2. The Phenotypic and Genotypic Components of PN
In the last couple of years, multiple approaches have been designed to focus on nutrition and food science technology
[1]. These advanced methodologies are based on understanding the individual variability in response to foods to provide personalised nutritional recommendations specific to patient subgroups
[2]. PN is one of the promising methods that have been used for approaching the variation in individuals’ responses to diet, nutrients, metabolic activity, and treatment outcomes
[3]. These variations have been linked primarily to the composition of the gut microbiome, genetics/metabolic profile, and social and lifestyle habits specific to each individual
[4]. The gut microbiome has been classified as one of the factors that can predict individuals’ responses to diet and develop an appropriate model for PN
[5]. Understanding the variation in genetic and metabolic profiles can also help in providing specific dietary advice for individuals or population subgroups in the form of PN
[6]. PN can optimise the dietary response and health by considering the variations in individuals’ social status and lifestyle habits
[7].
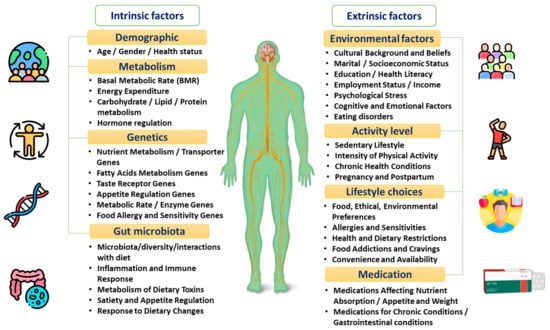
PN allows a better understanding of the inter-individual differences that are directly correlated to patients’ unique intrinsic factors, including the microbiome as well as the genetic and metabolic profile
[8][9][10][11][8,9,10,11]. Other factors including patients’ health status, physical activity, and dietary pattern, and psychosocial and socioeconomic characteristics can also extrinsically affect the response to dietary behaviours
[12][13][14][15][12,13,14,15], as shown in
Figure 1 and explained in the following sections.
Figure 1.
The factors affecting individuals’ dietary responses.
2.1. Gut Microbiota
The gut microbiota refers to the intestinal tract microorganisms responsible for the generation of metabolites, stabilisation of homeostasis, and maintenance of adequate immune responses
[16][17][16,17]. The intestinal microbiota is also connected with the brain axis to allow the exchange of information across the hypothalamus, pituitary, and adrenal glands. This interconnection is responsible for activating the dual hunger–satiety circuit and the dopamine reward path, producing energy and acquiring food from the environment
[18]. The axis between the brain and intestines can be influenced by the host’s genetic composition, level of stress, negative emotions, and diet type
[19]. The microbiota can also regulate the pathogenesis, progression, and management of diseases
[20][21][20,21]. The effectiveness of these functions relies on both the quantity and quality of the microbiota, as well as its metabolic potential
[22]. This shows that the characteristics of the gut microbiota can significantly vary across individuals based on their genetic profile, lifestyle, and habits
[23]. In practice, the gut microbiota is recognised as a key determinant in predicting how individuals respond to particular dietary components
[24]. Consequently, the direct evaluation of host–microbiota interactions constitutes an advanced therapeutic tool during disease control and prevention stages
[25]. This highlights the necessity of evaluating individuals’ microbiota to structure precision diets and interventions required for optimal health
[26].
In daily life, the type of consumed diet has been shown to influence the microbiome’s composition. For example, diets rich in animal-based nutrients can stimulate the release of bile-resistant species, while plant-based foods are associated with a higher level of plant polysaccharide-fermenting species
[27]. A limited 24 h consumption of carbohydrates can also decrease the production of bacteria responsible for destroying food fibres
[28]. In obesity and weight gain cases, the microbiota plays a crucial role in monitoring energy use and the formation of gut metabolites
[29]. Therefore, individuals eating an unhealthy diet and gaining weight for a prolonged period of more than ten years have limited intestinal microbiota diversity
[30]. Other findings relate the disruption in the microbiota’s composition to some inherited and non-modifiable individual characteristics, such as ethnicity and geographical setting
[31].
Another factor that can also interfere with the variety and stability of gut microbiota is the consumption of sugar substitutes
[32]. It was found that the administration of sucralose for 12 weeks was associated with lower levels of anaerobes,
bifidobacteria,
lactobacilli,
Bacteroides,
clostridia, and total aerobic bacteria
[33]. Prolonged sucralose consumption in mice caused a high release of bacterial pro-inflammatory genes and disruption in faecal metabolites
[34]. In turn, the limited utilisation of emulsifiers as food additives showed a reduced microbial diversity
[35]. The consumption of a fermentable oligosaccharides-, disaccharides-, monosaccharides-, and polyols (active b)-rich diet can also alter the gut microbiota
[36]. This type of diet has been shown to minimise the risk of insulin resistance in healthy overweight and obese patients
[37][38][37,38].
