Mycotoxins are a structurally diverse group of mostly low-molecular-weight compounds. Their structures range from single heterocyclic rings to irregularly arranged rings of six to eight members and their molecular weights are usually less than 1000 Da. Therefore, they do not induce any response in the human immune system.
- beauvericin
- enniatins
- minor mycotoxins
1. Introduction
Mycotoxins are produced mainly by the secondary metabolism of certain filamentous fungi, which grow under specific temperature and humidity and cause serious risks for human and animal health. As secondary metabolites, instead of playing a role in growth and normal metabolism of the fungus, many mycotoxins are involved in pathogenesis or in competing with other organisms [1][2][1,2].
Many of the toxigenic fungi are ubiquitous and, in some cases, have a conjunction with food and feed production. From these, the most common toxigenic species belong to four genera: Fusarium, Aspergillus, Penicillium, and Alternaria [3]. Fusarium and Alternaria usually produce mycotoxins before harvest or in freshly harvested products, whereas Aspergillus and Penicillium species represent a higher risk during drying and storage of food and feed products [1][3][1,3]. Fusarium genus includes over 90 described species and is responsible for the production of some of the most important classes of mycotoxins: trichothecenes, fumonisins, and zearalenones. Moreover, this genus produces less studied mycotoxins called minor or emerging mycotoxins: fusaproliferin, beauvericin (BEA), enniatins (ENs), and moniliformin. The toxicity of the toxins produced by Fusarium varies greatly depending on the toxin and the target organism [3][4][3,4]. The most important species that produce these toxic metabolites are Fusarium proliferatum, Fusarium subglutinans, Fusarium moniliforme, and Fusarium avenacum, involved in crop diseases, such as stalk and maize ear rot disease [5].
To date, more than 300 mycotoxins have been identified, and research is focused mainly on those that have been proven to have diverse health effects on humans and animals, like teratogenicity, carcinogenicity, and mutagenicity [6][7][6,7]. The exposure of humans to mycotoxins occurs either directly through the consumption of contaminated plant foods (e.g., cereals) or indirectly through the intake of animal-derived products (e.g., milk and eggs) that origin from animals fed with contaminated diets [6]. From the perspective of livestock breeding and nutrition, mycotoxins in feedstuffs are of dual concern. First one is connected with the safety of animal-derived food and is related to occurrence of mycotoxins in feed and their (partial) carry-over from feed to edible animal tissues such as milk, eggs, or meat. The occurrence of mycotoxins in food can be legislatively monitored (presence of aflatoxin M1 in milk [8]). The second one is connected with detrimental effects of mycotoxins on animal health and performance. Such detrimental mycotoxins include deoxynivalenol (DON), fumonisins, ochratoxin A, and zearalenone (ZEA). Most, but not all, of these mycotoxins are produced by the Fusarium species. Although these mycotoxins are significant contaminants when entering the food chain directly via food of plant origin, they are not considered relevant in food of animal origin because their carry-over from feed to animal-derived food products is negligible [9][10][11][12][9,10,11,12]. However, Fusarium species are also responsible for the production of minor mycotoxins, namely, enniatins and beauvericin, which are currently in the center of interest because of the wide range of their biological activities.
2. Beauvericin
Beauvericin (BEA) is a cyclic lactone trimer, which contains an alternate sequence of three N-methylphenylalanyl and three D-α-hydroxyisovaleryl residues (Figure 1). It was first isolated from the fungus Beauverina bassiana, an insect pathogen [13]. The first Fusarium species identified to produce BEA was Fusarium subglutinans [14]. Subsequently, other Fusarium species such as Fusarium bulbicola, Fusarium denticulatum, Fusarium lactis, Fusarium phyllophillum, Fusarium pseudocircinatum, and Fusarium succisae have been proven to produce BEA [15].
