Hyperuricemia is a risk factor for gout. It has been well observed that a large proportion of individuals with hyperuricemia have never had a gout flare(s), while some patients with gout can have a normuricemia. This raises a puzzle of the real role of serum uric acid (SUA) in the occurrence of gout flares. As the molecule of uric acid has its dual effects in vivo with antioxidant properties as well as being an inflammatory promoter, it has been placed in a delicate position in balancing metabolisms. Gout seems to be a multifactorial metabolic disease and its pathogenesis should not rely solely on hyperuricemia or monosodium urate (MSU) crystals.
- uric acid
- inflammation
- hyperuricemia
1. Introduction
[1]
[2]
[3]
[4]
[5]
[6]
[7]
[8]
[10]
[13]
[14]
[15]
[16]
2. Uric Acid and Gout
[17]
[18]
[19]
[20]
[21]
[22]
[23]
[24]
[25]
[15]
[26]
[27]
[28]
[33]
[34]
[26]
[35]
[36]
[37]
[38]
[39]
[42]
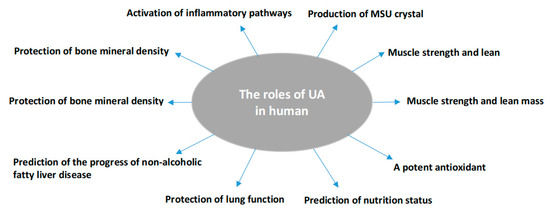
Figure 1.
[43]
[44]
[47]
[48]
3. Factors Affecting MSU Crystal Deposition Other Than Hyperuricemia
[2]
[49]
[50]
vice versa
[51]
[52]
[53]
[54]
[55]
[56]
[57]
4. The Causes of Hyperuricemia Irrelevant to Gout
[58]
[59]
[60]
[61]
[62]
[58]
[63]
[64]
[65]
[66]
[67]
[68]
[69]
[70]
[71]
[72]
[58]
[73]
[74]
References
- Kasper, D.; Hauser, S.; Longo, D.; Jameson, J.L.; Loscalzo, J. Harrison’s Principles of Internal Medicine, 19th ed.; Mcgraw-Hill: New York, NY, USA, 2015.
- Brucato, A.; Cianci, F.; Carnovale, C. Management of Hyperuricemia in Asymptomatic Patients: A Critical Appraisal. Eur. J. Intern. Med. 2020, 74, 8–17.
- Zhang, Q.; Gong, H.; Lin, C.; Liu, Q.; Baima, Y.; Wang, Y.; Lin, J. The prevalence of gout and hyperuricemia in middle-aged and elderly people in Tibet Autonomous Region, China: A preliminary study. Medicine 2020, 99, e18542.
- Boocock, J.; Leask, M.; Okada, Y.; Matsuo, H.; Kawamura, Y.; Shi, Y.; Li, C.; Mount, D.B.; Mandal, A.K.; Wang, W.; et al. Genomic dissection of 43 serum urate-associated loci provides multiple insights into molecular mechanisms of urate control. Hum. Mol. Genet. 2020, 29, 923–943.
- Towiwat, P.; Chhana, A.; Dalbeth, N. The Anatomical Pathology of Gout: A Systematic Literature Review. BMC Musculoskelet. Disord. 2019, 20, 140.
- Kuo, C.F.; Grainge, M.J.; Zhang, W.; Doherty, M. Global epidemiology of gout: Prevalence, incidence and risk factors. Nat. Rev. Rheumatol. 2015, 11, 649–662.
- Singh, G.; Lingala, B.; Mithal, A. Gout and hyperuricaemia in the USA: Prevalence and trends. Rheumatology 2019, 58, 2177–2180.
- Bardin, T.; Richette, P. Definition of hyperuricemia and gouty conditions. Curr. Opin. Rheumatol. 2014, 26, 186–191.
- Lin, K.C.; Lin, H.Y.; Chou, P. The interaction between uric acid level and other risk factors on the development of gout among asymptomatic hyperuricemic men in a prospective study. J. Rheumatol. 2000, 27, 1501–1505.
- Dalbeth, N.; House, M.E.; Aati, O.; Tan, P.; Franklin, C.; Horne, A.; Gamble, G.D.; Stamp, L.K.; Doyle, A.J.; McQueen, F.M. Urate crystal deposition in asymptomatic hyperuricaemia and symptomatic gout: A dual energy CT study. Ann. Rheum. Dis. 2015, 74, 908–911.
