α-linolenic亚麻酸 acid (ALA) belongs to the family of n-3 polyunsaturated fatty acids ((ALA) 属于 n-3 多不饱和脂肪酸 (n-3 PUFAs) and contains a carbon–carbon double bond on the third carbon atom at the methyl end of the carbon chain. This family of essential fatty acids also includes eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). ALA has gradually attracted increased attention due to its nutritional and medicinal advantages. Studies have shown that ALA exerts beneficial effects on a variety of diseases, including cancer.) 家族,在碳链甲基末端的第三个碳原子上含有碳-碳双键。这个必需脂肪酸家族还包括二十碳五烯酸(EPA)和二十二碳六烯酸(DHA)。ALA因其营养和药用优势而逐渐受到越来越多的关注。研究表明,ALA对包括癌症在内的多种疾病都有有益的作用。
1. Introduction
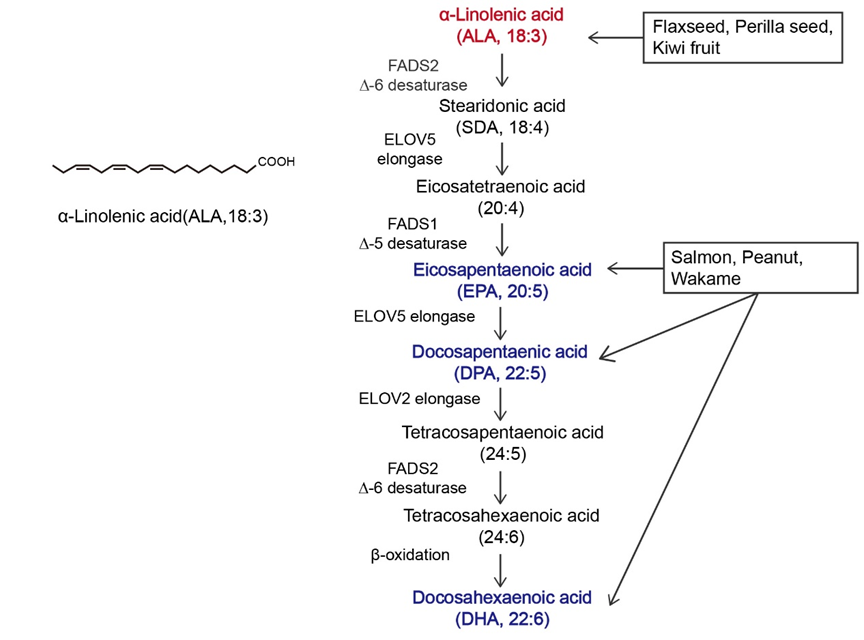
α-linolenic acid (ALA) belongs to the family of n-3 polyunsaturated fatty acids (n-3 PUFAs) and contains a carbon–carbon double bond on the third carbon atom at the methyl end of the carbon chain. This family of essential fatty acids [1] also includes eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). ALA is the synthetic precursor of these factors [2][3]. Studies have shown that ALA, DHA, and EPA can be converted into each other via metabolic pathways, as shown in Figure 1, but this conversion is inefficient [4][5]. In the past, attention to ALA was focused mainly on it as a precursor to DHA and EPA, while little was known about ALA itself [6][7]. The most common way to increase the levels of n-3 PUFAs in the body is through dietary intake. ALA can be acquired through the direct consumption of ALA-rich plants, such as flaxseed, perilla seed, chia seed, and rapeseed [8][9], as well as from various ALA preparations available on the market, such as ALA oil, soft capsules, and microcapsules [10]. As components of the phospholipid membrane [11], n-3 PUFAs play diverse roles, including cardiovascular disease prevention [12], anti-inflammatory effects [13], and anticancer effects [14]. However, the effects of ALA, DHA, and EPA on the human body are not consistent. Hemant Poudyal et al. [15] reported that ALA induced different physiological responses compared to DHA or EPA to alleviate the symptoms of metabolic syndrome. Jeong-Eun C
hoi et al. [16] showed tha
t EPA an
d DHA exerted antidepressant effects on rats, while ALA did not exert antidepressant effects. Laura E Voorrips [17] scer h
owed tha
t ALA was the only n-3 PUFA that was effective at reducing the risk of breast cancer (BC). Based on global medical and nutritional studies [9][18][19][20][21][22][23][24][25][26][27][28][29], ALA cs been a constan
regulat
e blood lipids, reduce blood viscosity, lower blood pressure, support weight loss, suppress allergic reactions, inhibit inflammation, affect diabetes and bone health, and inhibit cancer occurrence and metastasis. Therefore, it is necessary to distinguish ALA from other n-3 PUFAs.