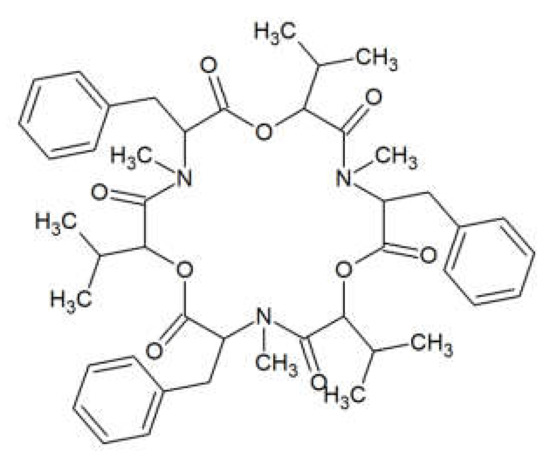
Figure 1.
Beauvericin structure.
BEA possesses insecticidal and phytotoxic properties and is involved in the etiology of insect and plant diseases caused by the producer fungal strains [16]. The antimicrobial and antibiotic activities of BEA have been tested on human or mammalian intestinal bacteria (see Table 1). BEA also showed endocrine disrupting antagonistic effects at the androgen receptor [17]. It also acts on cellular level as an enzyme inhibitor [18], and as a compound inducing oxidative stress. BEA eases apoptosis, interferes with smooth muscle contraction, impedes with steatosis caused by the storage of cholesterol in liver cells, and according to various bioassays, it is believed to be toxic. Nevertheless, it was discovered that cytotoxicity of BEA depends on the dose, length, and also way of exposure [19][20][19,20], because it is able to penetrate to the body through the skin, although its permeation is relatively low [21].
Table 1. Antimicrobial effects of beauvericin and enniatins B and B1 on bacteria isolated from the human or mammalian intestinal tract.
| Beauvericin | Bacillus cereus, B. mycoides, B. pumilis, B. sphaericus, Bifidobacterium adolescentis, Clostridium perfringens, Escherichia coli, Enterococcus faecium, Eubacterium biforme, Listeria monocytogenes, Paenibacillus alvei, P. azotofixans, P. macerans, P. macquariensis, P. pabuli, P. productus, P. pulvifaciens, P. validus, Peptostreptococcus anaerobius, Pseudomonas aeruginosa, Salmonella enterica, Shigella dysenteriae, Yersinia enterocolitica, | [24][26] | [24,26] |
| Enniatin B | Escherichia coli, E. faecium, Clostridium perfringens, Listeria monocytogenes, Pseudomonas aeruginosa, Salmonella enterica, Shygella dysenteriae, Staphylococcus aureus, Yersinia enterocolitica | [36] | |
| Enniatin B1 | Bifidobacterium adolescentis | [37] |
Furthermore, the effect of BEA on human and animal health might not be just negative, BEA was also proven to have several positive qualities such as antifungal [22], antiviral [23] [23] or antibiotic effect. The antibiotic effects of BEA were tested on the following bacterial species including those from GI tract: Bacillus cereus, Bacillus mycoides, Bacillus pumilis, Bacillus sphaericus, Bifidobacterium adolescentis Clostridium perfringens, Escherichia coli, Enterococcus faecium, Eubacterium biforme, Listeria monocytogenes, Paenibacillus alvei, Paenibacillus azotofixans, Paenibacillus macerans, Paenibacillus macquariensis, Paenibacillus pabuli, Paenibacillus productus, Paenibacillus pulvifaciens, Paenibacillus Validus, Peptostreptococcus anaerobius, Pseudomonas aeruginosa, Salmonella enterica, Shigella dysenteriae, Yersinia enterocolitica, and two strains of Staphylococcus aureus, using microbial bioassay techniques [24][25][26][24,25,26]. The highest activity was observed for C. perfringens with a minimum inhibitory concentration (MIC) of 1 ng per disc, followed by S. enterica (MIC = 10 ng per disc) and B. pumilus together with L. monocytogenes (MIC = 100 ng per disc). Generally, Gram-positive bacteria were more inhibited than Gram-negative ones. Furthermore, BEA, which acts as an inhibitor of activated T cells, is a possible drug candidate for the colon inflammation treatment [27].
