There is a need to disentangle the etiological puzzle of age-related neurodegenerative diseases, whose clinical phenotypes arise from known, and as yet unknown, pathways that can act distinctly or in concert. Enhanced sub-phenotyping and the identification of in vivo biomarker-driven signature profiles could improve the stratification of patients into clinical trials and, potentially, help to drive the treatment landscape towards the precision medicine paradigm. The rapidly growing field of neuroimaging offers valuable tools to investigate disease pathophysiology and molecular pathways in humans, with the potential to capture the whole disease course starting from preclinical stages. Positron emission tomography (PET) combines the advantages of a versatile imaging technique with the ability to quantify, to nanomolar sensitivity, molecular targets in vivo. There is an increasing body of literature implicating dysfunction of mitochondria and endoplasmic reticulum dynamics, energy metabolism and oxidative stress within the molecular paradigm of age-related neurodegenerative diseases. The development of novel PET radioligands enables the in vivo investigation of mitochondrial and ER dysfunction in age-related neurodegenerative diseases.
- positron emission tomography
- biomarkers
- neurodegeneration
- precision medicine
- Mitochondrial Dysfunction
Please note: Below is an entry draft based on your previous paper, which is wrirren tightly around the entry title. Since it may not be very comprehensive, we kindly invite you to modify it (both title and content can be replaced) according to your extensive expertise. We believe this entry would be beneficial to generate more views for your work. In addition, no worry about the entry format, we will correct it and add references after the entry is online (you can also send a word file to us, and we will help you with submitting).
1. Introduction
It is widely accepted that age-related neurodegenerative diseases are increasingly becoming a global public health concern—in particular, Alzheimer’s disease (AD) and other late-onset dementias (LOD), with widespread socioeconomic and healthcare impacts worldwide. The increasing burden of age-related diseases is mainly due to the ageing world population and the unprecedented shift in aging demographics of individuals over 60 years of age, which is predicted to rise to two billion in 2050 [1]. Age-related neurodegenerative diseases encompass a spectrum of complex and heterogenous diseases, including AD, Parkinson’s disease (PD), Parkinson’s disease Dementia (PDD), Dementia with Lewy Bodies (DLB), the recently identified dementia form of “Limbic-predominant Age-related TDP-43 Encephalopathy (LATE)”, late-onset forms of Fronto-Temporal Dementia (FTD) and of Amyotrophic Lateral Sclerosis (ALS), as well as parkinsonian plus syndromes, such as Corticobasal Syndrome (CBS), Progressive Supranuclear Palsy (PSP) and Multiple System Atrophy (MSA). Unlike other public health challenges, such as cancer, which have seen the recent development of effective disease modifying treatments, therapies for age-related neurodegenerative diseases remain ineffective to modify the disease course, with most therapies only providing some symptomatic relief.
The majority of research across age-related neurodegenerative diseases is built upon the clinicopathological nosology model [2], whereby a specific clinical phenotype is studied aiming to unlock the underlying pathology, traditionally through post-mortem investigations and, more recently, through in vivo studies, using imaging and other biomarkers that reflect key pathological changes. Variations across diseases have been attributed to the selective vulnerability of specific neuronal subtypes to disease pathology that subsequently determine the clinical phenotypic expression. However, the majority of age-related neurodegenerative diseases are complex in nature, resulting from poorly understood interactions between genomic, environmental and lifestyle factors, across the life course, and harbor multiple pathologies; as a result, their clinical presentations can have distinct, as well as overlapping, features occurring at different levels and timepoints [3][4][5][3,4,5]. The concept that neuronal networks, rather than neuronal subtypes, could underlie differences in the clinical phenotype and the susceptibility of individuals to different neurodegenerative diseases has gained increasing interest over the last decade, aiming to unlock the paradigm of age-related neurodegenerative diseases [4][6][7][8][9][4,6,7,8,9]. In 2018, the National Institute on Aging and the Alzheimer’s Association proposed the Research Framework classification of AD to better define the diagnosis of AD, across a disease continuum from preclinical to severe clinical stages from other LOD forms, based on the in vivo AT(N) biomarker signature, corresponding to the three landmark pathological features of increased Amyloid and Tau burden, associated with a significant loss of volume and neurodegeneration [10][11][10,11]. While this classification is a step towards the application of biological signature profiles, consideration should be given to the use of a binary classification model for continuous variables, based on a predetermined threshold, as a predictive or diagnostic tool in clinical trials, especially when using a clinical phenotype, such as cognitive decline or dementia, as the primary outcome measure [12].