- Schlesinger, N.; Norquist, J.M.; Watson, D.J. Serum urate during acute gout. J. Rheumatol. 2009, 36, 1287–1289.
- Lee, J.S.; Kwon, O.C.; Oh, J.S.; Kim, Y.G.; Lee, C.K.; Yoo, B.; Hong, S. Clinical features and recurrent attack in gout patients according to serum urate levels during an acute attack. Korean J. Intern. Med. 2020, 35, 240–248.
- Singh, A.J.; Reddy, S.G.; Kundukulam, J. Risk factors for gout and prevention: A systematic review of the literature. Curr. Opin. Rheumatol. 2011, 23, 192–202.
- Dalbeth, N.; Stamp, L. Hyperuricaemia and gout: Time for a new staging system? Ann. Rheum. Dis. 2014, 73, 1598–1600.
- Bonino, B.; Leoncini, G.; Russo, E.; Pontremoli, R.; Viazzi, F. Uric acid in CKD: Has the jury come to the verdict? J. Nephrol. 2020, 33, 715–724.
- Verzola, D.; Ratto, E.; Villaggio, B.; Parodi, E.L.; Pontremoli, R.; Garibotto, G.; Viazzi, F. Uric acid promotes apoptosis in human proximal tubule cells by oxidative stress and the activation of NADPH oxidase NOX 4. PLoS ONE 2014, 9, e115210.
- Rahimi-Sakak, F.; Maroofi, M.; Rahmani, J.; Bellissimo, N.; Hekmatdoost, A. Serum uric acid and risk of cardiovascular mortality: A systematic review and dose-response meta-analysis of cohort studies of over a million participants. BMC Cardiovasc. Disord. 2019, 19, 218.
- Spitsin, S.; Koprowski, H. Role of uric acid in Alzheimer’s disease. J. Alzheimers Dis. 2010, 19, 1337–1338.
- He, Q.; You, Y.; Yu, L.; Yao, L.; Lu, H.; Zhou, X.; Wu, S.; Chen, L.; Chen, Y.; Zhao, X. Uric acid levels in subjects with schizophrenia: A systematic review and meta-analysis. Psychiatry Res. 2020, 292, 113305.
- Ellmore, T.M.; Suescun, J.; Castriotta, R.J.; Schiess, M.C. A Study of the Relationship Between Uric Acid and Substantia Nigra Brain Connectivity in Patients with REM Sleep Behavior Disorder and Parkinson’s Disease. Front. Neurol. 2020, 11, 815.
- Rentzos, M.; Nikolaou, C.; Anagnostouli, M.; Rombos, A.; Tsakanikas, K.; Economou, M.; Dimitrakopoulos, A.; Karouli, M.; Vassilopoulos, D. Serum uric acid and multiple sclerosis. Clin. Neurol. Neurosurg. 2006, 108, 527–531.
- Meng, X.; Huang, X.; Deng, W.; Li, J.; Li, T. Serum uric acid a depression biomarker. PLoS ONE 2020, 15, e0229626.
- Floriano, J.P.; Nahas, P.C.; de Branco, F.M.S.; Dos Reis, A.S.; Rossato, L.T.; Santos, H.O.; Limirio, L.S.; Ferreira-Filho, S.R.; de Oliveira, E.P. Serum Uric Acid Is Positively Associated with Muscle Mass and Strength, but Not with Functional Capacity, in Kidney Transplant Patients. Nutrients 2020, 12, 2390.
- Trindade, D.B.; de Araujo, V.A.; Franco, E.P.; Fernandes, R.C.; Carvalho, A.; Pimentel, G.D. Serum uric acid concentration is not associated with handgrip strength, lean body mass or survival in gastrointestinal cancer patients. Clin. Nutr. ESPEN 2020, 37, 75–79.
- Wang, X.J.; Qian, X.W.; Zhang, X.; Han, L.; Zheng, Y.Q.; Wu, T.; Qin, G.Y.; Ye, Z.B.; Xiao, J. Association of serum uric acid with thyroid function in health check-up participants. Chin. Med. J. 2020, 133, 1409–1414.
- Tariq, M.A.; Shamim, S.A.; Rana, K.F.; Saeed, A.; Malik, B.H. Serum Uric Acid—Risk Factor for Acute Ischemic Stroke and Poor Outcomes. Cureus 2019, 11, e6007.
