Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 2 by Rita Xu and Version 1 by Miguel Mascarenhas Saraiva.
In the early 2000s, the introduction of single-camera wireless capsule endoscopy (CE) redefined small bowel study. Progress continued with the development of double-camera devices, first for the colon and rectum, and then, for panenteric assessment. Advancements continued with magnetic capsule endoscopy (MCE), particularly when assisted by a robotic arm, designed to enhance gastric evaluation.
- capsule endoscopy
- panendoscopy
- artificial intelligence
1. Introduction to Panendoscopy and Its Challenges
Capsule endoscopy (CE) is a minimally invasive procedure that was initially conceived for evaluation of the small bowel and has achieved a high diagnostic yield for the detection of small bowel lesions [1]. The notion of a panenteric examination (e.g., for Crohn’s disease assessment) emerged with the development and implementation of colon capsule endoscopy [2]. In fact, since CE allows for the evaluation of the whole gastrointestinal (GI) tract, the concept of a single minimally invasive panendoscopy has become quite a tempting idea [3]. Technical feasibility and expected favorable patient tolerance both support the use of this method. Nevertheless, there are several challenges in implementing it.
Firstly, the implementation of capsule panendoscopy (CPE) would further increase the reading burden of an already time-consuming exam. Without any auxiliary procedural automation, this would most likely reduce the cost-effectiveness of a gastroenterology department, not to mention that many medical institutions would lack the experience or resources required to perform it [4]. More importantly, by considerably increasing the number of frames that must be reviewed, fatigue and monotony levels would increase, potentially leading to missed lesions and/or decisive frames.
Secondly, the diagnostic accuracy of CE in assessing the esophagus and stomach is still suboptimal. In addition to the inability to inflate the lumen, which is an inherent constraint of CE in any anatomical area, there are other limitations that must be considered. In the esophagus, the capsule moves quickly, especially if taken in a sitting/orthostat position, which can reduce the number of mucosal frames and may be associated with incomplete visualization of the Z-line [5]. In the stomach, which is not a cylindric structure as is the case for the small bowel, some areas, particularly proximal ones, may be overlooked, since it is entirely dependent on peristaltic motions, even when dual-headed endoscopic capsules are used [6].
Lastly, while adequate bowel preparation is one of the most important current concerns of capsule enteric evaluation, it becomes much more determinant in the scenario of CPE. In fact, wresearchers have yet to find an effective and reproducible method of bowel preparation that is widely accepted and tolerated by patients, not only for small bowel CE, but also for colon CE [7]. Even though numerous studies have been conducted in this domain, including systematic reviews with meta-analysis, it remains challenging to reach a final conclusion due to heterogeneity in how researchers analyze mucosa cleansing [8,9][8][9]. There is currently no method that fulfils the criteria of the method being non-time-consuming, consistent, and free of inter-observer variability. Neither the development of operator-dependent nor color-intensity-based automated methods have fully addressed this issue [7,8,9][7][8][9]. The development of a standardized method and its integration in CE reading tools most likely needs to be the former step, thus facilitating the subsequent design of an appropriate clinical trial to determine the most beneficial preparation.
2. Wireless Capsule Endoscopy: A Pill-Sized Revolution in Gastrointestinal Imaging
Single-camera capsules were the first to be developed in the early 2000s, initially with lower resolution and a lower capturing frame rate [1]. Over time, improvements were made, including to the camara resolution capturing frame rate and battery power, and software refinement as well as hardware advancements took place with the introduction of real-time viewers [10]. The progress eventually led to development of adaptative frame rate technology, where the faster the capsule progresses, the higher the capture rate, reaching a maximum of six frames per second [10].
Dual-camera capsules were introduced in 2006 [2]. First-generation designs went into sleep mode shortly after ingestion due to power saving issues, rewiring only in the small bowel. The capturing frame rate was poor, resulting in a lower sensitivity in detecting polyps, compared to second-generation models [2,11][2][11]. These later devices became accessible later in 2009, offered a wider view angle and came with an adaptative frame rate up to 35 frames per second, which was a valuable inclusion to preserve battery [11]. More recently, in 2016, a third-generation design was introduced which was able to stay operational without interruption along the entire GI tract [12]. Initially it was intended to assess inflammatory bowel disease patients more accurately, but it rapidly prompted discussions of CPE.