Almost all age-related neurodegenerative diseases can be classified into sporadic or familial forms. The discovery of fully penetrant genetic mutations in several familial neurodegenerative diseases has allowed for the investigation of the early disease pathology prior to the clinical manifestations, in these familial forms, prior to the manifestation of clinical symptoms that could help to unlock causal pathways. In the nonfamilial sporadic forms, in addition to the genetic variants that are noncausative but can confer susceptibility to disease, there is a wide range of risk factors that may affect disease onset and development, including environmental factors and exposures across the life course, cardiovascular status and hypertension, obesity, diabetes, sleep disorders and a variety of factors related to brain biological aging, such as protein misfolding and aggregation, epigenetics and perturbations in DNA damage and repair. However, not all patients with all, or some, of these risk factors will develop symptoms and signs amounting to a clinical diagnosis within their lifetime. While the interaction between genetics and disease mechanisms is indeed complex and has not been fully elucidated, it has been postulated that unraveling the genetics of age-related neurodegenerative diseases might form the basis for sub-phenotyping and/or reclassification based on genotypic divergence aiming to drive forward the application of precision medicine [13].
There is a need to disentangle the etiological puzzle of age-related neurodegenerative diseases, whose clinical phenotypes arise from known, and as yet unknown, pathways that can act distinctly or in concert (Figure 1). Over the last 40 years, preclinical animal studies and post-mortem evaluations have unlocked a number of disease mechanisms and therapeutic targets, which showed promise to translate into novel therapies for age-related neurodegenerative diseases. In AD, the main causal hypotheses involved the amyloid cascade and the tau phosphorylation-propagation hypothesis. However, the majority of clinical trials targeting these mechanisms have failed to meet their primary endpoints [14][15][16][14,15,16]. The failure of clinical trials, across age-related neurodegenerative diseases, could be due to a number of reasons such as the late initiation of treatments in the disease course, poor target engagement or selection of the tested compound, suboptimal cohort stratification and the inability to reach the required effect sizes due to inadequate sample size and/or short follow-up periods [15]. Moreover, an inadequate appreciation of the complexity of disease etiology and pathophysiology can lead to an oversimplified mono-therapeutic approach [16][16].
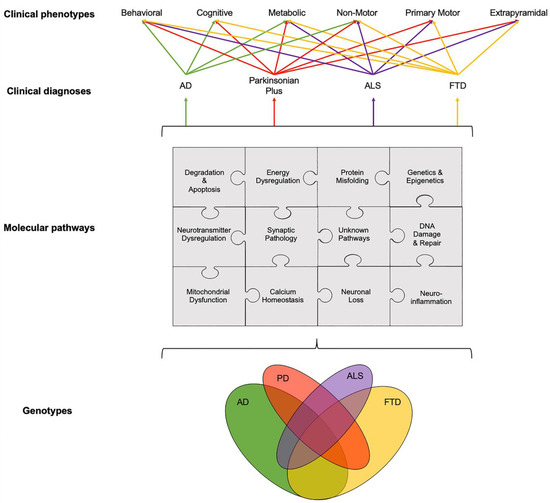
Figure 1. Schematic illustration of interlinked genotypes, molecular pathways and clinical phenotypes across age-related neurodegenerative diseases showing the overlap between various components and pathways at different levels, from genetics and molecular pathways to clinical phenotypes. Disentangling this etiological puzzle of known and yet unknown pathways acting distinctly or in concert could improve the stratification of patients into clinical trials and, potentially, help to drive the treatment landscape towards the precision medicine paradigm. The relationship between clinical diagnosis and clinical phenotypes was adapted from Ahmed et al., 2016 [3]. Abbreviations: AD: Alzheimer’s disease, ALS: Amyotrophic Lateral Sclerosis, FTD: Fronto-Temporal Dementia and PD: Parkinson’s disease.