- Fujikawa, H.; Sakamoto, Y.; Masuda, N.; Oniki, K.; Kamei, S.; Nohara, H.; Nakashima, R.; Maruta, K.; Kawakami, T.; Eto, Y.; et al. Higher Blood Uric Acid in Female Humans and Mice as a Protective Factor against Pathophysiological Decline of Lung Function. Antioxidants 2020, 9, 387.
- Wei, F.; Li, J.; Chen, C.; Zhang, K.; Cao, L.; Wang, X.; Ma, J.; Feng, S.; Li, W.D. Higher Serum Uric Acid Level Predicts Non-alcoholic Fatty Liver Disease: A 4-Year Prospective Cohort Study. Front. Endocrinol. 2020, 11, 179.
- Kuo, C.F.; See, L.C.; Yu, K.H.; Chou, I.J.; Chiou, M.J.; Luo, S.F. Significance of serum uric acid levels on the risk of all-cause and cardiovascular mortality. Rheumatology 2013, 52, 127–134.
- Seet, R.C.; Kasiman, K.; Gruber, J.; Tang, S.Y.; Wong, M.C.; Chang, H.M.; Chan, Y.H.; Halliwell, B.; Chen, C.P. Is uric acid protective or deleterious in acute ischemic stroke? A prospective cohort study. Atherosclerosis 2010, 209, 215–219.
- Konta, T.; Ichikawa, K.; Kawasaki, R.; Fujimoto, S.; Iseki, K.; Moriyama, T.; Yamagata, K.; Tsuruya, K.; Narita, I.; Kondo, M.; et al. Association between serum uric acid levels and mortality: A nationwide community-based cohort study. Sci. Rep. 2020, 10, 6066.
- Tai, S.; Li, X.; Zhu, Z.; Tang, L.; Yang, H.; Fu, L.; Hu, X.; Fang, Z.; Zhou, S. Hyperuricemia is a Risk Factor for One-Year Overall Survival in Elderly Female Patients with Acute Coronary Syndrome. Cardiovasc. Ther. 2020, 2020, 2615147.
- Sieminska, E.; Sobczak, P.; Skibinska, N.; Sikora, J. The differential role of uric acid—The purpose or cause of cardiovascular diseases? Med. Hypotheses 2020, 142, 109791.
- Ames, B.N.; Cathcart, R.; Schwiers, E.; Hochstein, P. Uric acid provides an antioxidant defense in humans against oxidant- and radical-caused aging and cancer: A hypothesis. Proc. Natl. Acad. Sci. USA 1981, 78, 6858–6862.
- Bowman, G.L.; Shannon, J.; Frei, B.; Kaye, J.A.; Quinn, J.F. Uric acid as a CNS antioxidant. J. Alzheimers Dis. 2010, 19, 1331–1336.
- Bardyn, M.; Chen, J.; Dussiot, M.; Crettaz, D.; Schmid, L.; Langst, E.; Amireault, P.; Tissot, J.D.; Jolicoeur, M.; Prudent, M. Restoration of Physiological Levels of Uric Acid and Ascorbic Acid Reroutes the Metabolism of Stored Red Blood Cells. Metabolites 2020, 10, 226.
- Sautin, Y.Y.; Johnson, R.J. Uric acid: The oxidant-antioxidant paradox. Nucleosides Nucleotides Nucleic Acids 2008, 27, 608–619.
- Stewart, J.D.; Langlois, V.; Noone, D. Hyperuricemia and Hypertension: Links and Risks. Integr. Blood Press. Control 2019, 12, 43–62.
- Paithankar, J.G.; Kudva, A.K.; Raghu, S.V.; Patil, R.K. Radioprotective role of uric acid: Evidence from studies in Drosophila and human dermal fibroblast cells. Mol. Biol. Rep. 2020, 47, 2427–2436.
- Pan, K.; Yao, X.; Liu, M.; Zhu, Z. Association of Serum Uric Acid Status with Bone Mineral Density in Adolescents Aged 12–19 Years. Front. Med. 2020, 7, 255.
- Yao, X.; Chen, L.; Xu, H.; Zhu, Z. The Association between Serum Uric Acid and Bone Mineral Density in Older Adults. Int. J. Endocrinol. 2020, 2020, 3082318.
- Lee, H.N.; Kim, A.; Kim, Y.; Kim, G.T.; Sohn, D.H.; Lee, S.G. Higher serum uric acid levels are associated with reduced risk of hip osteoporosis in postmenopausal women with rheumatoid arthritis. Medicine 2020, 99, e20633.