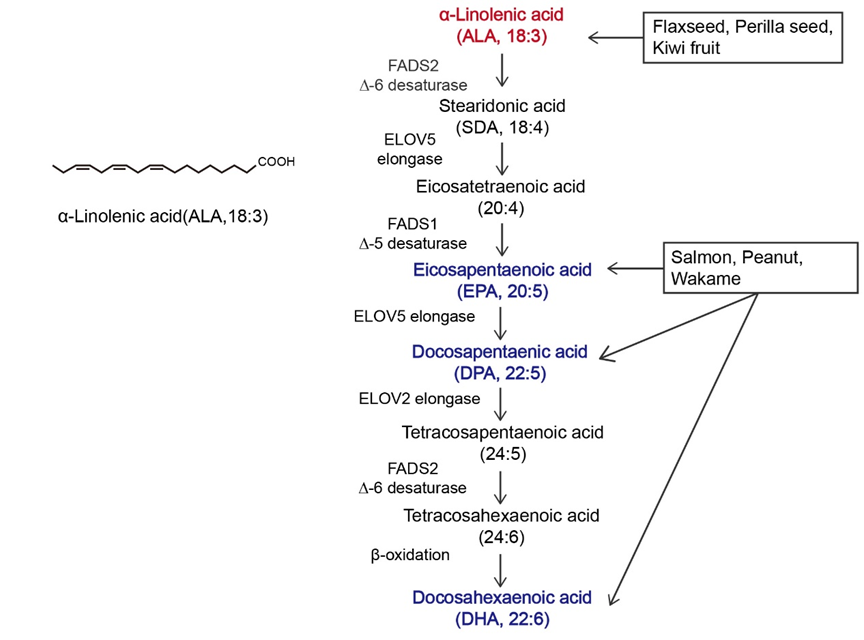
Figure 1.Overview of α-linolenic acid (ALA). Molecular structure of ALA and the in vivo metabolic pathway by which n-3 polyunsaturated fatty acids (n-3 PUFAs) are generated from ALA. The colors in the figure are intended to emphasize the members of n-3 PUFAs. The vertical arrow represents the metabolism of ALA to other n-3 PUFAs in vivo; Arrows in other directions represent different dietary sources of n-3 PUFAs.
According to the International Agency for Research on Cancer GLOBOCAN 2020 cancer incidence and mortality estimates, in 2020, there were 19.3 million new cancer cases and nearly 10 million deaths worldwide [30], except for melanoma cell cancer. As a populous country, China’s new cancer cases in 2020 accounted for 24% of the world’s new cancer cases [31]. Cancer has surpassed cardiovascular disease as the leading cause of death in China. A prominent feature of tumors is that their growth and proliferation are uncontrolled, and invasion and metastasis are the main problems facing current cancer treatment. Although the etiology of cancer is not yet fully understood, it can be roughly divided into two categories, endogenous and exogenous, and nutrients are the factors most closely related to daily life [32]. Nutrient intake can regulate the tumor microenvironment, thereby affecting cancer cell proliferation, apoptosis, and invasion. Current cancer treatment strategies, including surgery, radiotherapy, and chemotherapy, reduce the quality of life of patients, and diet has gradually become one of the most common treatment methods due to its high acceptance by patients and low toxicity and side effects [13][14]. Most of the initial dietary studies focused on limiting the proliferation of tumor cells by reducing the supply of major nutrients to tumors [33][34][35]. With further research, supplementation with specific nutrients, including histidine and mannose, has also become a strategy for the clinical treatment of cancer [36][37].The n-3 PUFA family has attracted considerable attention for its anticancer effects and use as a dietary supplement.
