DataData Envelopment Analysis (DEA) Envelopment Analysis (DEA) is a powerful non-parametric engineering tool for estimating technical efficiency and the production capacity of service units. The Complex-of-Needs Allocation Model proposed by Nepomuceno et al. (2020) is a two-step methodology for prioritizing hospital bed vacancy and reallocation during the COVID-19 pandemic.
The framework determines the production capacity of hospitals through Data Envelopment Analysis and incorporates the Complexity of Needs in two categories for the reallocation of beds throughout the medical specialties. As a result, we have a set of inefficient health-care units presenting less complex bed slacks to be reduced, i.e. to be allocated for patients presenting more severe conditions.
- Data Envelopment Analysis
- COVID-19
- Hospital Efficiency
- Bed Allocation
- Complexity of Needs
The Model Explained [1]
The first step consists of applying non-parametric frontier estimations for the full production capacity of the health service units (the maximum feasible production configuration for each hospital) based on hospital internments as the main output and hospital beds as one of the many discretionary resources. Similar to many assessments of health systems efficiency, the number of beds is considered a proxy for hospital capital [2][3][4]. That way, the lower the usage of this resource means the higher efficiency for the health service unit. The objective in this assessment, however, is to provide an optimal number of beds to be evacuated and allocated for potential COVID-19 cases, instead of reduced.
For the second step, the optimal number of beds to be reallocated (based on the best practices) are prioritized according to the Complexity of Needs for each medical specialty. The Complexity of Needs in the Brazilian health system is the degree of complexity each health problem presents, and the requirement for specialized knowledge. There are three categories: Basic Care, Moderate Complexity and High Complexity. Each category is defined in the Box 1.
Box 1: Complexity of Needs Categories
|
Basic Care: The first level characterized by a set of actions and practices using low-density technologies to solve health issues of greater frequency but low severity, including a list of simpler and cheaper procedures. The procedures in this category are capable of meeting most of the community's common health problems. |
|
Moderate Complexity: composed by actions and services aiming at meeting the main public health issues whose assistance in the clinical practice requires the availability of specialized professionals and the usage of technological resources for diagnostic, support and treatment. |
|
High Complexity: common for more severe health issues, this category is characterized by a set of procedures involving high technology and high cost, aiming at providing access to high-specialized knowledge and qualified services. |
Hospitalizations have moderate (



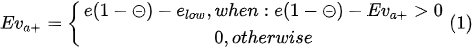
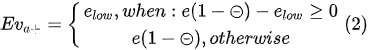
The optimal feasible contraction (evacuations) of moderate complexity beds is:
Where: 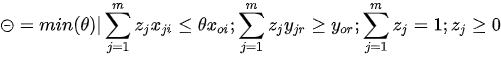
Equation (1) and (2) states that the optimal number for bed evacuations of high complexity internments depends on the number of evacuated beds of moderate complexity. In other words, the optimal number for bed evacuations of high complexity internments is the remaining feasible contraction of beds after all moderate complexity internments are evacuated. As an example, considering an efficiency score = 0.8, the service unit may improve efficiency by producing the same result using (1 – 0.8) = 20% fewer resources. Considering 100 hospital beds allocated to internments of both Complexity of Needs as the discretionary input | = 15 & = 85, the number of beds to be evacuated having moderate complexity is = = 15 beds; and the number of beds to be evacuated having high complexity is = = 20 – 15 = 5 beds.
Full concepts and definitions concerning the Complexity of Needs assistance in the Brazilian Health System and a list with the related medical specialties can be accessed in CONASS (2020) [7].
This entry refers to 10.1155/2020/8857553
References
- Thyago C. C. Nepomuceno; Wilka M. N. Silva; Késsia T. C. Nepomuceno; Isloana K. F. Barros; A DEA-Based Complexity of Needs Approach for Hospital Beds Evacuation during the COVID-19 Outbreak. Journal of Healthcare Engineering 2020, 2020, 1-9, 10.1155/2020/8857553.
- Hashem Omrani; Khatereh Shafaat; Ali Emrouznejad; An integrated fuzzy clustering cooperative game data envelopment analysis model with application in hospital efficiency. Expert Systems with Applications 2018, 114, 615-628, 10.1016/j.eswa.2018.07.074.
- T. Nepomuceno; W.M.D.N. Silva; L.G.D.O. Silva; PMU7 Efficiency-Based Protocols for BEDS Evacuation during the COVID-19 Pandemic. Value in Health 2020, 23, S604-S604, 10.1016/j.jval.2020.08.1219.
- Diogo Cunha Ferreira; Alexandre Morais Nunes; Rui Cunha Marques; Doctors, nurses, and the optimal scale size in the Portuguese public hospitals. Health Policy 2018, 122, 1093-1100, 10.1016/j.healthpol.2018.06.009.
- R. D. Banker; A. Charnes; W. W. Cooper; Some Models for Estimating Technical and Scale Inefficiencies in Data Envelopment Analysis. Management Science 1984, 30, 1078-1092, 10.1287/mnsc.30.9.1078.
- Nepomuceno, T. C., & Costa, A. P. C. (2019). Resource allocation with Time Series DEA applied to Brazilian Federal Saving banks. Economics Bulletin, 39(2), 1384-1392.
- Brasil. Conselho Nacional de Secretários de Saúde. (2007). Assistência de Média e Alta Complexidade no SUS. Conselho Nacional de Secretários de Saúde, Brasília. Availible at: http://bvsms.saude.gov.br/bvs/publicacoes/colec_progestores_livro9.pdf. Last accessed on April 5, 2020.