- Aguayo, R.S.; Baradad, M.; Soria, X.; Abal, L.; Sanmartin, V.; Egido, R.; Gallel, P.; Casanova, J.M.; Marti, R.M. Unilateral milia-type intradermal tophi associated with underlying urate subcutaneous deposition: An uncommon cutaneous presentation of gout. Clin. Exp. Dermatol. 2013, 38, 622–625.
- Pradhan, S.; Sinha, R.; Sharma, P.; Sinha, U. Atypical Cutaneous Presentation of Chronic Tophaceous Gout: A Case Report. Indian Dermatol. Online J. 2020, 11, 235–238.
- Howren, A.; Bowie, D.; Choi, H.K.; Rai, S.K.; De Vera, M.A. Epidemiology of depression and anxiety in gout: A systematic review and metaanalysis. J. Rheumatol. 2020, 48, 129–137.
- Zhou, Q.; Shao, Y.C.; Gan, Z.Q.; Fang, L.S. Lower vitamin D levels are associated with depression in patients with gout. Neuropsychiatr. Dis. Treat. 2019, 15, 227–231.
- Pascart, T.; Ramon, A.; Ottaviani, S.; Legrand, J.; Ducoulombier, V.; Houvenagel, E.; Norberciak, L.; Richette, P.; Becce, F.; Ornetti, P. Association of Specific Comorbidities with Monosodium Urate Crystal Deposition in Urate-Lowering Therapy-Naive Gout Patients: A Cross-Sectional Dual-Energy Computed Tomography Study. J. Clin. Med. 2020, 9, 1295.
- Sun, R.; Lu, J.; Li, H.; Cheng, X.; Xin, Y.; Li, C. Evaluation of Febuxostat Initiation During an Acute Gout Attack: A Prospective, Randomized Clinical Trial. Jt. Bone Spine 2020, 87, 461–466.
- Chhana, A.; Lee, G.; Dalbeth, N. Factors influencing the crystallization of monosodium urate: A systematic literature review. BMC Musculoskelet. Disord. 2015, 16, 296.
- Aliste-Fernandez, M.; San-Jose, P.; Aguadero, V. White blood cell count and total protein concentration to predict the absence of microcrystals in synovial fluid. Clin. Biochem. 2020, 83, 81–85.
- Cao, J.Y.; Waldman, B.; O’Connell, R.; Sullivan, D.R.; Scott, R.S.; Aryal, N.; Gebski, V.; Marschner, I.; Taskinen, M.R.; Simes, J.R.; et al. Uric acid predicts long-term cardiovascular risk in type 2 diabetes but does not mediate the benefits of fenofibrate: The FIELD study. Diabetes Obes. Metab. 2020, 22, 1388–1396.
- Liang, J.; Jiang, Y.; Huang, Y.; Song, W.; Li, X.; Ou, J.; Wei, Q.; Gu, J. The comparison of dyslipidemia and serum uric acid in patients with gout and asymptomatic hyperuricemia: A cross-sectional study. Lipids Health Dis. 2020, 19, 31.
- Pascual, E.; Addadi, L.; Andres, M.; Sivera, F. Mechanisms of crystal formation in gout-a structural approach. Nat. Rev. Rheumatol. 2015, 11, 725–730.
- Martillo, M.A.; Nazzal, L.; Crittenden, D.B. The crystallization of monosodium urate. Curr. Rheumatol. Rep. 2014, 16, 400.
- Pritzker, K.P.; Gay, S.; Jimenez, S.A.; Ostergaard, K.; Pelletier, J.P.; Revell, P.A.; Salter, D.; van den Berg, W.B. Osteoarthritis cartilage histopathology: Grading and staging. Osteoarthr. Cartil. 2006, 14, 13–29.
- Dang, N.L.H.; Kim, J.K.; Lee, K.B. Crystal-Induced Arthritis After Total Ankle Arthroplasty. J. Am. Podiatr. Med. Assoc. 2019, 109, 159–161.
- Ning, Y.; Yang, G.; Chen, Y.; Zhao, X.; Qian, H.; Liu, Y.; Chen, S.; Shi, G. Characteristics of the Urinary Microbiome from Patients With Gout: A Prospective Study. Front. Endocrinol. 2020, 11, 272.
- Wilhelmi de Toledo, F.; Grundler, F.; Goutzourelas, N.; Tekos, F.; Vassi, E.; Mesnage, R.; Kouretas, D. Influence of Long-Term Fasting on Blood Redox Status in Humans. Antioxidants 2020, 9, 496.
