2. Phosphate Metabolism
2.1. Phosphate Functions
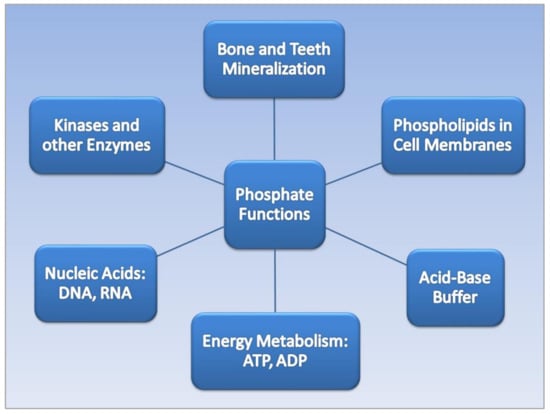
The dietary mineral phosphorus, often found in chemical combination with oxygen as phosphate (PO
4), is an essential micronutrient with a dietary reference intake (DRI) of 700 mg/day for adults
[9][10]. Phosphate performs a wide variety of functions in the human body
[10][11], as shown in
Figure 1. Bones and teeth contain 85% of total body phosphate. Inorganic phosphate (Pi) forms hydroxyapatite with calcium, which mineralizes the extracellular matrix of bone. The lipid bilayers of cell membranes contain phosphate, and phosphate is a component in nucleic acids, deoxyribonucleic acid (DNA), and ribonucleic acid (RNA). Energy is derived from the metabolism of adenosine triphosphate (ATP) and adenosine diphosphate (ADP). Phosphate also acts as a urinary buffer, and many enzymatic reactions involve inorganic phosphate.
Figure 1.
Phosphate functions in the human body.
2.2. Phosphate Regulation and Dysregulation
Serum Pi is regulated by a sensitive network of endocrine hormones that form a bone–kidney–parathyroid–intestine axis, as shown in
Table 1. Ref.
[11][12]. Pi absorption in the intestines occurs mainly through type II sodium-dependent phosphate cotransporters, and intestinal absorption is regulated by bioactive vitamin D3 released by the kidneys, 1,25(OH)
2D
3, or calcitriol. The kidneys regulate serum Pi through reabsorption largely in the renal proximal tubule. Fibroblast growth factor 23 (FGF23) released from osteocytes in the bones, together with parathyroid hormone (PTH) from the parathyroid glands, reduce high serum Pi levels by inhibiting kidney reabsorption of Pi and increasing Pi urinary excretion
[12][13]. PTH also increases the resorption of calcium from bone to maintain serum calcium levels. Excess calcium phosphate formed in the blood serum from dysregulated phosphate metabolism can lead to ectopic calcification deposited throughout the soft tissue
[13][14].
Table 1.
Endocrine Regulation of Serum Pi through the Bone–Kidney–Parathyroid–Intestine Axis.
3. Phosphate Toxicity and Tumorigenesis
Phosphate toxicity, the accumulation of excess phosphate in the body from dysregulated phosphate metabolism, is associated with tumorigenesis
[14][15]. Excessive cell growth during tumor promotion and progression is stimulated by the uptake of excess phosphate into cellular ribosomal RNA, and suppressed uptake of phosphorus within nuclear RNA was shown to delay carcinogenesis in precancerous tissue
[15][16]. High levels of phosphate within the tumor microenvironment have been found to stimulate cell signaling in tumorigenesis
[16][17] and tumor neovascularization
[17][18]. Moreover, high phosphate levels in patients with hyperphosphatemia are associated with chromosome instability and increased parathyroid cell proliferation—further investigations of a direct effect of phosphate on DNA damage are needed
[18][19]. Additionally, high extracellular levels of Pi have been linked to cancer progression through metastasis
[19][20].
Cancer cells absorb and sequester large amounts of inorganic phosphate from the tumor extracellular microenvironment through sodium-phosphate cotransporters, which were overexpressed in cancer cells of the breast, lung, ovaries, and thyroid gland
[20][21][21,22]. Levels of inorganic phosphate were up to twice as high in lung and colon tumor cells compared to normal cells
[22][23], and high dietary phosphate levels were found to increase skin cancer growth in an animal model
[23][24]. As well, lung tumorigenesis was stimulated in mice fed high levels of dietary inorganic phosphate
[16][17]. Cancer in humans was also associated with higher serum phosphate levels in adults, with the exception of reproductive cancers in females, which may be due to phosphate shifting into the reproductive tissue for rapid growth
[24][25][25,26].