While preclinical and post-mortem studies have, and will likely continue to, play a key role in the drug discovery process, as well as in understanding the underlying molecular mechanisms, considerations have to be given to their direct translation into humans [14][17][14,17]. For example, animal models of late-onset neurodegenerative diseases typically develop symptoms and die young, whereas in humans these diseases typically occur in late life [18]. Furthermore, post-mortem studies provide insights into pathological changes at a single timepoint (the very end stage of the disease), which can be contaminated from chronic drug treatments and other pathologies, making it difficult to disentangle whether the changes observed are a cause or consequence of neuronal death. The rapidly growing field of neuroimaging offers valuable tools to investigate disease pathophysiology and molecular pathways in vivo in humans, with the potential to capture the whole disease course. Positron emission tomography (PET) imaging combines the advantages of a versatile imaging technique with the ability to quantify, to nanomolar sensitivity, molecular targets, both in animals and in living humans. Magnetic resonance imaging (MRI) techniques can offer high spatial resolution and anatomical granularity with advanced acquisition protocols and analysis methodologies offering a platform to explore microstructural and functional connectivity, iron deposition, neuromelanin levels and neuro-hydrodynamics. Therefore, PET and MRI techniques are commonly employed in unison to extrapolate meaningful outcome measures reflecting molecular biology in vivo.
2. Dysregulation of Interlinked Molecular Pathways across Age-Related Neurodegenerative Diseases
While the temporal onset and the rate of progression can vary, clinical phenotypes, such as behavioral, cognitive, metabolic, nonmotor, primary motor and extrapyramidal, often overlap across different age-related neurodegenerative diseases (Figure 1). For example, patients with FTD can present with extrapyramidal symptoms similar to PD; AD patients can experience nonmotor symptoms such as sleep problems, which overlap with nonmotor symptoms observed in PD and parkinsonian plus syndromes, and patients with ALS can present with behavioral symptoms, such as apathy, which can overlap with FTD, parkinsonism plus syndromes and AD [19][20][21][19,20,21]. The pathogenesis and progression of age-related neurodegenerative diseases likely involves a dynamic interaction between various components and pathways at the genetic and pathological levels (Figure 1). Specific PET radioligands have been developed to target some of these molecular components, enabling the exploration of these pathways in vivo. There are a number of genotypic and molecular pathways that show varying degrees of overlap and crossover at various stages of disease etiology and progression. For example, while the clinical phenotype of three causative genes for FTD, C9orf72, MAPT and GRN, are associated with a similar behavioral variant FTD (bvFTD) presentation, the underlying protein pathology varies such that MAPT mutations are associated with tau pathology and C9orf72 and GRN mutations are associated with Tar-DNA-binding protein (TDP)-43 pathology [3]. Furthermore, a number of studies have unlocked genetic signatures that are common across different age-related neurodegenerative diseases. A meta-analysis of 1270 post-mortem brain tissue samples from AD, PD, ALS and Huntington’s disease (HD) patients identified shared gene expression signatures for 243 genes [22]. The common genes identified across these different diseases were related to functional pathways, including inflammation, synaptic signaling, metabolic dysfunction and oxidative stress. Moreover, while the causal role of epigenetics on age-related neurodegenerative diseases remains a topic of debate [23], similarities in the dysregulation of transcriptional networks and protein interaction networks have been reported [5].
