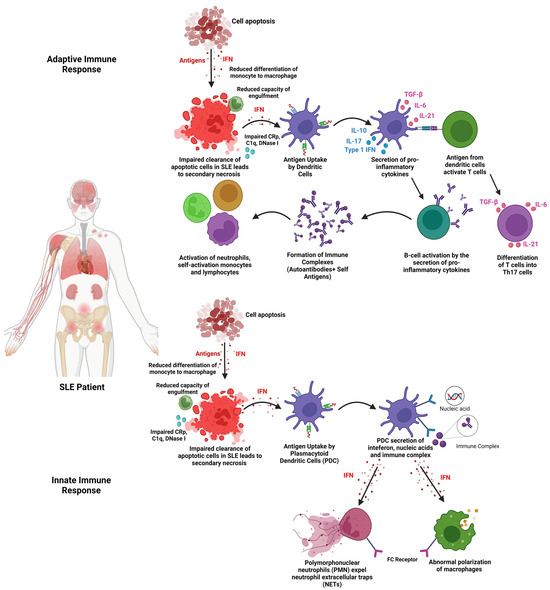
Systemic lupus erythematosus (SLE) is a multisystemic autoimmune disease that affects nearly 3.41 million people globally, with 90% of the cases affecting women of childbearing age. Extracellular vesicles (EVs) can reduce the pro-inflammatory cytokines and increase the anti-inflammatory cytokines. Moreover, EVs can increase the levels of regulatory T cells, thus reducing inflammation. EVs also have the potential to regulate B cells to alleviate SLE and reduce its adverse effects.
- extracellular vesicles (EVs)
- immunomodulation
- inflammation
- mesenchymal stromal cells
- systemic lupus erythematosus (SLE)
- autoimmune
1. Introduction
2. Extracellular Vesicles (EVs)
3. Stem Cell-Derived Extracellular Vesicles in Systemic Lupus Erythematosus
3.1. Isolation of EVs
The isolation method of EVs is crucial to obtain the possible highest purity of EVs to further enhance the specific mechanism of action required [22]. In all the studies, EVs were isolated from the supernatant only after reaching 80–90% confluency of MSCs. The supernatant derived from the conditioned media undergoes centrifugation between 10,000× g and 125,000× g and further undergoes ultracentrifugation at 140,000× g to isolate the EVs based on the size from the precipitate obtained [37][43]. Apart from that, some studies have included EVs that are also isolated from supernatants using super high-speed centrifugation of 175,000× g. There are other studies that have stated the use of only ultracentrifugation between 125,000× g and 140,000× g for the isolation of EVs [1][38][39][40][41][1,44,45,46,47].
3.2. Characterisation of EVs
The isolated EVs are required to be characterised based on their size and specific EV markers to identify the protein expressed by the EVs [37][43]. From the studies, the common characterisation method of EVs is the Western blot assay. The Western blot assay is used to determine specific protein markers related to EVs, which are commonly identified as CD9, CD36, and endoplasmic reticulum-oriented calnexin [37][43]. Other protein markers found in the selected studies that were used to identify and characterise EVs include CD63, Alix, CD81, CD63, GAPDH, and TSG101 [37][38][39][40][41][42][43][44][45][43,44,45,46,47,48,49,50,51]. Characterisation of EVs based on morphology was conducted using a transmission electron microscope and was recorded in a few of the studies. The morphology of EVs that were reported in the studies includes EVs shaped like a saucer, round, or sphere-shaped vesicles that include an entire capsule, bilayer-membrane structure, and a hollow globular vesicle [1][37][38][39][43][45][1,43,44,45,49,51]. Apart from that, most studies included the characterisation of EVs by size, using either a nanoparticle tracking analyser or a particle tracking assay [1][37][38][39][44][1,43,44,45,50]. However, some studies included a different characterisation method to understand the uptake of EVs using the ExoGlow-Protein EV labelling kit-(Green, System Bioscience, Palo Alto, CA, USA) that dyes EVs fluorescent green [45][51]. The study involving SHED-EVs reported a unique characterisation method based on the Ag expression on the surface of the EVs that were analysed using ExoAB Ab kit (System Bioscience, Palo Alto, CA) and R-PE-conjugated anti-rabbit IgG Ab (Cell Signalling Technology, Dancers, MA) using flow cytometry (BD Biosciences) [44][50].3.3. Range of Dose of EVs Administered
To investigate the efficacy of EV treatment for SLE in in vivo models, the dose of EVs required is an important factor that can determine the immunomodulation effects in SLE. In the study of Chen et al. [37][43] and Chen et al. [40][46], the mice were injected with 100 μL of 0.2 mg/mL EVs derived from hUC-MSCs via intravenous injection through the tail vein every 2 days for 14 days. Instead of 2 days, the study carried out by Wei et al. [42][48] reported 2 × 105 cells per 10 g animal weight of ADSC/miR-20a per 150 μL PBS solution weekly for 14 days. Instead of multiple injections of EVs, a study by Sun et al. [41][47] recorded single doses of EVs of 200 μg based on the protein concentration that were administered.3.4. Mechanism of Action (EVs)