Since its introduction, CE has established itself as the first-line method for assessing the small bowel mucosa. The two main indications for its usage include suspected mid-gastrointestinal bleeding and diagnosis/follow-up in situations of suspected/confirmed small bowel Crohn’s disease [13]. Moreover, it can also be used to monitor hereditary polyposis syndromes, mainly Peutz–Jeghers, and to rule out small intestine tumors [13]. It is also applicable to the evaluation of nonresponsive or refractory celiac disease cases, when the diagnosis of celiac disease is uncertain, or in malabsorption syndromes [13]. Additionally, dual-camera capsules have improved the visualization of the colonic mucosa, by enabling greater visibility of both haustra and areas located behind folds [11]. As a result, they have improved capsules’ overall diagnostic yield, not only for detecting protuberant lesions, but also for other mucosal lesions [11]. Consequently, this has become a possible alternative method for colorectal cancer (CCR) screening, mostly in situations where prior colonoscopy was incomplete or there was a greater risk of complications or contraindication to conventional colonoscopy or sedation [14,15,16][14][15][16].
CE is generally safe and well tolerated, with few contraindications. Caution is warranted in patients with swallowing disorders, due to risk of aspiration [17]. Additionally, it requires clinical assessment of the risk of capsule retention [13,18][13][18]. This is particularly applicable for patients with established Crohn’s disease (ECD), where the risk of retention is increased, and whenever obstructive symptoms are observed [13,19][13][19]. Given the high risk of CE retention in Crohn’s disease, the inability to distinguish high-risk from low-risk patients based on clinical presentation alone, and the indisputable effectiveness of patency testing, the safest approach would be to pursue patency testing before CE in all ECD patients [13,19,20][13][19][20]. Moreover, there is also an increased risk of retention in patients with previous gastrointestinal surgery or radiation therapy of the abdomen and pelvis, as well as persistent users of non-steroid anti-inflammatories and patients with a personal history of small bowel tumors [17]. In these cases, a patency capsule might also be considered [17,21][17][21]. The use of CE in individuals with implantable cardiac devices (pacemaker, defibrillators and left ventricular assist devices) should not be contraindicated, since several studies have shown that is safe [22].
3. Robotic-Assisted Panendoscopy: Advancements and Benefits
In addition to wireless CE, magnetically controlled capsule endoscopy (MCE) has emerged as an alternative method to evaluate the superior GI tract (Figure 1) [23]. In this case, the capsule contains a magnet that can be moved in real time by a magnetic field that is generated outside the patient after swallowing it, using forces of translation and rotation [24].
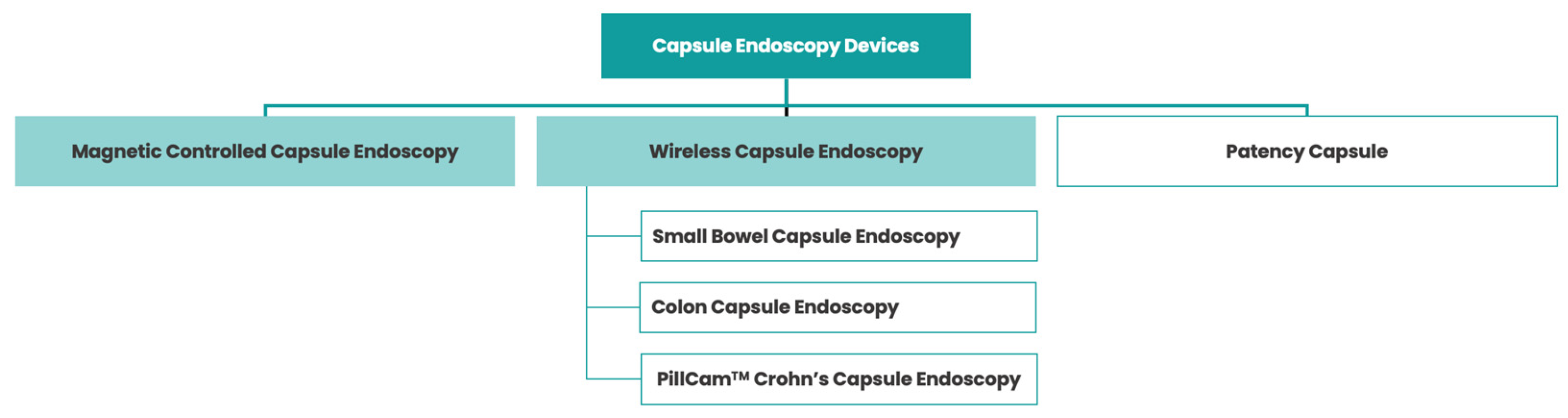
Figure 1. Various types of capsule endoscopy devices.
There are three types of magnetic control systems: hand-held magnets, electromagnetic coil systems (comparable to present-day MRIs) and robotic arms [25,26,27,28][25][26][27][28]. Of these techniques confined to very few centers, the latter is the most widely used and studied, mainly for the assessment of the gastric mucosa, given its operability (either manually or automatically), tolerability (the exam is conducted without patient movement) and ease of installation (compared to the installation of larger electromagnetic coil systems) [23].