Cancer has been a constant threat to human threat to human life since its identification, and even when it is treatable, it greatly reduces quality of life. Many studies have shown that ALA exerts significant anticancer effects on multiple cancers
[38][39][40][41][42][43][44][45][46][47][48][38,39,40,41,42,43,44,45,46,47,48]. In
Table 1, a subset of ALA-sensitive cancers is listed, including prostate cancer, BC, hepatocellular carcinoma, colorectal cancer (CRC), and pancreatic cancer. In addition, ALA also exerts effects on many common gastrointestinal tumors and bladder cancer
[49][50][51][49,50,51]. As shown in
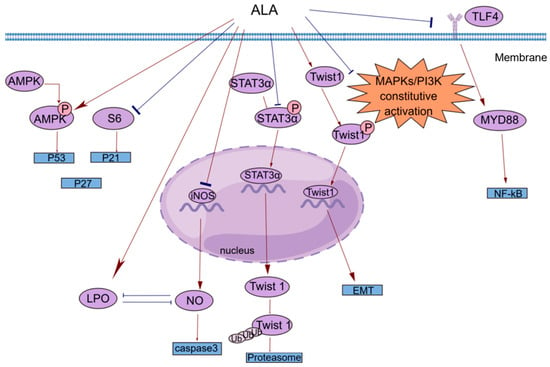
Figure 21, ALA exerts a variety of anticancer effects, including inhibiting proliferation, inducing apoptosis, suppressing tumor metastasis and angiogenesis, and exerting antioxidant effects. To provide a brief introduction to the anticancer effects of ALA, these effects are systematically reviewed, focusing on pharmacological actions and molecular mechanisms.
Figure 21. A brief summary of the molecular mechanism of the anticancer effects of ALA. ALA inhibits cell proliferation by regulating the AMPK/S6 axis. ALA can promote cell apoptosis by directly increasing intracellular lipid peroxidation (LPO) or indirectly reducing the accumulation of NO. ALA can suppress tumor metastasis by decreasing the mRNA expression of Twist1 and promoting the degradation of Twist1. The anti-inflammatory effects of ALA may be mediated by blocking the TLR4/MyD88/NF-κB cascade. This figure was constructed with FigDraw (ID: TOUPR3fbb8). There are two kinds of arrows, the flared arrows represent inhibition, and the other is facilitation.
Table 1.
The mechanism of the antitumor effects of ALA.
| Cancer |
Effect |
Effector Molecules |
Change in Ex-Pression |
PCa
(prostate cancer) [52] |
anti-inflammatory effect |
PG/LTs |
downregulation |
BC
(breast cancer) [38][39][38,39] |
anti-inflammatory effect/inhibition of tumor metastasis |
COX2/PGE2/Twist 1 |
downregulation |
HCC
(hepatocellular carcinoma) [40][41][40,41] |
inhibition of proliferation |
Farnesoid X receptor |
upregulation |
CRC
(colorectal cancer) [42][43][42,43] |
induction of apoptosis |
caspase 3 |
downregulation |
PCA
(pancreatic cancer) [44] |
anti-inflammatory effect |
IL-1β/IL-6 |
downregulation |
2. Inhibition of Proliferation
Cell proliferation plays a key role in life. Normal cell proliferation is critical for organismal growth, development, tissue repair, and metabolism. However, the abnormal expression of cancer-related genes in cells caused by various factors can lead to uncontrolled cell proliferation, which is an important part of cancer development.
Esophageal tumors can lead to dysphagia and strongly affect patient quality of life. In clinical practice, small and localized tumors are often surgically removed, but there is no way to perform surgery on larger or non-localized tumors. In addition, the resistance of esophageal cancer to chemotherapy has made the need for new therapies more urgent. Hyun-Seuk Moon’s team
[53] reported that dietary ALA with or without oleic acid (OA) could inhibit the proliferation of the esophageal cancer cell lines OE19 and OE33 by regulating the AMPK/S6 axis to treat esophageal tumors. OA and ALA promoted the expression of tumor suppressor genes, such as p53, p21, and p27, by activating AMPK and/or decreasing the phosphorylation of S6. This provides a new idea for cancer treatment involving the consumption of ALA-containing foods for therapeutic purposes. Studies have shown that ALA alone or in combination with other drugs can inhibit cell proliferation in a variety of ways. Peroxisome proliferator-activated receptor-γ (PPAR-γ) is a nuclear receptor that regulates lipid homeostasis. As natural ligands of PPAR-γ, fatty acids can inhibit the growth of cancer cells by activating PPAR-γ
[54]. Lijun Yang et al.