Animal and in vitro studies found that gluten-free bread intake lessens the microbiota dysbiosis usually occurring in gluten sensitivity or coeliac disease cases
[39][40][39,40]. Following a four-week gluten-free diet (GFD), individuals presented with different metabolic profiles and subsequent changes in gut microbiota
[41]. In healthy subjects, decreased levels of Bifidobacterium,
Clostridium lituseburense,
Faecalibacterium prausnitzii, and
Lactobacillus, and higher
Enterobacteriaceae and
Escherichia coli counts following GFD, were reported
[42]. There is some emphasis on the potential of a low-gluten diet to induce moderate changes in the intestinal microbiome, reduce fasting and postprandial hydrogen exhalation, and improve self-reported bloating in healthy individuals
[43]. Despite its advantages, GFD can be associated with a higher risk of heart disease due to a possible reduction in whole grains’ consumption
[44].
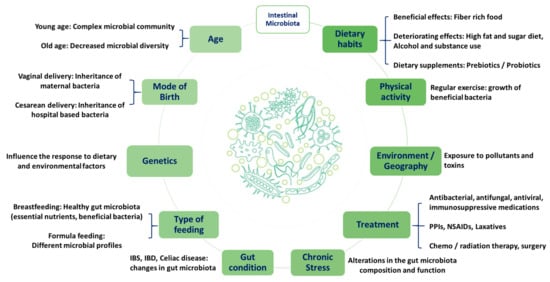
This may suggest the impact of dietary habits on gut microbiota and confirm the crucial role of the microbiome as a major contributing factor to PN (
Figure 2). Therefore, the variation between individuals and populations can affect the overall response to diet in terms of meals’ digestion, nutritional benefits, and personalisation.
Figure 2. Factors affecting individuals’ intestinal microbiota. Proton pump inhibitors (PPIs), nonsteroidal anti-inflammatory drugs (NSAIDs), irritable bowel syndrome (IBS), and irritable bowel disease (IBD).
2.2. Genetics and Metabolic Profile
The genetic makeup is another important factor that may contribute to the inter-individual variation in dietary behaviours
[45]. Some of the recent advances in the field of genomics assisted researchers in better understanding the role of genetic variant sites and functions in the development of chronic conditions. This also contributed to predicting the risk of chronic diseases and personalising their prevention and treatment plans
[46]. Accordingly, individuals may present with genetic variations, known as polymorphisms, which can lead to differences in the metabolic processing of nutrients within the same population
[47]. For example, the presence of a single-nucleotide polymorphism (SNP) in intron 1 of the cytochrome P450 enzyme
CYP1A2 gene was linked to a variation in caffeine metabolism
[48][49][48,49]. This may account for the high inter-individual variability found in caffeine intrinsic concentrations. In addition, individuals with the CC genotype of a SNP were more likely to gain weight when eating a high-saturated-fat diet (around 10% higher BMI), whereas those with the TT genotype were not associated with this complication
[50][51][50,51].
The mutual mapping of the individuals’ genetic and metabolic profiles constitutes an important tool for assessing the body’s response to different nutrients and tailoring a personalised diet
[52]. For example, a protein- and fibre-rich diet may benefit individuals suffering from low-insulin sensitivity, while a high monounsaturated fatty acids-based diet may benefit patients with insulin resistance
[53]. Interestingly, when measuring the metabolic response to high and low glycaemic index meals, it was found that certain subjects had a variance in their glucose and insulin responses to the same standardised index meals
[54]. This further strengthens the importance of taking into consideration the inter-individual alterations in metabolic profile while tailoring the diet to produce better health outcomes. In parallel, biological components, including proteins, metabolites, microbiota, and epigenetic markers, helped in understanding the possible association between the individuals’ physiological mechanisms and their susceptibility to chronic diseases
[55].
2.3. Psychosocial and Socioeconomic Status
Obesity has been correlated with an increased risk of psychosocial burden
[56]. In particular, obese individuals can suffer from mood, self-esteem, and body image-related issues
[57]. It was suggested that depressive symptoms are associated with altered eating behaviours and increased food and beverage caloric intake
[58]. This is likely due to the food’s ability to activate brain reward circuits that lead to the release of dopamine
[59]. Patients with eating disorders also reported difficulties in controlling the frequency of their eating, portion sizes, or extreme eating behaviour
[60]. This can be further associated with disordered eating leading to uncontrolled weight gain. In such cases, the psychosocial status of individuals should be considered as a crucial factor when tailoring a specific nutritional plan
[61]. The implementation of a long-term weight loss plan should also be considered to allow a gradual improvement in an individual’s psychological distress
[62].
