Suprachoroidal drug delivery technology has advanced rapidly and emerged as a promising administration route for a variety of therapeutic candidates, targeting multiple ocular diseases, ranging from neovascular age-related macular degeneration to choroidal melanoma. This entry summarizes the latest preclinical and clinical progress in suprachoroidal delivery of therapeutic agents, focusing on small molecule suspensions.
- suprachoroidal
- microinjector
- SCS
1. Current Treatment Landscape and Unmet Clinical Need
Highly active research and development efforts are ongoing to optimize ocular drug delivery for potential improvement in efficacy, safety, and durability benefits. The most common ocular drug delivery method for treating posterior eye diseases is intravitreal (IVT) injections [1][2][3][4]. It is estimated that 24.4 million IVT injections were performed globally in 2019 with 6.9 million of these injections performed in the United States, most often for neovascular age-related macular degeneration (nAMD) and diabetic macular edema (DME) [5]. While IVT injections of anti-vascular endothelial growth factor (anti-VEGF) therapies are commonly performed in an office setting, and have demonstrated remarkable therapeutic benefits in controlled clinical trials [6][7][8][9][10][11][12][13][14][15][16][17], real world data on patients receiving IVT injections of anti-VEGF therapies show a much more modest improvement in patients’ vision [18][19][20][21][22]. This disparity may relate to treatment burden, with patients undertreated due to the inability to maintain the frequent treatments in fixed regimens utilized in clinical trials. Furthermore, a subset of patients responds incompletely to anti-VEGF treatments regardless of the frequency of administration [23]. Other pharmacological agents such as corticosteroids, that are commonly injected intravitreally for posterior eye diseases, may have undesirable side effects, including ocular hypertension and/or cataracts, due to their anterior chamber exposure [24][25][26][27][28][29][30][31].
In addition to posterior eye diseases that are currently treated with IVT injections, there remain significant unmet clinical needs in other ocular disorders, such as glaucoma, that are currently treated topically with eye drops and/or surgery. Glaucoma patients face challenges including compliance with proper administration of topical eye drops of beta blockers (e.g., timolol), alpha agonists (e.g., brimonidine), Rho kinase inhibitors (e.g., netarsudil), and prostaglandin analogs (e.g., latanoprost) [32][33][34]. These drugs act by decreasing the production and/or increasing the outflow of the aqueous humor. In some instances, combination treatments may also be required to provide adequate treatment. Specifically related to topical eye drops, in addition to patient compliance, there are challenges maintaining drug concentrations above therapeutic levels due to the high clearance rate via nasolacrimal drainage and/or dilution from production of reflex tears [35][36]. Taken together, there remains an unmet clinical need for improved delivery to targeted ocular tissues, compared to current topical or intravitreal delivery methods.
One possible solution to address this unmet need is the delivery of therapeutic agents into the suprachoroidal space (SCS). The SCS is the ‘potential space’ between the sclera and choroid that circumferentially spans the entire posterior segment of the eye from the ciliary body rearwards. Potential spaces in the body are areas between directly apposed organs or tissue layers. These potential spaces, such as the pleural space, the pericardial cavity, and the SCS, expand when fluid enters and flows within the space and collapse upon fluid egress. These potential spaces can serve as “druggable” targets for the delivery of therapeutic agents.
Drug delivery to the SCS has unique potential advantages in that, (1) it specifically targets affected chorioretinal tissues with posterior and circumferential spread of the drug administered, (2) it may provide sustained drug kinetic release profiles, depending on the physicochemical formulation properties, and (3) it may spare the unaffected anterior segment of the eye and the vitreous chamber, thus minimizing risks associated with off-target effects to potentiate safety [37][38]. To reliably access the SCS, microneedles have been designed to be long enough to penetrate through the sclera, delivering therapeutic agents into the SCS, without penetrating into the vitreous. The therapeutic agent flows both circumferentially and posteriorly towards the back of the eye, targeting chorioretinal tissues (
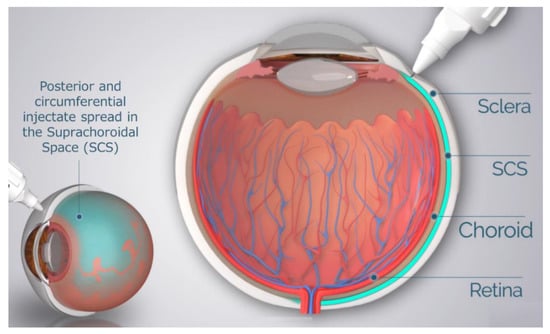
Figure 1. Schematic of Microneedle Injection into the Suprachoroidal Space (SCS).