[55] reported that ALA dose-dependently inhibited the proliferation of renal cell carcinoma (RCC) cells by significantly increasing PPAR-γ activity and gene expression and significantly inhibiting cyclooxygenase-2 (COX-2). COX-2 is an inducible enzyme involved in inflammation. Moreover, when ALA was combined with the PPAR-γ agonist rosiglitazone and the COX-2 inhibitor N-(3-pyridyl) indomethacinamide, its inhibitory effect on the proliferation of the human RCC cell line OS-RC-2 was further increased. ALA inhibited the transformation of cervical cancer cells by reducing the expression of the human papillomavirus oncoproteins E6 and E7, restoring the expression of the tumor suppressor proteins p53 and Rb, and reducing the expression of phosphorylated ERK1/2 and p38. Thus, cell proliferation was inhibited
[56]. Consequently, it is possible and promising to use ALA in clinical practice to treat associated tumors by preventing tumor cell proliferation.
3. Induction of Apoptosis
Apoptosis is regulated by genes and is a type of programmed cell death. During embryonic development, certain cell populations undergo apoptosis to eliminate certain cells and complete organogenesis. However, mutagenesis by external factors can cause normal cells to become cancerous. The carcinogenesis of normal cells requires uncontrolled cell proliferation, the dysfunction of cell apoptosis, and the dysregulation of apoptotic regulators. In general, cancerous cells escape apoptosis by upregulating antiapoptotic factors and downregulating proapoptotic factors
[57].
Most studies investigating the antiapoptotic effects of n-3 PUFAs have focused on major substances such as EPA and DHA, and little research has been conducted on ALA
[58][59][60][58,59,60]. However, the functions of these substances are different. For example, one prospective study separated DHA, EPA, and ALA and found that ALA was the only n-3 PUFA that significantly reduced BC risk
[17]. Interestingly, this phenomenon of local generalization is not uncommon. Caspases are a class of cysteine proteases that can mediate apoptosis. The apoptotic effect of ALA is closely related to its ability to increase lipid peroxidation
[61][62]. An increase in lipid peroxides may increase the generation of free radicals, and reactive oxygen species (ROS) can directly activate mitochondrial permeability transition, leading to the loss of mitochondrial membrane potential. This results in cytochrome c (cyt c) release and caspase pathway activation. ALA reduced the mRNA expression of inducible nitric oxide synthase (iNOS) to reduce intracellular levels of NO, which can inhibit lipid peroxidation by scavenging free radicals from lipid peroxidation. ALA also inhibited iNOS-induced NO production in a peroxidation-dependent manner, further activating caspase 3 to induce apoptosis
[61][62]. In addition, studies have shown that ALA can promote apoptosis in a variety of ways, such as by upregulating the expression of the proapoptotic gene Bax, downregulating the expression of the antiapoptotic gene Bcl-2, stabilizing hypoxia-inducible factor-1α (HIF-1α) and downregulating fatty acid synthase (FASN) to promote mitochondrial apoptosis
[62][63][63,64]. This opens up multiple possibilities for the clinical use of ALA.
4. Anti-Inflammatory Response
The inflammatory response is a double-edged sword. When the normal balance of the body is disrupted, immune activity is increased and typically manifests as inflammation. However, the existence of inflammation itself and the changes in the microenvironment caused by inflammation cause certain pathological symptoms. Cancer patients are prone to secondary inflammatory diseases, and cancer may also develop in response to inflammation
[64][65][65,66]. For example, patients with inflammatory bowel diseases such as ulcerative colitis and Crohn’s disease have an increased risk of CRC and a higher mortality rate than patients with sporadic CRC
[66][67]. The main reason may be the recurrent chronic inflammatory response, which continuously damages the intestinal mucosa. The mucosa is in a state of long-term repair accompanied by intestinal microbial heterotopia and atypical hyperplasia, which can eventually lead to cancer
[67][68]. ALA has been shown to exert powerful anti-inflammatory effects
[68][69], and different epidemiological studies have shown that ALA is inversely correlated with plasma levels of inflammatory factors, including C-reactive protein (CRP), interleukin-6 (IL-6), interleukin-1β (IL-1β), interferon γ (IFN-γ), tumor necrosis factor-α (TNF-α), and E-selectin
[25][26][25,26]. The potential anti-inflammatory mechanisms of ALA are diverse and include reducing the level of arachidonic acid (AA) in the blood and downregulating COX-2
[69][70].