The development and implementation of MCE for gastric assessment addresses one of the shortcomings of wireless CE by not depending entirely on stomach peristalsis to move. Although the protocol is not fully established, patients are typically asked to drink 1 L of water (generally mixed with an anti-foaming agent) 10 min prior to the start of the exam, to enhance gastric distention [28]. Then, the capsule is mobilized through this water interface, enabling evaluation of the gastric mucosa. In fact, there is some evidence that shows that MCE’s diagnostic accuracy for detecting gastric lesions might be comparable to the gold standard upper endoscopy, with superior overall agreement in 90% of cases [27]. This, in turn, may serve as a safe and effective alternative for gastric assessment, besides wireless CE, in patients who cannot tolerate esophagogastroduodenoscopy.
Furthermore, the implementation of MCE controlled by a robotic arm could also contribute to panendoscopic evaluation of the whole GI tract. For example, a patient could ingest the capsule lying down (to maximize the assessment of the esophageal mucosa), followed by an extensive evaluation protocol of the stomach with the help of magnetic fields [28]. Then, when the capsule enters the duodenum, the patient would be able to leave the examination bed and move as in wireless CE, allowing for the remaining panenteric assessment.
When it comes to contraindications, they are similar to those outlined previously in wireless CE. The presence of a magnetic field adds extra contraindications, comparable to those applied to MRI, namely the presence of implanted electronic devices, non-MRI-compatible pacemakers and/or magnetic metal foreign bodies [28].
From a diagnostic standpoint, it should be highlighted that MCE’s ability to evaluate the fundus is still incomplete, with some studies reporting impossibility in 20% of instances [29]. Furthermore, thus far, it is challenging to compare wireless CE and MCE, given the lack of comparative research between them.
4. Artificial Intelligence in Panendoscopy: Enhancing Diagnostic Accuracy
In recent years, artificial intelligence (AI) has gained relevance in diverse fields of medical practice, particularly is specialties with a strong imaging and diagnostic component [30]. Gastroenterology has always been marked by ground-breaking achievements, using highly innovative technologies to improve patient care. As a result, it is not surprising that it is also leading the way in the advancement of AI technologies in healthcare.
AI-related developments have been achieved in two areas of computational science over the previous decade: machine learning (ML) and deep learning (DL). These two fields emerged around the same period. However, the lack of adequate computational power in the past limited the widespread adoption of DL models. As a result, technology initially embraced ML algorithms. Their aim was to complete a task by analyzing patterns automatically. Nevertheless, ML requires a supervised phase to ensure proper data annotation [31].
With the current availability of ample computational resources, DL models have gained significant momentum in recent years. These models are a subset of machine learning that are also used for automatic pattern identification but, unlike the former, do not necessarily require human interaction to train the model, displaying supervised or unsupervised learning potential [32,33][32][33]. They involve neural networks with multiple layers (three or more), structured in a hierarchical human-brain-inspired architecture, which is capable of performing more complicated tasks by sequentially combining inputs from various layers ranging from lower-level to higher-levels ones [34]. One DL model example is a convolutional neural network (CNN), which, as the name suggests, has a multilayer neural network structure that is used to automatically analyze complex visual data, mimicking the neurobiological process [35].
There are some ML-based capsule software add-ons which assist the gastroenterologist in image-pattern analysis. They were developed for many purposes, including color image analysis (e.g., automatically detecting blood, as in PillCam’s Suspected Blood Indicator), topographic segmentation (e.g., automatically recognizing distinct anatomical sections) and video adjustment (e.g., reducing duration of a video by displaying frames with the highest probability of being abnormal, as in PillCam’s Top 100) [36]. These tools helped to reduce the reading burden, although the percentage of missing lesions is higher compared to that in developed DL models [37]. Therefore, there has been exponential interest in the development and validation of DL models for CE.
Convolutional neural networks were initially developed using frames from a single-camera capsules, later expanding to dual-camera capsules. Specific CNNs were applied first in the small bowel, followed by the colon and rectum, and then, in both anatomical regions, excelling at detecting a particular lesion [37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54][37][38][39][40][41][42][43][44][45][46][47][48][49][50][51][52][53][54]. Nevertheless, adopting a sequential approach where each specific CNN is applied one at a time for an AI-assisted review of a CE video, while logical, might not be the most efficient strategy.