It remains to be elucidated why, and how, pathologies diverge towards different clinical phenotypes and if there is a common causal mechanism that links the spectrum of age-related neurodegenerative diseases. The molecular nexopathies paradigm, introduced by Warren and colleagues, proposes that specific pathogenic proteins result in the disintegration of specific neural networks and multiple functional networks, which could give rise to phenotypic variations, as well as overlap between neurodegenerative diseases [4]. A deeper understanding of interlinked and distinctive molecular pathways, which drive pathological and clinical consequences, could provide novel therapeutic strategies. Molecular PET imaging can be employed to investigate known overlapping, and distinct, molecular pathologies and pathways in age-related neurodegenerative diseases (Figure 2). This section highlights novel PET biomarkers targeting mitochondrial dysfunction.

Figure 2. Overview of molecular pathways targeted with PET radioligands. (A) Mitochondrial dysfunction and energy dysregulation can be investigated using (18F)BCPP-EF, for mitochondrial complex 1 and (11C)SA4503 for sigma 1 receptor. (B) Neuroinflammation can be investigated by targeting translator protein expressed in the outer mitochondrial membrane and elevated in activated microglia using PET radioligands such as (11C)PK11195 and astroglia activation using novel PET radioligands such as (11C)BU99008 for imidazoline 2-binding sites expressed in the outer mitochondrial membrane. (C) Abnormal protein aggregation of tau and amyloid-β can be quantified using specific radioligands such as (18F)AV1451 and (18F)Florbetaben, respectively. (D) Synaptic pathology can be investigated using (11C)UCB-J targeting synaptic vesicle glycoprotein 2A. (E) Dysregulation of neurotransmitter systems can be investigated by employing various PET radioligands, including serotonergic markers such as (11C)DASB for the serotonin transporter and dopaminergic markers such as presynaptic markers (18F)DOPA for dopamine storage, (11C)PE2I for dopamine transporter and (11C)Raclopride for postsynaptic dopaminergic receptors, as well as PET radioligands for noradrenergic, glutamatergic and GABAergic systems. Abbreviations: D2R/D3R: Dopamine type-2/type-3 receptor, DAT: Dopamine transporter, DDC: Dopa Decarboxylase, I2BS: Imidazoline 2-binding sites, MC1: Mitochondrial Complex 1, SERT: Serotonin transporter, Sigma 1R: Sigma 1 receptor, SV2A: Synaptic vesicle glycoprotein 2A and TSPO: Translocator protein.
3. Mitochondrial Dysfunction and Energy Dysregulation
There is an increasing body of literature implicating dysfunction of mitochondria and endoplasmic reticulum (ER) dynamics, energy metabolism and oxidative stress within the molecular paradigm of age-related neurodegenerative diseases [24][25][26][27][28][29][24,25,26,27,28,29]. Protein aggregation and deposition have been linked with mitochondrial dysfunction, disrupted mitochondrial transport, dysregulation of adenosine triphosphate (ATP) production, calcium imbalance and oxidative stress [28]. Furthermore, mitochondrial dysfunction can alter the energy supply to synapses, which could drive synaptic disconnection, contributing towards synaptic dysfunction and loss [30][31][30,31]. The identification of several genes, such as PINK-1, Parkin, TREM2, APOE and TOMM40 [32][33][34][35][32,33,34,35], which play key roles in the normal functioning of mitochondria has also highlighted the role of mitochondrial dysfunction in disease pathogenesis [36][37][38][36,37,38]. The temporal sequence of events and the exact interplay between mitochondria and ER dysfunction, oxidative stress, neuroinflammation and protein deposition remains to be fully elucidated. There are lines of evidence to support the accumulation of toxic proteins preceding and triggering mitochondrial and ER dysfunction [39][40][41][39,40,41]. Conversely, other evidence suggests that mitochondrial dysfunction and, consequently, oxidative stress and calcium imbalance, together with dysfunction of the ER, may lead to protein misfolding and the accumulation of toxic protein aggregates [42][43][42,43].