A common clinical phenomenon in alcoholic hepatitis patients is the leakage of bacterial endotoxins through the damaged intestinal barrier into the portal vein. The endotoxins then bind to lipopolysaccharide-binding protein (LBP), triggering the TLR4/MyD88/NF-κB inflammatory cascade in the liver. ALA can inhibit the lipopolysaccharide (LPS)-induced inflammatory response by blocking this cascade
[70][71]. N-6 polyunsaturated fatty acids, such as linolenic acid (LA), can be metabolized to AA, which is the precursor of many potent proinflammatory mediators, including prostaglandins (PGs) and leukotrienes (LTs)
[71][72]. ALA intake can reduce blood levels of AA because ALA competes with LA for the enzyme delta-6-desaturase. Moreover, ALA is the preferred substrate of this enzyme. Increasing ALA intake can limit the conversion of LA to AA, thereby reducing the biosynthesis of proinflammatory eicosanoid acid and further exerting anticancer effects
[52][72][52,73]. COX-2 enzymes are involved in the synthesis of proinflammatory prostaglandins, and one possible mechanism by which ALA inhibits cancer is that it inhibits inflammation through the downregulation of COX-2
[73][74]. NF-κB plays an important role in the inflammatory and immune responses. COX-2 is a downstream target of NF-κB activation. ALA suppresses tumors by reducing the expression of NF-κB and its target genes in tumor cells
[56].
5. Inhibition of Tumor Metastasis
Tumors can spread in vivo to local normal tissues, to nearby lymph nodes, tissues, and organs, or to distant tissues through fluid transport, which is a feature that has made them a leading cause of cancer-related death
[74][75]. Cancer metastasis can be divided into the following steps: tumor growth in situ, angiogenesis, epithelial–mesenchymal transition (EMT), invasion, intravasation, survival in the blood circulation, extravasation, dormancy, and metastatic tumor growth
[75][76].
In vivo and in vitro experiments have shown that 体内和体外实验表明,ALA
inhibits metastasis in various cancers to varying degrees. 在不同程度上抑制了各种癌症的转移。Marianela Vara-Messler
et al. [76] fed B等[77]以富含AL
B/c mice a chia seed oil diet rich in A
LA and corn oil rich in LA as a control and found that ALA could significantly reduce the incidence of BC and the number of metastatic lesions in mice. Mechanistically, ALA can alter signaling in BC cells by altering the cell membrane structure, which increases fatty acid unsaturation and exerts anticancer effects. In vitro experiments were performed to explore the mechanisms by which ALA inhibits cancer metastasis, including the EMT and tumor angiogenesis. 的奇亚籽油和富含LA的玉米油作为对照,给BALB/c小鼠喂食,发现ALA可显著降低小鼠BC的发病率和转移性病变的数量。从机制上讲,ALA可以通过改变细胞膜结构来改变BC细胞的信号传导,从而增加脂肪酸不饱和度并发挥抗癌作用。通过体外实验探索ALA抑制癌症转移的机制,包括EMT和肿瘤血管生成。Twist1
is required to initiate EMT and promote tumor metastasis and is regulated by signal transducer and activator of transcription 3α (是启动 EMT 和促进肿瘤转移所必需的,并受信号转导和转录 3α 激活因子 (STAT3α
) and mitogen-activated protein kinases (MAPKs). ) 和丝裂原活化蛋白激酶 (MAPK) 的调节。Shih-Chung Wang
et al. [39] studied the effect of 等[39]研究了ALA
on 对Twist1
and 和Twist1
-mediated TNBC cell migration and reported that ALA could reduce the mRNA expression of 介导的TNBC细胞迁移的影响,报道ALA可降低Twist1