Socioeconomic status can also be directly correlated with psychological status
[63], as individuals with a high socioeconomic status (SES) seem to follow healthier food habits
[64]. Individuals with a low SES are prone to a poorer health status, as they are unable to comply with the required nutritional recommendations or dietary guidelines; in turn, they are more likely to experience unhealthy conditions
[59][63][59,63]. Recent evidence suggested that a higher percentage of low SES households had unhealthy eating habits, such as consumption of fast foods, while high SES households had healthier eating patterns
[65]. This could be due to the lack of purchasing power in those with a low SES, which can lead to the consumption of cheaper and lower-quality ingredients, causing nutritional deficiencies
[66]. This confirms the importance of SES consideration when tailoring an individualised diet to improve the nutritive quality. Moreover, both social inequity and diet quality, in conjunction with healthy dietary behaviours, constitute a crucial and active public health concern.
3. PN Use in the Management of Obesity
Obesity is a complex non-communicable disease, which is influenced by both environmental and hereditary factors, representing a relevant target for PN
[67]. Recently, studies have shown significant correlations between individuals’ intrinsic components and the extrinsic factors that can directly affect their lifestyle and habits
[67]. In this case, PN can help in simultaneously evaluating individuals’ genes, metabolic markers, microbial species, environmental elements (sociodemographic and physical activity), and obesity phenotypic traits (body weight, body mass index, waist circumference, and central and regional adiposity).
3.1. Genetic Basis of Obesity
The progression of obesity has been correlated with multiple genetic factors that can affect the interaction of macronutrients with the individual’s genotype
[68][69][68,69]. Recently, advanced human genome sequencing and applied population genetics studies have been used as a main tool for detecting the gene variants associated with obesity and its related traits
[69]. SNPs have been known as one of the main types of genetic variants that are associated with obesity
[70]. For example, insulin-like growth factor, dioxygenase enzyme, melanocortin receptor, and apolipoprotein present SNPs associated with an increased risk of obesity
[1][2][16][17][18][71][1,2,16,17,18,71]. In parallel, the conduction of a Genome-Wide Association Study (GWAS) helped in detecting more than 140 obesity-related SNPs
[72], while another one revealed about 300 SNPs in total
[73]. Despite their discovery, the impact of these SNPs on BMI is still modestly rated, and further investigations are needed for evaluating the influence of genetics on the development of obesity
[70][73][70,73]. This cannot be relevant to Prader-Willy syndrome cases or genes related to leptin and melanocortin signalling, which have a higher influence on BMI
[74].
In some cases, genes are integrated with carbohydrate and lipid metabolism
[75], and in others, genes are responsible for activating the proteins of carbohydrates and lipid taste receptors
[76]. Some of the genes participate in encoding the lipid transporters of proteins or digestive enzymes present in starch and milk
[77], and some other genes are responsible for using and storing energy, food reward, and gut regulatory processes
[78][79][78,79]. For example, the intake of dietary fats and carbohydrates was found to be associated with the SNP “rs1761667” and “rs35874116” on the cluster of differentiation 36 (CD36) protein and taste 1 receptor member 2 (TAS1R2) gene, respectively
[18]. Moreover, “rs1799883” SNP of the fatty acid binding protein 2 (FABP2) gene was found to be associated with hypertriglyceridemia, while “rs9939609” SNP of the fat mass and obesity-associated (FTO) gene was correlated with an increased risk of body fat accumulation
[18]. In parallel, the “rs1800497” SNP of the dopamine receptor D2 (DRD2) gene was seen to interlink with the brain–gut microbiota axis and stimulate dysbiosis, negative emotions, and obesity
[18]. Despite their unsatisfactory effects, some genetic variations, such as a high AMY1 copy number, were seen to protect the body against obesity
[80].
It is worth mentioning that epigenetic changes linked to external factors can change genetic activity and express the obese phenotype
[81][82][93,94]. These epigenetic modifications were mainly documented following the practice of a dietary plan, physical activity, and surgeries
[13]. Therefore, advanced gene-based technologies have been implemented to personalise dietary recommendations based on individuals’ genetic profiles
[83][95]. Nutrigenomics studies reported how individuals’ genetic variations influence their responses to nutrients and how diet, in turn, affects gene expression
[84][96]. Limited data supported the superiority of this technology regarding weight loss results in comparison to standardised care
[85][86][97,98]. Currently, the increased application of pharmacogenomics to evaluate therapeutic responses to pharmaceutical compounds is associated with a marked clinical relevance
[87][99]. This advanced technique allows the mapping of genetic variants that can influence the response to weight loss treatment
[81][93]. However, pharmacogenomics application is still limited due to financial issues. In recent studies, the discovery of next-generation probiotics has been linked to several health benefits
[88][100]. The clinical use of these probiotics is also limited due to several reasons, such as safety, efficacy, and cost
[89][90][91][92][101,102,103,104]. In some cases, the transplantation of faecal matter has been initialised for the treatment of obesity and other metabolic disorders. Its clinical application remains limited due to the variation in the obtained findings
[93][105].