3.4.1. Effects of EVs on Pro-Inflammatory Cytokines
The immunomodulatory characteristics of EVs have championed the role of EVs in downregulating disease progression of SLE through various pathways and mechanisms. In terms of macrophage polarisation, in the study by Chen et al. [37][43], EVs derived from hUC-MSCs are involved in decreasing the levels of NOTCH1, IL-1β, and iNOS which are markers indicating activation of the M1 phenotype (pro-inflammatory). Specifically, the iNOS marker was also downregulated when BM-MSC EVs were used [45][51]. The effect of EVs on macrophage polarisation is also proven in the study by Dou et al. [43][49], where EVs derived from human bone marrow mesenchymal stem cells (BM-MSCs) decreased the polarisation of macrophage into the M1 phenotype. The expression of CD80, NOS2, and MCP-1, which are protein expression markers in M1 macrophages, was significantly decreased.3.4.2. Effects of EVs on Anti-Inflammatory Cytokines
Moreover, the EVs played a pivotal role in increasing the CD206, CD86+, CD116+, Arginase-1, and IL-10, which are part of markers indicating M2 macrophage polarisation leading to anti-inflammatory effects [37][40][43,46]. CD206+ and CD163+ markers can also be seen to be upregulated in the study carried out by Sun et al. [41][47] using UC-MSCs to inhibit lupus via M2 macrophage polarisation. The upregulation of Arg-1 markers is also recorded in the study carried out by Zhang et al. [45][51] involving EVs derived from BM-MSCs. The study by Dou et al. [43][49] also recorded an upregulation of CD206, MRC-2, and ARG-1, which are M2 macrophage markers indicating an anti-inflammatory response. Different markers of M2 macrophage, such as CD14+ and CD163+, were alleviated and recorded in the study by Sun et al. [41][47].3.4.3. Effects of EVs on T Cell Lineage
Apart from the secretion of anti-inflammatory and pro-inflammatory cytokines, EVs have proven to be involved in the regulation of Treg and T helper cells to suppress the disease progression of SLE. In the study by Tu et al. [38][44], Th17 subsets were significantly downregulated, showing a reduction in pro-inflammation effects. The cytokine level IL-17 co-relates to the production of Th17 cells. Lower levels of IL-17 indicate lower production of Th17 cells, as IL-17 acts as a biomarker to examine the disease activity in SLE patients [46][54].3.4.4. Effects of EVs on B Cells
Having said that, EVs also have the potential to regulate B cells, which was recorded in the study carried out by Zhao et al. [39][45], which further confirms immunomodulation effects via B cells. EVs have been shown to increase the levels of B cell apoptosis while inhibiting the excessive proliferation of B cells. Cytokine levels further confirmed that the hyperactivation of B cells reduced significantly after the treatment with EVs.3.4.5. Effects of EVs on Lupus Nephritis (c-Complements)
Furthermore, SLE can also lead to complications such as lupus nephritis, which is caused by kidney inflammation. EVs were also reported in various studies, proving to have positive effects by alleviating inflammation and its effects on the kidneys. In the study by Wei et al. [42][48] and Zhang et al. [45][51], levels of IgG and C3, which are immune complexes, were significantly downregulated in the glomerular mesangial and endocapillary of the kidney after the treatment with EVs.3.5. Role of miRNAs and tsRNAs in Extracellular Vesicles in Ameliorating the Disease Progression of SLE
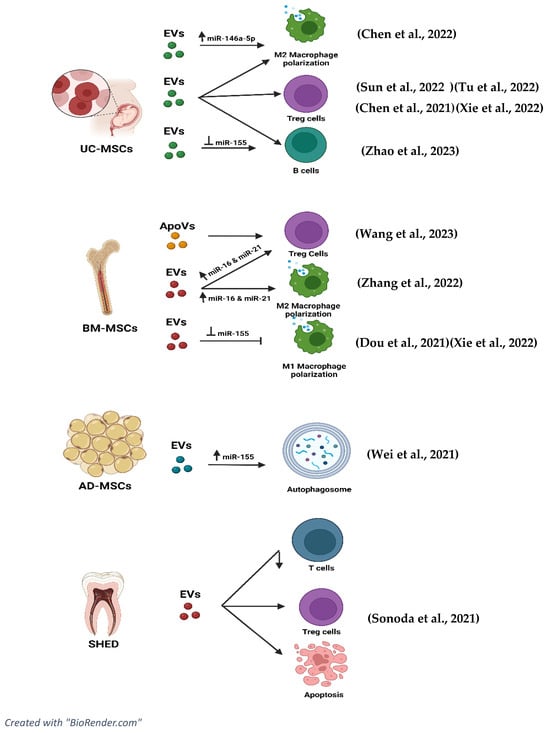
To further improve or understand the immunomodulatory effects of EVs, the effectiveness of inhibition and overexpression of miRNAs related to EVs are included in the studies and shown in Figure 23. The study by Chen et al. [37][43] indicated that the inhibition of miR-146a-5p resulted in adverse effects on lung injuries. NOTCH1, IL-1β, and iNOS were overexpressed while IL-10 and TGF-β levels were downregulated. The inhibition produced a negative effect, thus proving that expression of miR-146a-5p in EVs can upregulate IL-10, CD206, Arg-1, and TGF-β and decrease the expression of NOTCH1, IL-1β, and iNOS in patients diagnosed with SLE.