Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Hyun Woo Chung and Version 2 by Lindsay Dong.
The advent of PET/MRI, which combines metabolic PET information with high anatomical detail from MRI, has emerged as a promising tool for breast cancer diagnosis, staging, treatment response assessment, and restaging. Technical advancements including the integration of PET and MRI, considerations in patient preparation, and optimized imaging protocols contribute to the success of dedicated breast and whole-body PET/MRI.
- breast cancer
- PET/MRI
- 8F-FDG PET/CT
1. Introduction
Breast cancer is the cancer with the highest incidence and mortality among women worldwide [1]. Early detection and precise staging are crucial for effective treatment and improved patient outcomes [2]. Mammography, ultrasound (US), and dynamic contrast-enhanced (DCE) magnetic resonance imaging (MRI) are well-established local-regional imaging methods for breast cancer. Bone scintigraphy and 18F-fluorodeoxyglucose positron emission tomography/computed tomography (18F-FDG PET/CT) are also available to evaluate distant metastasis [3].
18F-FDG PET/CT has been widely validated for various cancers, playing an important role in diagnosis, initial staging, therapy response evaluation, and restaging [4]. However, its application for breast cancer in terms of detection, differential diagnosis of benign from malignant lesions, and local tumor staging is not recommended. This is due to its high false-negative rate for small (<1 cm) and low-grade breast cancer, a high false-positive rate for local benign breast disease, and low sensitivity for the detection of axillary lymph node metastasis [5]. Consequently, researchers have explored various novel PET radiotracers targeting molecular factors. Examples include 18F-fluoroestradiol (FES) for estrogen receptor (ER), 89Zr-Df-trastuzumab for human epidermal growth factor receptor-2 (HER2), 68Ga-fibroblast-activation-protein-inhibitor (FAPI) for fibroblast activation protein (FAP), and 18F-fluoromisonidazole (FMISO) for hypoxia. In May 2022, the United States Food and Drug Administration approved 18F-FES for patients with recurrent and metastatic breast cancer, serving as an adjunct to biopsy for detecting ER-positive lesions [3].
PET/MRI, which combines the metabolic information of PET with the high anatomical details of MRI, has been suggested as a promising synergistic imaging modality for cancer. Since MRI is highly sensitive for breast cancer and does not expose the patient to radiation, PET/MRI is under active investigation across the spectrum of diagnosis, staging, treatment response assessment, and restaging of breast cancer [6].
 Currently, ongoing clinical trials are evaluating the axillary staging performance of 18F-FDG PET/MRI compared to sentinel node biopsy (SNB) in both advanced and early breast cancers [18][34]. These trials consist of two prospective comparative single-center studies conducted in different settings. In the first trial (ClinicalTrials.gov Identifier: NCT04826211), the staging performance of 18F-FDG PET/MRI is compared with SNB in patients with breast cancer undergoing primary systemic therapy (PST) for positive axillary lymph nodes at diagnosis. Initial staging and post-PST 18F-FDG PET/MRI results, which are used to plan surgery, will be compared with the results of SNB. In the second trial (ClinicalTrials.gov Identifier: NCT04829643), the axillary staging of 18F-FDG PET/MRI is compared with SNB in patients with early breast cancer undergoing surgery. The results from these trials have the potential to offer patients a less invasive and de-escalated axillary surgery with improved outcomes.
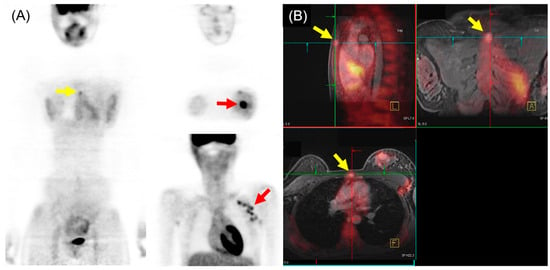
In the comparison of 18F-FDG PET/MRI and 18F-FDG PET/CT for M staging of breast cancer, higher sensitivity and lower specificity of 18F-FDG PET/MRI were generally found, particularly for osseous and/or hepatic metastases [19][36]. Recent meta-analysis, including 16 articles involving 1261 patients, indicated that 18F-FDG PET/MRI showed superior sensitivity and similar specificity to 18F-FDG PET/CT in detecting bone metastases in patients with breast cancer [20][37]. Another meta-analysis with a subgroup using three studies (182 patients) reported that 18F-FDG PET/MRI had higher sensitivity and specificity for detecting distant metastasis of breast cancer than 18F-FDG PET/CT [21][38]. The pooled sensitivity, specificity, and AUC for 18F-FDG PET/MRI were 95%, 96%, and 0.98, respectively. For 18F-FDG PET/CT, the pooled sensitivity, specificity, and AUC were 87%, 94%, and 0.94, respectively. An example of 18F-FDG PET/MRI for initial M staging in a patient with breast cancer is shown in Figure 23.
