Tattooing is the procedure of implanting permanent pigment granules and additives into the dermal layer of the skin, serving various purposes such as decoration, medical identification, or accidental markings. There has been a significant rise in the popularity of decorative tattooing as a form of body art among both teenagers and young adults. Thus, the incidence of tattoos is increasing, with expanding applications such as permanent makeup, scar camouflage, nipple–areola, lips, and eyebrows tattooing, and utilization in oncological radiotherapy such as colon marking. However, there have been reported a broad range of adverse reactions linked to tattooing, encompassing allergic reactions, superficial and deep cutaneous infections, autoimmune disorders induced by the Koebner phenomenon, cutaneous tumors, and others.
- tattoos
- side effects
- bacterial infections
- mycobacterial infections
- viral infections
- fungal infections
1. Introduction
2. Bacterial Infections
The most commonly encountered clinical infections related to tattoos include impetigo and folliculitis [3][15][3,55]. Staphylococcus aureus, Streptococcus pyogenes, Clostridium difficile, and Pseudomonas aeruginosa are the primary causative agents for these superficial infections [3][15][3,55] (Table 1). Clinical manifestations of bacterial infections encompass local pain, erythema, and swelling, as well as fever and purulence [3][16][3,56]. It is crucial to differentiate cellulitis or erysipelas from temporary tattoo-induced edema, which is a transient reaction inherent to the tattooing process, particularly when applied to the lower extremities [3][16][3,56]. This reaction is inevitable and can occur in any individual [3][16][3,56]. Most bacterial infections are easily treatable, and their treatment generally aligns with standard bacterial infection management (Table 1). They can be verified through suitable cultures and subsequently treated accordingly. However, certain pathogens may pose greater challenges. For instance, an epidemic of cutaneous infections caused by methicillin-resistant Staphylococcus aureus was reported in the USA following tattooing [3][17][18][3,12,57].| Side Effects |
Bacterial | Mycobacterial | |||
|---|---|---|---|---|---|
| Clinical measures | Staphylococcus aureus/Streptococcus pyogenes/Clostridium difficile/Pseudomonas aeruginosa [3][15][3,55] | Mycobacterium tuberculosis/Mycobacterium bovis [3][6][19][20][21][3,7,17,58,59] | Mycobacterium chelonae/Mycobacterium abscessus/Mycobacterium fortuitum [22][23][24][6,15,16] | Mycobacterium mageritense [3][25][26][3,60,61] | Mycobacterium leprae [1][3][27][1,3,62] |
| Standard bacterial infection management | Multidrug therapy administered in two phases [28][63]: Isoniazid Rifampicin Pyrazinamide Ethambutol or Streptomycin |
Macrolide antibiotics [29][64] (Clarithromycin) 4 months in mild cases 6–12 months in severe cases |
Antibiotic therapy [29][64]: Amikacin Imipenem Cefoxitin Fluroquinolones Sulfonamides |
Paucibacillary disease [30][65]: Dapsone + Rifampicin + Clofazimine for 6 months |
|
| Multibacillary disease [30][65]: Dapsone + Rifampicin + Clofazimine for 12 months |
|||||
| Rifampicin resistance [30][65]: 24 months treatment broken down as 6 months of Clofazimine + Ofloxacin and Minocycline followed by 18 months of Clofazimine + Ofloxacin or Minocycline |
|||||
| Dapsone resistance [30][65]: Clofazimine + Rifampicin for 6 months |
|||||
3. Mycobacterial Infections