3.2. Weight Management
The consumption of specific types of food can help prevent the development of obesity
[94][106]. According to epidemiological research, consuming dairy products and vegetarian protein sources can protect against obesity, unlike consuming large amounts of meat, which is correlated with a greater risk of weight gain
[95][96][97][107,108,109]. This was supported by a Chinese study, which viewed that consuming large quantities of fatty food can increase the chance of weight gain and obesity
[98][110]. Therefore, poor diet quality was strongly correlated with a greater risk of weight gain despite gender differences
[99][111]. The increased caloric density of high-fat foods also promotes low-satiety effects, especially when consumed in large quantities
[100][112]. This can emphasise the need for a more passive focus on selecting the appropriate intervention for dietary self-monitoring adherence
[101][113].
In practice, the majority of obese women valued the use of weight management services and advice, despite the limited practical discussions and application of these approaches
[102][114]. The use of individualised information while providing nutritional advice helped in sustaining changes in healthy dietary behaviours
[103][115]. A UK-based study showed that applying PN advice through mobile applications was beneficial in improving diet quality and individuals’ engagement in dietary habits, in comparison to the general population
[104][116]. These findings highlighted the potential of PN to improve individuals’ adherence to dietary habits as well as improve weight and glucose management for a long period
[105][106][107][117,118,119]. In the long term, the benefits of PN use were associated with a decrease in total fat intake, in addition to compliance with nutritional advice
[108][120].
In daily life, limited physical activity due to a sedentary lifestyle, high screen time, processed meats, physical education, and transportation constitute a direct risk factor for obesity
[109][121]. For example, individuals exercising minimal physical effort have a greater chance of alleviating the risk of type 2 diabetes by 26% compared to unenergetic ones
[110][122]. When applied to physical activity, PN is still inconsistently modifying behavioural changes, such as the ones documented in dietary patterns and diet quality
[111][112][113][123,124,125]. The value of personalising dietary advice for modifying physical activity levels was not found to be superior to the conventional guidelines when the physical activity was objectively assessed
[114][115][126,127]. In some cases, PN was seen to significantly enhance individuals’ exercise frequency when they were informed about their genetic testing results
[116][128].
In summary, the obtained findings can illustrate crucial inputs about PN application in practice and its impact on changing individuals’ diet quality and physical activity, highlighting the need for further research.
3.3. Intestinal Bacterial Flora
The different responses to nutritional recommendations can be regulated by the composition of the gut microbiome for each individual
[117][118][129,130]. It has been evidenced that the intestinal microbiota is intrinsically affected by the overall health, including obesity risk
[119][131]. Physiologically, the gut microbiota utilises energy from the diet and interacts with the host genes that regulate the expansion and storage of energy
[120][132]. Therefore, live bacteria (probiotics), nondigestible or limited digestible food constituents, such as oligosaccharides (prebiotics), or both (synbiotics), or even faecal transplants have been used as an emerging tool to restore the intestinal microbiota and treat or prevent obesity
[121][122][123][124][133,134,135,136]. This may suggest the key role of the gut microbiota while applying the PN criteria to facilitate weight loss in obese individuals
[125][137]. A human study reported that obese individuals had more Firmicutes and nearly 90% fewer Bacteroidetes than lean individuals
[126][138]. It was observed that a healthy weight and good metabolic health were seen in patients with bacteria of the genus
Oscillospira, while
Collinsella aerofaciens bacteria were more frequently documented in obese individuals
[127][139]. Other anatomical and physiological changes can also occur in the gut microbiota following the performance of bariatric surgery. Despite its documented benefits regarding weight loss and glycaemic control, a recent study verified the alterations in microbial diversity and composition three months following bariatric surgery
[128][140]. More specifically, a high level of Proteobacteria and Bacteroidetes and a low Firmicutes concentration were reported
[129][141]. In the long term, microbiota species were still maintained, indicating that bariatric surgery could achieve a fast and prolonged modification in the patient’s gut microbiota
[129][141]. The transplantation of faecal microbiota has been reported to reduce body fat accumulation two weeks post-procedure in germ-free mice who had their Roux-en-Y Gastric Bypass (RYGB) or sleeve gastrectomy (SG; 46% and 26%, respectively)
[128][140]. Thus, the inter-individual changes in gut microbiota should always be considered when structuring a nutritional plan, since it can directly influence metabolism, resulting in either weight loss or gain
[130][142]. This was supported by a study validating that individuals’ gut microbiota can be used to design personalised diets for glucose homeostasis
[131][143].