- Yamamoto, T.; Xie, J.; Li, Z.; Field, C.; Block, C.; Taylor, T. Effect of Uric Acid Control on Serum Creatinine. J. Clin. Rheumatol. 2019, 25, 279–283.
- Kubota, M. Hyperuricemia in Children and Adolescents: Present Knowledge and Future Directions. J. Nutr. Metab. 2019, 2019, 3480718.
- Mishima, E.; Anzai, N.; Miyazaki, M.; Ab. Uric Acid Elevation by Favipiravir, an Antiviral Drug. Tohoku J. Exp. Med. 2020, 251, 87–90.
- Batandier, C.; Poyot, T.; Marissal-Arvy, N.; Couturier, K.; Canini, F.; Roussel, A.M.; Hininger-Favier, I. Acute emotional stress and high fat/high fructose diet modulate brain oxidative damage through NrF2 and uric acid in rats. Nutr. Res. 2020, 79, 23–34.
- Yoo, I.H.; Kim, W.; Cho, J.; Kim, H.; Lim, B.C.; Hwang, H.; Chae, J.H.; Choi, J.; Kim, K.J. Erratum to: Elevated Serum Uric Acid in Benign Convulsions with Mild Gastroenteritis in Children. J. Clin. Neurol. 2020, 16, 181.
- Hase, R.; Kurata, R.; Ishida, K.; Kurita, T.; Muranaka, E.; Mito, H. Acute Gouty Arthritis During Favipiravir Treatment for Coronavirus Disease 2019: A Case Report. Intern. Med. 2020, 59, 2327–2329.
- Abhishek, A.; Valdes, A.M.; Jenkins, W.; Zhang, W.; Doherty, M. Triggers of acute attacks of gout, does age of gout onset matter? A primary care based cross-sectional study. PLoS ONE 2017, 12, e0186096.
- Flynn, T.J.; Cadzow, M.; Dalbeth, N.; Jones, P.B.; Stamp, L.K.; Hindmarsh, J.H.; Todd, A.S.; Walker, R.J.; Topless, R.; Merriman, T.R. Positive association of tomato consumption with serum urate: Support for tomato consumption as an anecdotal trigger of gout flares. BMC Musculoskelet. Disord. 2015, 16, 196.
- Hazard, A.; Bourrion, B.; Dechaine, F.; Fournier, L.; Francois, M. Lack of evidence for allopurinol for the prevention of a first gout attack in asymptomatic hyperuricemia: A systematic review. Eur. J. Clin. Pharmacol. 2020, 76, 897–899.
- Cortese, F.; Giordano, P.; Scicchitano, P.; Faienza, M.F.; De Pergola, G.; Calculli, G.; Meliota, G. Uric acid in metabolic and cerebrovascular disorders: A review. Curr. Vasc. Pharmacol. 2019, 18, 610–618.
- Zamora, A.E.; Naik, R. Calcium Pyrophosphate Deposition Disease. Available online: (accessed on 31 December 2020).
- Felten, R.; Duret, P.M.; Gottenberg, J.E.; Spielmann, L.; Messer, L. At the crossroads of gout and psoriatic arthritis: “psout”. Clin. Rheumatol. 2020, 39, 1405–1413.
- Chiang, S.L.; Ou, T.T.; Wu, Y.J.; Tu, H.P.; Lu, C.Y.; Huang, C.M.; Kuo, T.M.; Wang, T.N.; Chou, C.H.; Ko, Y.C. Increased level of MSU crystal-bound protein apolipoprotein A-I in acute gouty arthritis. Scand. J. Rheumatol. 2014, 43, 498–502.
- Cumpelik, A.; Ankli, B.; Zecher, D.; Schifferli, J.A. Neutrophil microvesicles resolve gout by inhibiting C5a-mediated priming of the inflammasome. Ann. Rheum. Dis. 2016, 75, 1236–1245.
- Hwangbo, D.S.; Lee, H.Y.; Abozaid, L.S.; Min, K.J. Mechanisms of Lifespan Regulation by Calorie Restriction and Intermittent Fasting in Model Organisms. Nutrients 2020, 12, 1194.
- Filippou, G.; Scanu, A.; Adinolfi, A.; Picerno, V.; Toscano, C.; Bortoluzzi, A.; Frediani, B.; Govoni, M.; Punzi, L.; Scire, C.A. The two faces of the same medal... or maybe not? Comparing osteoarthritis and calcium pyrophosphate deposition disease: A laboratory and ultrasonographic study. Clin. Exp. Rheumatol. 2020, 39, 66–72.