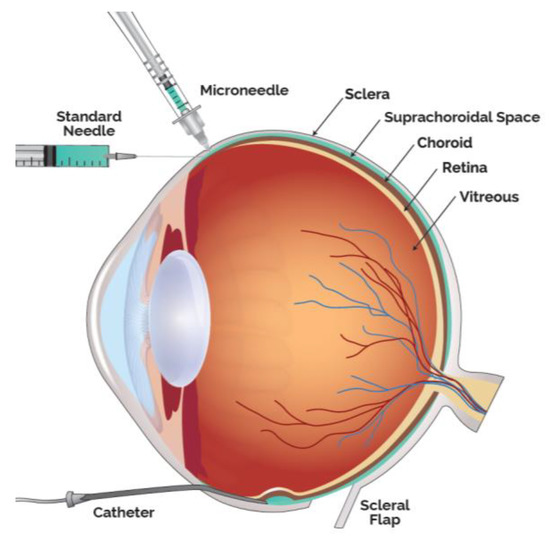
Figure 2. Modalities to Administer Therapeutic Agents into the Suprachoroidal Space (SCS).
The objective of this review article is to summarize the current status of preclinical and clinical therapeutic agents that have been administered into the SCS. As described in this review article, SC administration may offer unique advantages, such as compartmentalization away from the anterior segment and prolonged durability with appropriate formulations. Clinical trials with suprachoroidally administered triamcinolone acetonide, a small molecule suspension, have already demonstrated safety and efficacy. This route of administration may further play a significant role in ocular drug delivery of other novel therapeutic agents for a wide range of ocular diseases, spanning from glaucoma and ocular melanoma to several common chorioretinal diseases, such as age-related macular degeneration (AMD) and diabetic retinopathy (DR).
2. Small Molecule Suspensions
2.1. Corticosteroid
2.1. Corticosteroid
Safety and efficacy of an SC-delivered investigational formulation of triamcinolone acetonide (TA) has been evaluated in multiple controlled clinical trials [39][40][41][42][43] and its pharmacokinetic and pharmacodynamic characteristics have also evaluated in multiple animal studies.
Preclinically, favorable pharmacokinetics of SC TA has been demonstrated. This commonly used corticosteroid is a crystalline small molecule with low aqueous solubility (ranging between 0.02 mg/mL at 28 °C and 0.03 mg/mL at 50 °C [44]) and has historically been administered via topical, periocular or intravitreal routes, for the treatment of ocular inflammation. At a particle size distribution in the low micrometer range after micronization, it has been demonstrated that the concentration of TA in the SCS in various preclinical models can be maintained above therapeutic levels for an extended period of time [45].
With respect to ocular distribution, when TA was injected into the SCS in rabbits, TA concentrations in the retinal pigment epithelium (RPE)-choroid-sclera (RCS) and the retina were significantly higher than those in both the aqueous humor and the vitreous through the duration of the study (91 days) [46]. This study illustrated that drug delivery into the SCS can be compartmentalized, away from the anterior segment and the vitreous humor, preferentially targeting chorioretinal tissues and provide sustained PK profile.
Pharmacodynamically, efficacy of SC TA was supported in a porcine model of uveitis. In this model, lipopolysaccharides (LPS) were introduced into pigs to induce uveitis [47]. Suprachoroidal administration of TA meaningfully reduced inflammation over time. In an in vivo model, Chen et al. showed that TA delivered via the SC route provided excellent targeting to the posterior retina; resulting in improved efficacy with significantly fewer aqueous humor cells and lower vitreous opacity scores compared to TA administered via the sub-Tenon route in rabbits [48]. Similar studies have also shown that TA administered via the SC or IVT routes in a model of endotoxin-induced panuveitis in albino rabbits led to comparable efficacy in the reduction of ocular inflammation [49]. Furthermore, an in vivo porcine model of acute uveitis demonstrated that 1/10th the dose of TA administered suprachoroidally was as effective as the full dose administered intravitreally, with no adverse effects [47]. Using a similar porcine model, another study showed that TA administered suprachoroidally was more effective in reducing ocular inflammation than low dose oral prednisone (0.1 mg/kg/day) administered for three days, and resulted in an improved rate of reduction in inflammation when compared to high dose oral prednisone (1 mg/kg/day) [50]. These results validate SC administration as a potential drug delivery route for small molecule suspensions.
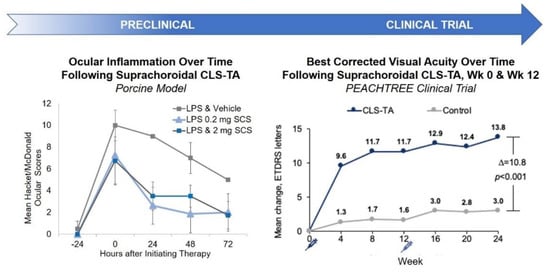
Figure 3.