Currently, ongoing clinical trials are evaluating the axillary staging performance of 18F-FDG PET/MRI compared to sentinel node biopsy (SNB) in both advanced and early breast cancers [18][34]. These trials consist of two prospective comparative single-center studies conducted in different settings. In the first trial (ClinicalTrials.gov Identifier: NCT04826211), the staging performance of 18F-FDG PET/MRI is compared with SNB in patients with breast cancer undergoing primary systemic therapy (PST) for positive axillary lymph nodes at diagnosis. Initial staging and post-PST 18F-FDG PET/MRI results, which are used to plan surgery, will be compared with the results of SNB. In the second trial (ClinicalTrials.gov Identifier: NCT04829643), the axillary staging of 18F-FDG PET/MRI is compared with SNB in patients with early breast cancer undergoing surgery. The results from these trials have the potential to offer patients a less invasive and de-escalated axillary surgery with improved outcomes.
In the comparison of 18F-FDG PET/MRI and 18F-FDG PET/CT for M staging of breast cancer, higher sensitivity and lower specificity of 18F-FDG PET/MRI were generally found, particularly for osseous and/or hepatic metastases [19][36]. Recent meta-analysis, including 16 articles involving 1261 patients, indicated that 18F-FDG PET/MRI showed superior sensitivity and similar specificity to 18F-FDG PET/CT in detecting bone metastases in patients with breast cancer [20][37]. Another meta-analysis with a subgroup using three studies (182 patients) reported that 18F-FDG PET/MRI had higher sensitivity and specificity for detecting distant metastasis of breast cancer than 18F-FDG PET/CT [21][38]. The pooled sensitivity, specificity, and AUC for 18F-FDG PET/MRI were 95%, 96%, and 0.98, respectively. For 18F-FDG PET/CT, the pooled sensitivity, specificity, and AUC were 87%, 94%, and 0.94, respectively. An example of 18F-FDG PET/MRI for initial M staging in a patient with breast cancer is shown in Figure 23.
2. 18F-FDG PET/MRI for Breast Cancer
2.1. Diagnosis
Breast MRI is the most sensitive modality for detecting breast cancer [7][21]. However, the moderately specific nature of breast MRI results in false-positive findings, necessitating additional imaging and biopsy [8][22]. Thus, reducing false-positive findings from breast MRI has significant potential impact by avoiding additional biopsies, reducing cost, decreasing patient anxiety, and minimizing time to surgery. 18F-FDG PET has a limited sensitivity in small breast lesion with both false-negative and false-positive findings as a benign lesion can have an increased uptake. However, the addition of 18F-FDG PET with multiparametric MRI has been suggested to increase the specificity, especially when the size of breast lesions is more than 10 mm [9][23]. Furthermore, the addition of dedicated prone breast PET/MRI to supine whole-body imaging is reported to be more sensitive than whole-body-only supine imaging. In a study involving 38 prospectively enrolled patients with 56 breast cancer lesions, dedicated prone breast 18F-FDG PET/MRI, combined with supine whole-body imaging, correctly identified breast cancers in 97% of cases (37/38). In contrast, supine whole-body-only imaging missed five patients (87%, 33/38) [10][24]. The unidentified patient in dedicated prone breast 18F-FDG PET/MRI had a pT1a tumor measuring 5 mm without radiotracer uptake and considered a benign lesion. The missed five patients in supine whole-body-only 18F-FDG PET/MRI had small lesions ranging from 5 to 13 mm. With recent advances in artificial intelligence (AI) and its applications in medical imaging, Romeo et al. demonstrated that the AI-based radiomics model, with features extracted from simultaneous multiparametric 18F-FDG PET/MRI, achieved high accuracy in discriminating between benign and malignant breast lesions, with an AUC of 0.983 [11][26]. Its sensitivity was not statistically different from the clinical interpretation by experts (100% for AI-based radiomics model vs. 95.3% for clinical interpretation), but specificity was higher for the AI-based radiomics model (94.3% vs. 73.7%, respectively), indicating the potential to decrease false-positive findings in benign breast lesions. While 18F-FDG PET/MRI is not currently recommended for breast cancer diagnosis, its utilization could improve the diagnostic accuracy of MRI and potentially enable a less invasive, comprehensive diagnostic strategy.2.2. Initial Staging