Tattoo-inoculated mycobacterial infections encompass tuberculosis, leprosy, and atypical mycobacteria such as Mycobacterium chelonae and Mycobacterium abscessus [22][23][24][6,15,16]. Tattooing can lead to the development of primary cutaneous tuberculosis [3][6][20][24][3,7,16,58]. This occurs when individuals lacking previous immunity are inoculated with Mycobacterium tuberculosis or Mycobacterium bovis [3][6][19][20][21][3,7,17,58,59]. Within 2–4 weeks, an erythematous papule or nodule emerges, eventually progressing to a superficial ulcer known as a tuberculous chancre [3][6][19][20][21][3,7,17,58,59]. Often, painless regional lymphadenopathy ensues within 3 to 8 weeks [3][6][19][20][21][3,7,17,58,59]. In cases where the patient’s immune system is compromised, there is a risk of progression to lupus vulgaris and tuberculosis cutis verrucose, or even hematogenous spread [3][19][20][21][3,17,58,59]. Differential diagnoses include foreign-body granuloma, sarcoidosis, inoculation leprosy, tertiary syphilis, and infections with atypical mycobacteria [6][7]. The histological examination typically reveals epithelioid histiocytes, Langhans giant cells, and tuberculoid granulomas, with or without central caseous necrosis [3][19][20][21][3,17,58,59]. A positive tuberculin test holds significant diagnostic value for primary tuberculosis [6][19][20][21][7,17,58,59]. The treatment approach for cutaneous tuberculosis is consistent with that of systemic tuberculosis and involves multidrug therapy [28][63]. Commonly used drugs include isoniazid, rifampicin, pyrazinamide, and ethambutol or streptomycin, administered in two phases: the intensive one (which aims to rapidly reduce the burden of Mycobacterium tuberculosis and typically spans about 8 weeks) and the continuation phase, designed to eradicate any remaining bacteria and extends for a duration of 9 to 12 months [28][63] (Table 1). Strict adherence to the treatment regimen is crucial for a successful cure [28][63]. Various factors influence the outcomes of treatment, including the patient’s immunity, overall health, disease stage, type of cutaneous lesions, treatment adherence, duration of therapy, and potential side effects [28][63]. Atypical mycobacterial infections, particularly with Mycobacterium chelonae, appear to be an emerging complication [3][32][33][34][35][3,66,67,68,69]. This occurrence is particularly associated with the preparation of grey ink, which is obtained by diluting black ink with water [3][33][3,67]. If the water used in this process is contaminated with Mycobacterium chelonae, a bacterium commonly found in nonsterile water, it can lead to infections [3][33][3,67]. Less commonly, skin infections can be caused by other mycobacterial species, such as Mycobacterium haemophilum, Mycobacterium abscessus, Mycobacterium immunogenum, Mycobacterium massiliense, Mycobacterium mageritense, and Mycobacterium fortuitum [3][25][26][3,60,61] (Table 1). Interestingly, mycobacterial infections tend to manifest more frequently in the grey or black areas of a tattoo [3][33][3,67]. Clinically, lesions present as chronic papules, pustules, lichenoid plaques, and plaques with scales, typically developing within 1 to 3 weeks after the procedure [3][33][3,67]. Ulcerated nodules primarily confined to the tattooed area have also been reported [3][33][3,67]. For skin and soft-tissue infections caused by nontuberculous mycobacteria, a prolonged treatment regimen involving combination therapy with at least two susceptible antimicrobials is recommended to minimize the risk of antibiotic resistance [29][64]. Typically, the recommended duration of therapy for mild cases is around 4 months, while severe cases may require treatment for 6–12 months [29][64]. Macrolide antibiotics, with clarithromycin commonly included, are considered standard treatment for nontuberculous mycobacteria infections, including those associated with tattoos and involving Mycobacterium chelonae, Mycobacterium abscessus, and Mycobacterium fortuitum [29][64]. However, it is important to note that Mycobacterium mageritense is known