; Cetin, A.E.; Kaplanoglu, E. Exoskeleton design and adaptive compliance control for hand rehabilitation. Trans. Inst. Meas. Control. 2019, 42, 493–502.
- Li, J.; Wang, S.; Wang, J.; Zheng, R.; Zhang, Y.; Chen, Z. Development of a Hand Exoskeleton System for Index Finger Re-habilitation. Chin. J. Mech. Eng. 2012, 25, 223–232.
- Zhou, M.A.; Pinhas, B.T. RML Glove—An exoskeleton glove mechanism with haptics feedback. IEEE/ASME Trans. Mechatron. 2014, 20, 641–652.
- Mohamaddan, S.; Komeda, T. Wire-driven mechanism for finger rehabilitation device. In Proceedings of the 2010 IEEE International Conference on Mechatronics and Automation, Xi’an, China, 4–7 August 2010; pp. 1015–1018.
- In, H.; Cho, K.-J.; Kim, K.; Lee, B. Jointless structure and under-actuation mechanism for compact hand exoskeleton. In Proceedings of the 2011 IEEE International Conference on Rehabilitation Robotics, Zurich, Switzerland, 29 June–1 July 2011; pp. 1–6.
- Nilsson, M.; Ingvast, J.; Wikander, J.; Von Holst, H. The Soft Extra Muscle system for improving the grasping capability in neurological rehabilitation. In Proceedings of the 2012 IEEE-EMBS Conference on Biomedical Engineering and Sciences, Langkawi, Malaysia, 17–19 December 2012; pp. 412–417.
- Serbest, K.; Eldogan, O. Design, development and evaluation of a new hand exoskeleton for stroke rehabilitation at home. J. Polytech. 2020, 24, 305–314.
- Yap, H.K.; Lim, J.H.; Nasrallah, F.; Yeow, C.-H. Design and Preliminary Feasibility Study of a Soft Robotic Glove for Hand Function Assistance in Stroke Survivors. Front. Neurosci. 2017, 11, 547.
- Villoslada, A.; Rivera, C.; Escudero, N.; Martín, F.; Blanco, D.; Moreno, L. Hand exo-muscular system for assisting as-tronauts during extravehicular activities. Soft Robot. 2018, 6, 11–20.
- Shields, B.L.; Main, J.A.; Peterson, S.W.; Strauss, A.M. An anthropomorphic hand exoskeleton to prevent astronaut hand fatigue during extravehicular activities. IEEE Trans. Syst. Man Cybern. Part A Syst. Hum. 1997, 27, 668–673.