Complex CNNs have started to emerge, offering the capability of detecting multiple types of lesions at once [55,56,57,58,59][55][56][57][58][59]. The first paper in this field was published by Ding et al. and demonstrates the potential of a CNN-based approach to assisting in the reading of wireless CE. Indeed, their AI system provides the simultaneous detection of a wide range of lesions. Despite the novelty of being the first published complex model, the findings of this study are currently a topic of debate, as this CNN can accurately detect various types of lesions but fails to differentiate between them [55]. The CNN described in that study serves as the core technology for the newly developed DL solution (ProScan™, AnX Robotica, Plano, TX, USA) to be incorporated into the reading software of the NaviCam SB system (AnX Robotic Corp, Plano, TX, USA). Although the hardware has received clearance by the Food and Drug Administration (FDA), this clearance has not been granted for ProScan™, which currently awaits approval for commercial use. Other groups have also developed DL models which are most often used in the small bowel, but are also capable of being used in the colon [56,57,58,59][56][57][58][59].
From panenteric AI-enhanced mucosa evaluation, some groups have also tried to develop DL solutions for assessing the stomach. First, they used MCE capsules [60,61][60][61]. Then, there was also a published CNN that used various types of wireless CE capsules, representing another important step for pursuing the AI-enhanced panendoscopy vision [62].
The technological readiness level of these algorithms in CE is currently situated in the initial stages of development, spanning from experimental to demonstration pilots, with some still in the research phase focused on concept validation. To fully understand the potential of AI during CE, prospective and multicentric studies are still required since most research conducted so far has been retrospective. The role of this DL-based technology in the identification of esophageal lesions by CE is still to be explored. CE is associated with a scarcity of esophagus images, which limits the establishment of esophageal-only databases. Nevertheless, the development of these types of models may be a pivotal step towards minimally invasive AI-enhanced CPE.
References
- Iddan, G.; Meron, G.; Glukhovsky, A.; Swain, P. Wireless capsule endoscopy. Nature 2000, 405, 417.
- Eliakim, R.; Fireman, Z.; Gralnek, I.M.; Yassin, K.; Waterman, M.; Kopelman, Y.; Lachter, J.; Koslowsky, B.; Adler, S.N. Evaluation of the PillCam Colon capsule in the detection of colonic pathology: Results of the first multicenter, prospective, comparative study. Endoscopy 2006, 38, 963–970.
- Eliakim, R.; Adler, S.N. Colon PillCam: Why not just take a pill? Dig. Dis. Sci. 2015, 60, 660–663.
- Piccirelli, S.; Mussetto, A.; Bellumat, A.; Cannizzaro, R.; Pennazio, M.; Pezzoli, A.; Bizzotto, A.; Fusetti, N.; Valiante, F.; Hassan, C.; et al. New Generation Express View: An Artificial Intelligence Software Effectively Reduces Capsule Endoscopy Reading Times. Diagnostics 2022, 12, 1783.
- Park, J.; Cho, Y.K.; Kim, J.H. Current and Future Use of Esophageal Capsule Endoscopy. Clin. Endosc. 2018, 51, 317–322.
- Kim, J.H.; Nam, S.J. Capsule Endoscopy for Gastric Evaluation. Diagnostics 2021, 11, 1792.
- Spada, C.; McNamara, D.; Despott, E.J.; Adler, S.; Cash, B.D.; Fernández-Urién, I.; Ivekovic, H.; Keuchel, M.; McAlindon, M.; Saurin, J.C.; et al. Performance measures for small-bowel endoscopy: A European Society of Gastrointestinal Endoscopy (ESGE) Quality Improvement Initiative. United Eur. Gastroenterol. J. 2019, 7, 614–641.
- Tabone, T.; Koulaouzidis, A.; Ellul, P. Scoring Systems for Clinical Colon Capsule Endoscopy-All You Need to Know. J. Clin. Med. 2021, 10, 2372.
- Rosa, B.; Margalit-Yehuda, R.; Gatt, K.; Sciberras, M.; Girelli, C.; Saurin, J.C.; Valdivia, P.C.; Cotter, J.; Eliakim, R.; Caprioli, F.; et al. Scoring systems in clinical small-bowel capsule endoscopy: All you need to know! Endosc. Int. Open 2021, 9, E802–E823.
- Cortegoso Valdivia, P.; Pennazio, M. Chapter 2—Wireless capsule endoscopy: Concept and modalities. In Artificial Intelligence in Capsule Endoscopy; Mascarenhas, M., Cardoso, H., Macedo, G., Eds.; Academic Press: Cambridge, MA, USA, 2023; pp. 11–20.
- Eliakim, R.; Yassin, K.; Niv, Y.; Metzger, Y.; Lachter, J.; Gal, E.; Sapoznikov, B.; Konikoff, F.; Leichtmann, G.; Fireman, Z.; et al. Prospective multicenter performance evaluation of the second-generation colon capsule compared with colonoscopy. Endoscopy 2009, 41, 1026–1031.