The development of novel PET radioligands, (18F)BCPP-EF, for mitochondrial complex 1 (MC1) and (11C)SA-4503 for sigma 1 receptor (σ1R) enables the in vivo investigation of mitochondrial and ER dysfunction (Figure 2A) in late-onset neurodegenerative and other diseases related to aging [44][45][44,45]. Sigma-1 receptors are expressed at the mitochondrion-associated ER membrane, where they regulate calcium signaling from the ER to the mitochondrion [46][47][48][46,47,48]. Sigma-1 receptors also display neuromodulator and neuroprotective properties, aiding protein folding and modulating synaptic neurotransmitter functions [46][49][50][46,49,50]. MC1 plays a fundamental role in cellular energy production, acting as the first rate limiting step of oxidative phosphorylation in the electron transport chain in mitochondria, as well as maintaining calcium homeostasis and regulating reactive oxygen species (ROS) levels [51][52][51,52]. The altered expression and dysfunction of σ1R and MC1 have been illustrated from post-mortem and preclinical studies in ALS, AD and PD [49][50][53][54][55][56][57][49,50,53,54,55,56,57].
Recently, σ1R and MC1 levels were investigated in a cohort of early de novo PD patients using (11C)SA-4503 and (18F)BCPP-EF PET, respectively [58]. Lower levels of σ1R and MC1 were observed at the baseline, but there were no significant cross sectional or longitudinal changes at 12-months follow-up. In another small cohort of moderate levodopa-treated PD patients, decreased striatal σ1R levels was reported [59][60][59,60], suggesting that the loss of σ1R might be more prominent in moderate-to-advanced disease stages. A combined (18F)BCPP-EF and (11C)PE2I PET preclinical study demonstrated that the striatal loss of MC1 correlated with the loss of presynaptic nigrostriatal dopaminergic neurons, supporting the interplay and colocalization of mitochondrial and synaptic dysfunction in a PD model [61]. Work is ongoing to investigate the role of σ1R and MC1 in AD, ALS, FTD and HD using (11C)SA-4503 and (18F)BCPP-EF PET, respectively, as part of the MIND-MAPS program (https://lp.invicro.com/mind-maps), which could help to provide a more comprehensive understanding of the mitochondrial-ER-synaptic complex, across the spectrum of age-related neurodegenerative diseases. Preliminary work suggests decreased MC1 density in AD [62] [62] and FTD patients [63], with the loss of MC1 associated with global cognitive impairment across cohorts of age-related neurodegenerative cohorts [64]. Furthermore, preliminary findings indicate that σ1R density is increased in early AD, suggesting that this may represent a potential cellular response to stress that could subsequently decrease as the disease progresses [62]. Reduced (18F)BCPP-EF uptake has also been shown to correlate with increase tau deposition, using (11C)PPB3 PET, but not with amyloid-β, using (11C)PiB PET, or glucose metabolism, using (18F)FDG PET [65]. These preliminary findings could indicate that tau pathology precedes early mitochondria-related energy failure. However, these findings need to be further validated in larger, longitudinal studies. The temporal relationship between mitochondrial dysfunction, energy dysregulation and synaptic neuropathology warrants further investigation, as it may play a key role in the development of several age-related neurodegenerative diseases.
There are a number of other PET radioligands with mitochondrial targets. First-, second- and third-generation PET radioligands, such as (11C)PK11195, (11C)PBR28, and (11C)ER176 respectively, commonly employed to study neuroinflammation target the 18-kDa translator protein (TSPO) expressed in the outer mitochondrial membrane and elevated in activated microglia. The novel PET radioligand (11C)BU99008 targets imidazoline 2-binding sites expressed in the outer mitochondrial membrane of activated astrocytes. Furthermore, PET radioligands such as (11C)Harmine and (11C)Deprenyl target mitochondrial monoamine oxidase (MAO)-A and MAO-B, respectively.