, reduce the accumulation of 的mRNA表达,减少STAT3α
in the nucleus, and reduce the protein and phosphorylation levels of 在细胞核中的积累,降低Twist1
. ALA promoted的蛋白和磷酸化水平。ALA 促进 Twist1
degradation, thereby eliminating EMT and inhibiting Twist1-mediated migration in TNBC cells. One of the hallmark features of EMT is the loss of epithelial integrity due to the degradation of adherens junctions, which maintain epithelial cell contacts. A major driver of this degradation is proteolytic digestion by matrix metalloproteinases (MMPs). In tumors, MMP2 and降解,从而消除 EMT 并抑制 TNBC 细胞中 Twist1 介导的迁移。EMT 的标志性特征之一是由于维持上皮细胞接触的粘附连接降解而导致上皮完整性丧失。这种降解的主要驱动因素是基质金属蛋白酶 (MMP) 的蛋白水解消化。在肿瘤中,MMP2 和 MMP9
are involved in connective tissue degradation, tumor-induced angiogenesis, and cell migration. Another mechanism by which ALA inhibits tumor metastasis is by reducing vascular endothelial growth factor (VEGF), MMP-2 and MMP-9 protein expression [56]. As an important vasodilator, 参与结缔组织降解、肿瘤诱导的血管生成和细胞迁移。ALA抑制肿瘤转移的另一种机制是降低血管内皮生长因子(VEGF)、MMP-2和MMP-9蛋白的表达[56]。作为一种重要的血管扩张剂,NO
can stimulate 可以刺激VEGF
production and participate in every step of VEGF-mediated tumor angiogenesis. NO can be generated by the enzyme iNOS in vivo. ALA not only reduces NO levels by reducing the mRNA expression of iNOS but also increases lipid peroxidation. The accumulation of peroxides increases the generation of free radicals; thus, the inactivation and reduction of NO decrease tumor angiogenesis and inhibit tumor metastasis [56][61].
的产生,并参与VEGF介导的肿瘤血管生成的每一步。NO可以由体内iNOS酶产生。ALA不仅通过降低iNOS的mRNA表达来降低NO水平,而且还增加脂质过氧化。过氧化物的积累增加了自由基的产生;因此,NO的灭活和减少可减少肿瘤血管生成并抑制肿瘤转移[56,62]。
6. Antioxidant Effect
抗氧化作用
氧化应激(O
xidative stress (OS
) refers to the breakdown of the balance between ROS production and elimination in the body and is mainly characterized by the excessive production of highly reactive molecules such as ROS and reactive nitrogen species (RNS). OS is closely related to the occurrence and development of tumors [77][78]. )是指体内ROS产生和消除之间平衡的破坏,主要特征是ROS和活性氮(RNS)等高反应性分子的过度产生。OS与肿瘤的发生发展密切相关[78,79]。Rashmi Deshpande
et al. [61]’s study revealed that 等[62]的研究表明,ALA
could inhibit cancer by stimulating 可以通过刺激ROS
production to induce apoptosis. However, this study was performed in a relatively simple in vitro experimental environment, and there are more complex and diverse mechanisms in vivo that can counteract this effect. 产生诱导细胞凋亡来抑制癌症。然而,这项研究是在相对简单的体外实验环境中进行的,体内有更复杂和多样化的机制可以抵消这种影响。Leslie Couedelo
et al. [79] showed that 等[80]表明,ALA
intake induced vitamin 摄入会诱导维生素E
depletion. Since vitamin E is a potent antioxidant, it can be used to capture the free radicals produced without producing OS. In addition, 的消耗。由于维生素E是一种有效的抗氧化剂,因此可用于捕获产生的自由基而不产生OS。此外,Jin Hyang Song
and 和Teruo Miyazawa
reported that excessive incorporation of n报道,在细胞膜中过量掺入n-3 PUFAs
into cell membranes can have adverse effects by enhancing membrane sensitivity to li会增强细胞膜对脂质过氧化(lipid peroxidation
(LPO) and inducing OS, but these studies were based on a high-fat diet [80]. In conclusion, when , LPO)的敏感性并诱导OS,从而产生不良影响,但这些研究是基于高脂肪饮食[81]。总之,当ALA
is added to the diet, its effect on the body as a whole should be considered, and the amount of intake should also be considered.