- Tontini, G.E.; Rizzello, F.; Cavallaro, F.; Bonitta, G.; Gelli, D.; Pastorelli, L.; Salice, M.; Vecchi, M.; Gionchetti, P.; Calabrese, C. Usefulness of panoramic 344°-viewing in Crohn’s disease capsule endoscopy: A proof of concept pilot study with the novel PillCam™ Crohn’s system. BMC Gastroenterol. 2020, 20, 97.
- Pennazio, M.; Rondonotti, E.; Despott, E.J.; Dray, X.; Keuchel, M.; Moreels, T.; Sanders, D.S.; Spada, C.; Carretero, C.; Cortegoso Valdivia, P.; et al. Small-bowel capsule endoscopy and device-assisted enteroscopy for diagnosis and treatment of small-bowel disorders: European Society of Gastrointestinal Endoscopy (ESGE) Guideline—Update 2022. Endoscopy 2023, 55, 58–95.
- Vuik, F.E.R.; Nieuwenburg, S.A.V.; Moen, S.; Spada, C.; Senore, C.; Hassan, C.; Pennazio, M.; Rondonotti, E.; Pecere, S.; Kuipers, E.J.; et al. Colon capsule endoscopy in colorectal cancer screening: A systematic review. Endoscopy 2021, 53, 815–824.
- Kjølhede, T.; Ølholm, A.M.; Kaalby, L.; Kidholm, K.; Qvist, N.; Baatrup, G. Diagnostic accuracy of capsule endoscopy compared with colonoscopy for polyp detection: Systematic review and meta-analyses. Endoscopy 2021, 53, 713–721.
- Möllers, T.; Schwab, M.; Gildein, L.; Hoffmeister, M.; Albert, J.; Brenner, H.; Jäger, S. Second-generation colon capsule endoscopy for detection of colorectal polyps: Systematic review and meta-analysis of clinical trials. Endosc. Int. Open 2021, 9, E562–E571.
- Nakamura, M.; Kawashima, H.; Ishigami, M.; Fujishiro, M. Indications and Limitations Associated with the Patency Capsule Prior to Capsule Endoscopy. Intern. Med. 2022, 61, 5–13.
- Garrido, I.; Andrade, P.; Lopes, S.; Macedo, G. Chapter 5—The role of capsule endoscopy in diagnosis and clinical management of inflammatory bowel disease. In Artificial Intelligence in Capsule Endoscopy; Mascarenhas, M., Cardoso, H., Macedo, G., Eds.; Academic Press: Cambridge, MA, USA, 2023; pp. 69–90.
- Pasha, S.F.; Pennazio, M.; Rondonotti, E.; Wolf, D.; Buras, M.R.; Albert, J.G.; Cohen, S.A.; Cotter, J.; D’Haens, G.; Eliakim, R.; et al. Capsule Retention in Crohn’s Disease: A Meta-analysis. Inflamm. Bowel Dis. 2020, 26, 33–42.
- Silva, M.; Cardoso, H.; Macedo, G. Patency Capsule Safety in Crohn’s Disease. J. Crohn’s Colitis 2017, 11, 1288.
- Rondonotti, E.; Spada, C.; Adler, S.; May, A.; Despott, E.J.; Koulaouzidis, A.; Panter, S.; Domagk, D.; Fernandez-Urien, I.; Rahmi, G.; et al. Small-bowel capsule endoscopy and device-assisted enteroscopy for diagnosis and treatment of small-bowel disorders: European Society of Gastrointestinal Endoscopy (ESGE) Technical Review. Endoscopy 2018, 50, 423–446.
- Tabet, R.; Nassani, N.; Karam, B.; Shammaa, Y.; Akhrass, P.; Deeb, L. Pooled Analysis of the Efficacy and Safety of Video Capsule Endoscopy in Patients with Implantable Cardiac Devices. Can. J. Gastroenterol. Hepatol. 2019, 2019, 3953807.
- Liao, Z.; Zou, W.; Li, Z.S. Clinical application of magnetically controlled capsule gastroscopy in gastric disease diagnosis: Recent advances. Sci. China Life Sci. 2018, 61, 1304–1309.
- Shamsudhin, N.; Zverev, V.I.; Keller, H.; Pane, S.; Egolf, P.W.; Nelson, B.J.; Tishin, A.M. Magnetically guided capsule endoscopy. Med. Phys. 2017, 44, e91–e111.