3. Enniatins
Enniatins (ENs) were discovered in the cultures of Fusarium orthoceras, later renamed Fusarium oxysporum [28]. ENs represent a large group of related mycotoxins with the structure of cyclic hexadepsipeptides, comprised of D-α-hydroxy-isovaleryl-(2-hydroxy-3-methylbutanoic acid) and N-methylamino acid residues linked with peptide bonds and intra-molecular ester (lactone) bonds (see Figure 2). ENs of type A and B contain N-methyl-valine or N-methyl-isoleucine or the mixtures of these two amino acids [29]. Currently, 29 naturally occurring enniatin analogues are known [30] [30] and seven of them (ENs A, A1, B, B1, B2, B3, and B4) have been found in cereals. ENs A, A1, B, and B1 are most frequently reported in foods and feeds [15]. ENs are produced by strains of some species of Fusarium, Alternaria, Halosarpheia, and Verticillium genera [31].
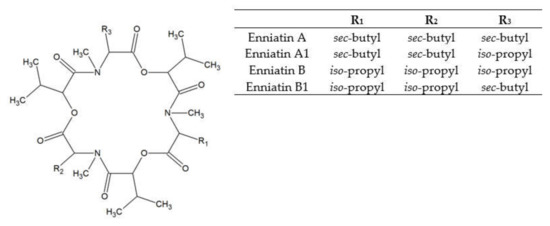
Figure 2.
Enniatin structure.
ENs are phytotoxic [32], antifungal (towards Aspergillus flavus, A. parasiticus, A. fumigatus, A. ochraceus, Beauveria bassiana, Fusarium verticilloides, F. sporotrichioides, F. tricinctum, F. poae, F. oxysporum, F. proliferatum, Penicillium expansum, and Trichoderma harzianum) [24], antiyeast (towards Candida albicans, Trichosporum cutaneum, and Cryptococcus neoformans) [33] [33] and antibacterial (towards Bacillus subtilis, Mycobacterium spp., Pseudomonas aeruginosa, Staphylococcus aureus, Escherichia coli, and lactic acid bacteria) [34] [34] and insecticidal agents [35]. The antimicrobial activities of ENs tested on human or mammalian intestinal bacteria are shown in Table 1.
ENs have cytotoxic activities that have been tested on several mammalian and cancer cell types such us Hep-G2 [36][38][36,38], Caco-2, HT-29 [36], MRC-5 [38] or CHO-K1 cells [39]. These studies gave proof of the potential cytotoxicity of ENs in mammal cell lines at quite low micromolar concentrations. Furthermore, synergistic effect of the combination of several individual ENs was observed [39]. It has been proved that ENs might even have an effect of genotoxicity. When eaten in larger doses, symptoms that are frequently occurring in transition cows include reduced rumen fermentation [40]. ENs are able to penetrate to the body through the skin and their permeation is higher than that of BEA with the highest permeation found in enniatin B (k (p, v) = 9.44 × 10–6 cm/h) [21].
ENs are also known as ionophores [41][42][41,42], antibiotics [24], and antimicrobial compounds [43][44] [43,44] against human, animal, and plant pathogenic bacteria with no selectivity between Gram-positive and Gram-negative bacteria. Undeniable benefit of ENs is also an anti-helminthic effect [45]. Their biological activities may be explained by their ability to selectively increase the flux of alkali metal ions through biological membranes. Using the patch clamp technique in the inside-out mode, enniatin was shown to incorporate into the cell membrane, where it forms pores selective for cations [46]. Recent study suggested that EN B1 can destabilize the lysosome-associated membrane proteins 2 which results in the alkalinization of lysosomes and partial lysosomal membrane permeabilization [47]. In addition to their effect on cells, ENs exerts a hypolipidemic effect partly by inhibiting enzymes such as acyl-CoA: cholesterol acyl transferase (ACAT) and partly by reducing triglyceride synthesis and diminishing the free fatty acid pool in the cells. Furthermore, ENs inhibit 30,50-cyclo-nucleotide phosphodiesterase and can attach to calmodulin. Even though, ENs are currently used only to the local treatment of respiratory infections [46].