More recently, H
+-dependent Pi transporters in breast cancer cells were found to transport high concentrations of Pi at five-times the rate of sodium-phosphate cotransporters
[26][27]. Patients with high levels of FGF23, which regulates Pi metabolism, had reduced overall survival compared to patients with low levels
[27][28], and FGF23 levels were significantly higher in patients with urothelial carcinoma of the bladder and upper urinary tract compared to normal controls
[28][29]. Additionally, compared to men with benign prostate hyperplasia, men with prostate cancer had higher levels of PTH, which also regulates Pi metabolism
[29][30]. High serum PTH levels are associated with all-cause mortality in U.S. adults
[30][31], and patients with primary hyperparathyroidism had significantly higher risks of diagnosis with cancers of the breast, skin, and kidney
[31][32].
4. Phosphate Toxicity and Obesity
The same hormones that regulate phosphate metabolism are also associated with obesity, providing a transitive link between obesity and phosphate toxicity. For example, high serum FGF23 was associated with increased fat mass in a cohort of elderly white people with normal renal function
[32][33]. Participants in the study who had the highest levels of FGF23 also had a significantly higher risk for overweight compared to individuals with the lowest FGF23 levels. A 10% increase in FGF23 in the cohort was associated with a 3% increase in body weight and BMI and a 2% increase in waist circumference (WC) and waist–hip ratio (WHR). Additionally, a 10% increase in FGF23 in males was associated with a 4% increase in total body fat mass and trunk fat mass.
Hyperparathyroidism is commonly found in high-grade obesity, and higher serum levels of PTH were found in 72% of bariatric patients with severe obesity who underwent laparoscopic sleeve gastrectomy (LSG)
[33][34]. Patients’ PTH levels dropped along with BMI following surgery, likely related to a lower caloric density and volume of food intake following LSG
[34][35]. These findings imply that diet is an etiological factor in hyperparathyroidism related to obesity, which provides an additional transitive link between obesity and phosphate toxicity from excessive dietary phosphate intake. Higher concentrations of serum PTH were also positively associated with obesity in females with metabolic abnormalities, while levels of 25(OH)D3, which are converted to calcitriol to increase phosphate absorption in the intestines, were inversely associated with obesity in males with metabolic abnormalities
[35][36].
Obesity is often associated with inadequate intake of micronutrients such as calcium, magnesium, copper, iron, and zinc, but a recent analysis of the US National and Health Nutrition Examination Survey (NHANES) 2007–2014 found that phosphorus dietary intake in adults, along with sodium, was positively associated with BMI
[36][37]. Of relevance, type II sodium-phosphate cotransporters (Na/Pi-2b) and type III inorganic phosphate transporters (Pit-1 and Pit2) are found in the salivary glands, and obese and overweight children were found to have significantly higher saliva levels of phosphate than normal-weight children, despite having normal serum phosphate levels
[37][38]. A plausible mechanism accounting for higher saliva phosphate in obese and overweight children could be related to increased salivary gland cotransport of phosphate from higher levels of ingested dietary phosphate—more investigations are needed in this area.
Hypophosphatemia has also been linked to high BMI, but rather than resulting from low dietary phosphate intake or phosphate losses in urine, low serum phosphate is most frequently caused by a transcellular shift of internal phosphate
[38][39]. Because dietary carbohydrates require phosphorylation of glucose compounds during glycolysis, excessive intake of carbohydrates releases increased levels of insulin which may cause phosphate to shift from extracellular blood serum to liver and skeletal muscle cells during metabolism of a heavy load of sugars
[39][40]. Moreover, abdominal obesity is a part of metabolic syndrome
[40][41], and high serum levels of catecholamines in metabolic syndrome also increase metabolic glycolysis of sugars, which further contributes to a phosphate transcellular shift that lowers serum phosphate levels.
A paradoxical relationship also exists in the association of obesity with a lower risk of breast cancer in premenopausal women compared to postmenopausal women
[41][42]. The mid-luteal phase of the menstrual cycle is when the uterus undergoes growth
[42][43], and women self-reported consuming more animal-based foods during this phase
[43][44]. Animal-based foods contain high levels of protein and phosphorus, which are needed to support the monthly growth of the uterus. The need for more phosphorus during the menstrual cycle could mitigate the risk of phosphate toxicity associated with heavy dietary phosphate intake in obese premenopausal women, which would lower the risk of breast cancer compared to obese postmenopausal women.
Before closing this section on phosphate toxicity and obesity, it should be mentioned that low levels of vitamin D are consistently linked with obesity and with cancer, but researchers found that “the mediating role of vitamin D in the biological pathways linking obesity and cancer is low”
[44][45]. On the other hand, high serum Pi can signal endocrine-controlled reductions in the renal biosynthesis of calcitriol (bioactive vitamin D), thus lowering dietary phosphate intestinal absorption. In other words, low vitamin D appears to be a consequence rather than a cause of dysregulated Pi metabolism in obesity and cancer.