- Swain, P.; Toor, A.; Volke, F.; Keller, J.; Gerber, J.; Rabinovitz, E.; Rothstein, R.I. Remote magnetic manipulation of a wireless capsule endoscope in the esophagus and stomach of humans (with videos). Gastrointest. Endosc. 2010, 71, 1290–1293.
- Rahman, I.; Afzal, N.A.; Patel, P. The role of magnetic assisted capsule endoscopy (MACE) to aid visualisation in the upper GI tract. Comput. Biol. Med. 2015, 65, 359–363.
- Liao, Z.; Hou, X.; Lin-Hu, E.Q.; Sheng, J.Q.; Ge, Z.Z.; Jiang, B.; Hou, X.H.; Liu, J.Y.; Li, Z.; Huang, Q.Y.; et al. Accuracy of Magnetically Controlled Capsule Endoscopy, Compared With Conventional Gastroscopy, in Detection of Gastric Diseases. Clin. Gastroenterol. Hepatol. 2016, 14, 1266–1273.e1.
- He, C.; Wang, Q.; Jiang, X.; Jiang, B.; Qian, Y.-Y.; Pan, J.; Liao, Z. Chapter 13—Magnetic capsule endoscopy: Concept and application of artificial intelligence. In Artificial Intelligence in Capsule Endoscopy; Mascarenhas, M., Cardoso, H., Macedo, G., Eds.; Academic Press: Cambridge, MA, USA, 2023; pp. 217–241.
- Liao, Z.; Duan, X.D.; Xin, L.; Bo, L.M.; Wang, X.H.; Xiao, G.H.; Hu, L.H.; Zhuang, S.L.; Li, Z.S. Feasibility and safety of magnetic-controlled capsule endoscopy system in examination of human stomach: A pilot study in healthy volunteers. J. Interv. Gastroenterol. 2012, 2, 155–160.
- Currie, G.; Hawk, K.E.; Rohren, E.; Vial, A.; Klein, R. Machine Learning and Deep Learning in Medical Imaging: Intelligent Imaging. J. Med. Imaging Radiat. Sci. 2019, 50, 477–487.
- Handelman, G.S.; Kok, H.K.; Chandra, R.V.; Razavi, A.H.; Lee, M.J.; Asadi, H. eDoctor: Machine learning and the future of medicine. J. Intern. Med. 2018, 284, 603–619.
- Kim, J.; Kim, J.; Jang, G.J.; Lee, M. Fast learning method for convolutional neural networks using extreme learning machine and its application to lane detection. Neural Netw. 2017, 87, 109–121.
- Afonso, J.; Martins, M.; Ferreira, J.; Mascarenhas, M. Chapter 1—Artificial intelligence: Machine learning, deep learning, and applications in gastrointestinal endoscopy. In Artificial Intelligence in Capsule Endoscopy; Mascarenhas, M., Cardoso, H., Macedo, G., Eds.; Academic Press: Cambridge, MA, USA, 2023; pp. 1–10.
- Amisha; Malik, P.; Pathania, M.; Rathaur, V.K. Overview of artificial intelligence in medicine. J. Family Med. Prim. Care 2019, 8, 2328–2331.
- Li, N.; Zhao, X.; Yang, Y.; Zou, X. Objects Classification by Learning-Based Visual Saliency Model and Convolutional Neural Network. Comput. Intell. Neurosci. 2016, 2016, 7942501.
- Fisher, M.; Mackiewicz, M. Colour Image Analysis of Wireless Capsule Endoscopy Video: A Review. In Color Medical Image Analysis; Celebi, M.E., Schaefer, G., Eds.; Springer: Dordrecht, The Netherlands, 2013; pp. 129–144.
- Aoki, T.; Yamada, A.; Kato, Y.; Saito, H.; Tsuboi, A.; Nakada, A.; Niikura, R.; Fujishiro, M.; Oka, S.; Ishihara, S.; et al. Automatic detection of blood content in capsule endoscopy images based on a deep convolutional neural network. J. Gastroenterol. Hepatol. 2020, 35, 1196–1200.
- Afonso, J.; Saraiva, M.M.; Ferreira, J.P.S.; Ribeiro, T.; Cardoso, H.; Macedo, G. Performance of a convolutional neural network for automatic detection of blood and hematic residues in small bowel lumen. Dig. Liver Dis. 2021, 53, 654–657.
- Leenhardt, R.; Vasseur, P.; Li, C.; Saurin, J.C.; Rahmi, G.; Cholet, F.; Becq, A.; Marteau, P.; Histace, A.; Dray, X. A neural network algorithm for detection of GI angiectasia during small-bowel capsule endoscopy. Gastrointest. Endosc. 2019, 89, 189–194.