添加到饮食中时,应考虑其对整个身体的影响,也应考虑摄入量。
亚麻籽油(F
laxseed oil (FO
) is rich in ALA and is often used as a dietary supplement to treat cancer and improve health. )富含ALA,常被用作治疗癌症和改善健康的膳食补充剂。Jyoti Sharma
et al. [81] examined mice with skin cancer induced by 等[82]研究了由7,
12-
dimethylbenzo-[a] thane (DMBA) combined with croton oil and showed that FO scavenged free radicals by increasing the levels of enzymatic and nonenzymatic antioxidants, including superoxide dismutase (SOD), catalase (CAT), glutathione peroxidase (GPx), and glutathione (GSH), in the skin and liver. SOD, CAT, and GPx are important antioxidant enzymes that work in concert to prevent excessive levels of intracellular ROS. The main role of SOD is to accelerate the dismutation of superoxide anions to hydrogen peroxide, after which CAT and GPx convert the resulting hydrogen peroxide into harmless substances [82]. The free radical scavenging effect of 二甲基苯并-[a]烷(DMBA)与巴豆油联合诱导的皮肤癌小鼠,发现FO通过增加皮肤和肝脏中酶和非酶抗氧化剂的水平来清除自由基,包括超氧化物歧化酶(SOD)、过氧化氢酶(CAT)、谷胱甘肽过氧化物酶(GPx)和谷胱甘肽(GSH)。SOD、CAT 和 GPx 是重要的抗氧化酶,它们协同工作以防止细胞内 ROS 水平过高。SOD的主要作用是加速超氧阴离子向过氧化氢的歧化,然后CAT和GPx将产生的过氧化氢转化为无害物质[83]。GSH
is mediated by the active sulfhydryl的自由基清除作用是由其结构中的活性巯基-SH
groups in its structure, which are easily dehydrogenated through oxidation. In addition, GSH can bind to GPx and requires different secondary enzymes and cofactors, including nicotinamide–adenine dinucleotide phosphate (NADPH), to exert its effects [81]. 基团介导的,这些基团容易通过氧化脱氢。此外,GSH可以与GPx结合,需要不同的二级酶和辅因子,包括烟酰胺-腺嘌呤二核苷酸磷酸(NADPH)才能发挥其作用[82]。NADPH
oxidase, which is the major source of 氧化酶是脉管系统中ROS
in the vasculature, is composed of a catalytic subunit and a regulatory cytosolic subunit. 的主要来源,由催化亚基和调节性胞质亚基组成。Hao Han
[83] examined atherosclerosis and showed that [84]对动脉粥样硬化进行了研究,发现FO
could inhibit 可以通过降低NADPH
oxidase by reducing the mRNA and protein expression of the NADPH oxidase catalytic subunit, thereby regulating cytoplasmic subunit expression, reducing malondialdehyde levels and increasing GSH levels to exert antioxidant effects. ALA-rich FO is consumed mainly as a cooking oil, and there is undoubtedly a close association between this nutrient and the gut microbiota. 氧化酶催化亚基的mRNA和蛋白表达来抑制NADPH氧化酶,从而调节细胞质亚基的表达,降低丙二醛水平,增加GSH水平,发挥抗氧化作用。富含ALA的FO主要作为食用油食用,这种营养素与肠道微生物群之间无疑有着密切的联系。Xiaoyan Sun
et al. [84] used an 等[85]采用FO
diet to study the antioxidant capacity of colon epithelial cells in aged rats, and the results showed that the antioxidant levels of aged rats increased significantly after 饮食研究了老年大鼠结肠上皮细胞的抗氧化能力,结果表明,FO
administration. Mechanistically, the intake of FO may have changed some intestinal bacteria. OS can play a role in the entire process of tumor development, and ALA intake can slow the toxic effects on the body when administered at different stages of tumor development.
给药后老年大鼠的抗氧化水平显著增加。从机制上讲,FO的摄入可能改变了一些肠道细菌。OS可以在肿瘤发展的整个过程中发挥作用,在肿瘤发展的不同阶段服用ALA可以减缓对身体的毒性作用。