2.2. Tyrosine Kinase Inhibitor
2.2. Tyrosine Kinase Inhibitor
Another small molecule suspension that has been evaluated for potential SC delivery is axitinib. Axitinib has several properties with attractive therapeutic potential. It is a highly potent tyrosine kinase inhibitor (TKI) with pan-VEGF inhibition and high binding affinities [51]. Pan-VEGF inhibition may have benefits over current specific VEGF-A inhibition for the treatment of nAMD, DR, and DME, as other VEGF ligands such as VEGF-C and VEGF-D, have been shown to be upregulated after anti-VEGF-A administration both locally, after the treatment of nAMD, and systemically [52][53]. This upregulation of other VEGF ligands could contribute to tachyphylaxis, a form of treatment resistance, and lead to refractory cases clinically. Axitinib has also been shown to more effectively inhibit angiogenic sprouts than anti-VEGF-A inhibition in an in vitro angiogenesis model [54]. One recent phase 2 clinical trial demonstrated that broad VEGF inhibition yielded a statistically significantly better visual outcome in nAMD than focused VEGF-A inhibition [55]. In addition, axitinib is a more highly potent TKI than others that have undergone assessment in ocular clinical trials [56] and has demonstrated more potent inhibition of murine corneal neovascularization, compared to other TKIs at the same dose [57]. Axitinib has been shown to not only inhibit angiogenesis, but also regress established neovascularization in a preclinical choroidal neovascularization model, which may be more relevant to potential clinical use [58]. Finally, axitinib has shown better biocompatibility with ocular cells, including retinal pigment epithelial cells, compared to other TKIs in an in vitro study, suggesting the potential for intrinsic safety benefits [59].
50
2.3. Complement Inhibitor & Plasma Kallikrein Inhibitor
2.3. Complement Inhibitor & Plasma Kallikrein Inhibitor
Additional small molecules have been investigated to target other signaling pathways, such as the complement system, a potential treatment target for non-neovascular age-related macular degeneration (dry AMD). Suprachoroidally administered A01017 (Achillion Pharamaceuticals, Blue Bell, PA, USA now AstraZeneca, Cambridge, UK), a potent small molecule complement factor D inhibitor [63], was well tolerated with sustained drug levels in posterior segment tissue of rabbits for up to 92 days. Similar to TA and axitinib, a high level of A01017 was observed in the RCS and retina throughout the entire duration of the study with an estimated half-life of approximately 66–76 days. Low or no quantifiable A01017 was detected in the vitreous humor, aqueous humor or plasma.
Yet another example of a small molecule suspension that has demonstrated preclinical ocular tolerability and sustained ocular drug levels is BCX4161 (BioCryst Pharmaceuticals, Durham, NC, USA), a potent and selective inhibitor of human plasma kallikrein, that is elevated in patients with diabetic macular edema [64]. BCX4161 was suprachoroidally administered to Dutch-Belted rabbits and was found to be well tolerated with sustained levels detected throughout the RCS and both central and peripheral retina over the 12-week study duration. Furthermore, the concentration of BCX4161 in the retina was 1 to 2 orders of magnitude higher than levels in the vitreous humor.
Table 1.
| Therapeutic Agent | Therapeutic Class | Disease | Phase (Species) | Duration | Key Results | Ref |
|---|---|---|---|---|---|---|
| Triamcinolone Acetonide (TA) Suspensions | Corticosteroid | Macula Edema Associated with Uveitis | Phase 3 Clinical Study | 24 weeks | In a phase 3 clinical trial for macula edema associated with noninfectious uveitis, 46.9% of the subjects treated with 2 SC injections of TA gained at least 15 ETDRS letters from baseline at 24 weeks, compared to 15.6% in the sham group | [39] |
| Axitinib Suspensions | Tyrosine kinase inhibitor | nAMD | Preclinical (Rabbit) |
10 weeks | Efficacious and sustained level of axitinib, above IC50, was observed in the posterior ocular tissues throughout the duration of the study | [61] |
| A01017 | Complement inhibitor | non-neovascular AMD | Preclinical (Rabbit) |
92 days | High level of A01017 was observed in the RCS and retinal tissues throughout the entire duration of the study. | [63] |
| BCX4161 | Plasma kallikrein inhibitor | DME | Preclinical (Rabbit) |
12 weeks | BCX4161 was well tolerated and sustained levels were observed in the RCS, peripheral and central retinal tissues throughout the duration of the study | [64] |
Abbreviations: SC: suprachoroidal; ETDRS: early treatment diabetic retinopathy study; TA: triamcinolone acetonide; nAMD: neovascular age-related macular deg