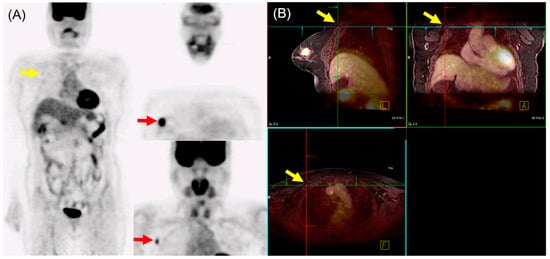
The American Joint Committee on Cancer (AJCC) anatomic TNM staging system for breast cancer includes the extent of the tumor (T), the spread to regional lymph nodes (N), and distant metastasis (M). It emphasizes that comprehensive initial anatomic staging using mammography, US, and MRI is crucial for guiding patient treatment decisions [12][27]. MRI has demonstrated greater accuracy than conventional imaging methods in assessing the extent of breast tumors [13][28]. Consequently, 18F-FDG PET/MRI is proposed to be superior for T-staging compared to conventional mammography, ultrasound (US), and 18F-FDG PET/CT, and is, at the very least, equivalent to breast MRI alone. In a study by Grueneisen et al., involving 49 patients with 83 biopsy-proven invasive breast cancers, mostly at more than T1c stage, no significant difference was observed in correct T-staging between 18F-FDG PET/MRI and MRI. However, both modalities were significantly more accurate than 18F-FDG PET/CT (PET/MRI and MRI, 82%; PET/CT, 68%) [14][29]. In N staging, early studies initially reported the performance of 18F-FDG PET/MRI as either equivalent to or inferior to MRI alone [14][15][29,31]. However, Morawitz et al. demonstrated the diagnostic superiority of 18F-FDG PET/MRI over MRI and CT in determining the regional lymph node status. Their prospective double-center study involved 182 patients with newly diagnosed, treatment-naïve breast cancer [16][32]. 18F-FDG PET/MRI detected significantly more nodal-positive patients than MRI and CT. Moreover, across all lymph node stations (axillary, supraclavicular, and internal mammary stations), 18F-FDG PET/MRI identified significantly more lymph node metastases compared to MRI and CT. Consequently, 18F-FDG PET/MRI resulted in nodal upstaging in 30 patients compared to MRI and in 41 patients compared to CT. No downstaging occurred in 18F-FDG PET/MRI compared to MRI or CT. MRI upstaged nodes in 15 patients and downstaged nodes in 6 patients compared to CT. Additionally, simple imaging features from 18F-FDG PET/MRI and MRI can be utilized for N staging in patients with newly diagnosed breast cancer through machine-learning–based prediction models, exhibiting high accuracy [17][33]. The diagnostic accuracy for MRI features was 87.5% for both the machine-learning algorithm and radiologists. For 18F-FDG PET/MRI, the diagnostic accuracy was 91.2% and 89.3% for the machine-learning algorithm and radiologists, respectively, with no significant difference. An example of 18F-FDG PET/MRI for initial N staging in a patient with breast cancer is shown in Figure 12.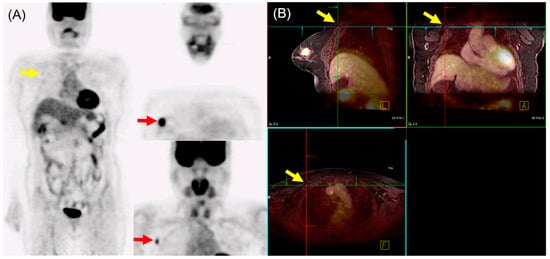
Figure 12. 18F-FDG PET/MRI for initial N staging in a patient with breast cancer. (A) PET images revealed hypermetabolic right breast cancer with right axillary lymph node metastasis (red arrow). Additionally, inconclusive mild hypermetabolic uptake was found in the right interpectoral area (yellow arrow). (B) PET/MRI identified right interpectoral lymph node metastasis with gadolinium-contrast enhancement on T1-w MRI (yellow arrow).
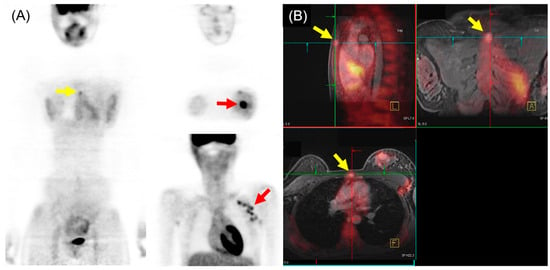
Figure 23. 18F-FDG PET/MRI for initial M staging in a patient with breast cancer. (A) PET images revealed hypermetabolic left breast cancer with left axillary lymph node metastases (red arrow). Additionally, inconclusive mild hypermetabolic uptake was observed in the sternum area (yellow arrow). (B) PET/MRI identified sternum metastasis with gadolinium-contrast enhancement on T1-w MRI (yellow arrow).