- Tsuboi, A.; Oka, S.; Aoyama, K.; Saito, H.; Aoki, T.; Yamada, A.; Matsuda, T.; Fujishiro, M.; Ishihara, S.; Nakahori, M.; et al. Artificial intelligence using a convolutional neural network for automatic detection of small-bowel angioectasia in capsule endoscopy images. Dig. Endosc. 2020, 32, 382–390.
- Houdeville, C.; Souchaud, M.; Leenhardt, R.; Beaumont, H.; Benamouzig, R.; McAlindon, M.; Grimbert, S.; Lamarque, D.; Makins, R.; Saurin, J.C.; et al. A multisystem-compatible deep learning-based algorithm for detection and characterization of angiectasias in small-bowel capsule endoscopy. A proof-of-concept study. Dig. Liver Dis. 2021, 53, 1627–1631.
- Ribeiro, T.; Saraiva, M.M.; Ferreira, J.P.S.; Cardoso, H.; Afonso, J.; Andrade, P.; Parente, M.; Jorge, R.N.; Macedo, G. Artificial intelligence and capsule endoscopy: Automatic detection of vascular lesions using a convolutional neural network. Ann. Gastroenterol. 2021, 34, 820–828.
- Aoki, T.; Yamada, A.; Aoyama, K.; Saito, H.; Tsuboi, A.; Nakada, A.; Niikura, R.; Fujishiro, M.; Oka, S.; Ishihara, S.; et al. Automatic detection of erosions and ulcerations in wireless capsule endoscopy images based on a deep convolutional neural network. Gastrointest. Endosc. 2019, 89, 357–363.e2.
- Klang, E.; Barash, Y.; Margalit, R.Y.; Soffer, S.; Shimon, O.; Albshesh, A.; Ben-Horin, S.; Amitai, M.M.; Eliakim, R.; Kopylov, U. Deep learning algorithms for automated detection of Crohn’s disease ulcers by video capsule endoscopy. Gastrointest. Endosc. 2020, 91, 606–613.e2.
- Barash, Y.; Azaria, L.; Soffer, S.; Margalit Yehuda, R.; Shlomi, O.; Ben-Horin, S.; Eliakim, R.; Klang, E.; Kopylov, U. Ulcer severity grading in video capsule images of patients with Crohn’s disease: An ordinal neural network solution. Gastrointest. Endosc. 2021, 93, 187–192.
- Afonso, J.; Saraiva, M.J.M.; Ferreira, J.P.S.; Cardoso, H.; Ribeiro, T.; Andrade, P.; Parente, M.; Jorge, R.N.; Saraiva, M.M.; Macedo, G. Development of a Convolutional Neural Network for Detection of Erosions and Ulcers With Distinct Bleeding Potential in Capsule Endoscopy. Tech. Innov. Gastrointest. Endosc. 2021, 23, 291–296.
- Saito, H.; Aoki, T.; Aoyama, K.; Kato, Y.; Tsuboi, A.; Yamada, A.; Fujishiro, M.; Oka, S.; Ishihara, S.; Matsuda, T.; et al. Automatic detection and classification of protruding lesions in wireless capsule endoscopy images based on a deep convolutional neural network. Gastrointest. Endosc. 2020, 92, 144–151.e1.
- Mascarenhas Saraiva, M.; Afonso, J.; Ribeiro, T.; Ferreira, J.; Cardoso, H.; Andrade, P.; Gonçalves, R.; Cardoso, P.; Parente, M.; Jorge, R.; et al. Artificial intelligence and capsule endoscopy: Automatic detection of enteric protruding lesions using a convolutional neural network. Rev. Esp. Enferm. Dig. 2021, 115, 75–79.
- Yamada, A.; Niikura, R.; Otani, K.; Aoki, T.; Koike, K. Automatic detection of colorectal neoplasia in wireless colon capsule endoscopic images using a deep convolutional neural network. Endoscopy 2021, 53, 832–836.
- Saraiva, M.M.; Ferreira, J.P.S.; Cardoso, H.; Afonso, J.; Ribeiro, T.; Andrade, P.; Parente, M.P.L.; Jorge, R.N.; Macedo, G. Artificial intelligence and colon capsule endoscopy: Development of an automated diagnostic system of protruding lesions in colon capsule endoscopy. Tech. Coloproctol. 2021, 25, 1243–1248.
- Ribeiro, T.; Mascarenhas, M.; Afonso, J.; Cardoso, H.; Andrade, P.; Lopes, S.; Ferreira, J.; Mascarenhas Saraiva, M.; Macedo, G. Artificial intelligence and colon capsule endoscopy: Automatic detection of ulcers and erosions using a convolutional neural network. J. Gastroenterol. Hepatol. 2022, 37, 2282–2288.