to be resistant to macrolides due to the presence of the erythromycin ribosomal methylase gene, which imparts resistance to macrolide antibiotics [29][64]. Mycobacterium mageritense generally exhibits susceptibility or intermediate susceptibility to amikacin, imipenem, cefoxitin, fluoroquinolones, and sulfonamides but is resistant to clarithromycin [29][64]. It is essential to guide antibiotic therapy based on susceptibility testing [29][64] (Table 1). Instances of tattoo inoculation with Mycobacterium leprae are predominantly reported in regions where leprosy is endemic, and unhygienic tattooing practices are prevalent [1][3][27][1,3,62]. The onset of leprosy after tattooing can vary significantly, occurring between 10 to 20 years post-tattooing [1][3][27][1,3,62]. Outbreaks have been linked to the use of shared needles during unhygienic tattooing by roadside artists [3][6][27][3,7,62]. Manifestation of leprosy skin lesions may occur 10 to 20 years after the initial inoculation, and the clinical presentation is primarily influenced by the immunologic status of the host [3][6][27][3,7,62]. In cases where a mycobacterial infection is suspected, conducting a biopsy, tissue culture, and polymerase chain reaction for Mycobacterium species is recommended [3][6][27][3,7,62]. Histologically, these reactions are characterized by the formation of suppurative granulomas with the presence of polymorphonuclear leukocytes [3][6][27][3,7,62]. Treatment recommendations for leprosy in adults consist of long-term multidrug therapy: dapsone, rifampicin, and clofazimine for 6 months in paucibacillary disease and for 12 months in case of multibacillary disease [30][65]. In case of rifampicin resistance, clofazimine plus at least two of minocycline, clarithromycin, and quinolone for 6 months is recommended, followed by an additional 18 months of clofazimine plus one of the aforementioned drugs [30][65] (Table 1).4. Viral Infections
The transmission of infections such as verrucae, molluscum contagiosum virus, human papillomavirus (HPV), herpes simplex virus (HSV), human immunodeficiency virus (HIV), and hepatitis B (HBV) and C viruses (HCV) has been documented [3][6][3,7] (Figure 1 and Table 2).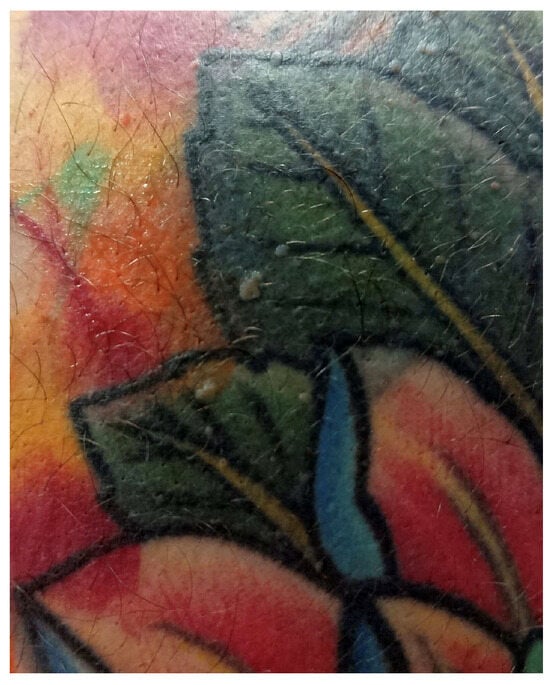
| Side Effects | Viral | Fungal | Parasitic | ||
|---|---|---|---|---|---|
| Clinical measures | Viral warts [3][12][36][37][38][3,52,70,71,72] | Molluscum contagiosum [3][12][[38][336][37],52,70,71,72] | HPV, HSV, HIV, HBV and HCV [3][6][3,7] | Dermatophytes/Aspergillus fumigatus/Sporotrichosis/Zygomycosis/Acremonium fungi/Candida [3][6][31][39][40][3,7,14,73,74] | Leishmania species [3] |
| Firstline [41][42][75,76]: Salicylic Acid Cryotherapy |
First-line [43][44][45][77,78,79]: Cryotherapy Curetage Cantharidin Podophyllotoxin |
Multidisciplinary medical personnel (infectious disease specialist) Antivirals as standard therapeutic approach |
Topical antifungals: Clotrimazole Econazole Miconazole Ketoconazole Nystatin Terbinafine |
Cryotherapy Photodynamic therapy Imiquimod [46][80] |
|
| Refractory warts [42][76]: Topical immunotherapy (contact allergens, intralesional Bleomycin, Fluorouracil) |
Other [43][44][45][47][48][49][50][51][77,78,79,81,82,83,84,85]: Imiquimod Salicylic Acid Topical retinoids |
Systemic antifungals: Amphotericin B Itraconazole Fluconazole Voriconazole Terbinafine Griseofulvin |
Intralesional or systemic antimonials [46][80]: Sodium stibogluconate Meglumine antimoniate |
||
| Other [41][42][52][53][54][55][56][57][75,76,86,87,88,89,90,91]: Cantharidin Imiquimod Trichloroacetic acid Pulsed dye laser Intralesional immunotheraphy Surgery |
Other systemic therapies [46][80]: AmphotericinB Miltefosine Pentamidin Itraconazole Fluconazole Ketoconazole Paromomycin Zinc sulfate Allopurinol |
||||