- Majtner, T.; Brodersen, J.B.; Herp, J.; Kjeldsen, J.; Halling, M.L.; Jensen, M.D. A deep learning framework for autonomous detection and classification of Crohn’s disease lesions in the small bowel and colon with capsule endoscopy. Endosc. Int. Open 2021, 9, E1361–E1370.
- Ferreira, J.P.S.; de Mascarenhas Saraiva, M.; Afonso, J.P.L.; Ribeiro, T.F.C.; Cardoso, H.M.C.; Ribeiro Andrade, A.P.; de Mascarenhas Saraiva, M.N.G.; Parente, M.P.L.; Natal Jorge, R.; Lopes, S.I.O.; et al. Identification of Ulcers and Erosions by the Novel Pillcam™ Crohn’s Capsule Using a Convolutional Neural Network: A Multicentre Pilot Study. J. Crohn’s Colitis 2022, 16, 169–172.
- Mascarenhas Saraiva, M.; Ferreira, J.P.S.; Cardoso, H.; Afonso, J.; Ribeiro, T.; Andrade, P.; Parente, M.P.L.; Jorge, R.N.; Macedo, G. Artificial intelligence and colon capsule endoscopy: Automatic detection of blood in colon capsule endoscopy using a convolutional neural network. Endosc. Int. Open 2021, 9, E1264–E1268.
- Ding, Z.; Shi, H.; Zhang, H.; Meng, L.; Fan, M.; Han, C.; Zhang, K.; Ming, F.; Xie, X.; Liu, H.; et al. Gastroenterologist-Level Identification of Small-Bowel Diseases and Normal Variants by Capsule Endoscopy Using a Deep-Learning Model. Gastroenterology 2019, 157, 1044–1054.e5.
- Aoki, T.; Yamada, A.; Kato, Y.; Saito, H.; Tsuboi, A.; Nakada, A.; Niikura, R.; Fujishiro, M.; Oka, S.; Ishihara, S.; et al. Automatic detection of various abnormalities in capsule endoscopy videos by a deep learning-based system: A multicenter study. Gastrointest. Endosc. 2021, 93, 165–173.e1.
- Mascarenhas Saraiva, M.J.; Afonso, J.; Ribeiro, T.; Ferreira, J.; Cardoso, H.; Andrade, A.P.; Parente, M.; Natal, R.; Mascarenhas Saraiva, M.; Macedo, G. Deep learning and capsule endoscopy: Automatic identification and differentiation of small bowel lesions with distinct haemorrhagic potential using a convolutional neural network. BMJ Open Gastroenterol. 2021, 8, e000753.
- Mascarenhas, M.; Ribeiro, T.; Afonso, J.; Ferreira, J.P.S.; Cardoso, H.; Andrade, P.; Parente, M.P.L.; Jorge, R.N.; Mascarenhas Saraiva, M.; Macedo, G. Deep learning and colon capsule endoscopy: Automatic detection of blood and colonic mucosal lesions using a convolutional neural network. Endosc. Int. Open 2022, 10, E171–E177.
- Xie, X.; Xiao, Y.F.; Zhao, X.Y.; Li, J.J.; Yang, Q.Q.; Peng, X.; Nie, X.B.; Zhou, J.Y.; Zhao, Y.B.; Yang, H.; et al. Development and Validation of an Artificial Intelligence Model for Small Bowel Capsule Endoscopy Video Review. JAMA Netw. Open 2022, 5, e2221992.
- Xia, J.; Xia, T.; Pan, J.; Gao, F.; Wang, S.; Qian, Y.Y.; Wang, H.; Zhao, J.; Jiang, X.; Zou, W.B.; et al. Use of artificial intelligence for detection of gastric lesions by magnetically controlled capsule endoscopy. Gastrointest. Endosc. 2021, 93, 133–139.e4.
- Pan, J.; Xia, J.; Jiang, B.; Zhang, H.; Zhang, H.; Li, Z.S.; Liao, Z. Real-time identification of gastric lesions and anatomical landmarks by artificial intelligence during magnetically controlled capsule endoscopy. Endoscopy 2022, 54, E622–E623.
- Mascarenhas, M.; Mendes, F.; Ribeiro, T.; Afonso, J.; Cardoso, P.; Martins, M.; Cardoso, H.; Andrade, P.; Ferreira, J.; Saraiva, M.M.; et al. Deep Learning and Minimally Invasive Endoscopy: Automatic Classification of Pleomorphic Gastric Lesions in Capsule Endoscopy. Clin. Transl. Gastroenterol. 2023, 14, e00609.
More
