Brain spaces around (perivascular spaces) and alongside (paravascular or Virchow–Robin spaces) vessels have gained significant attention due to the advancements of in vivo imaging tools and to their crucial role in maintaining brain health, contributing to the anatomic foundation of the glymphatic system. In fact, it is widely accepted that peri- and para-vascular spaces function as waste clearance pathways for the brain for materials such as ß-amyloid by allowing exchange between cerebrospinal fluid and interstitial fluid. Visible brain spaces on magnetic resonance imaging are often a normal finding, but they have also been associated with a wide range of neurological and systemic conditions, suggesting their potential as early indicators of intracranial pressure and neurofluid imbalance.
- perivascular spaces
- paravascular spaces
- Virchow–Robin spaces
- PVS
- glymphatic system
- neurofluids
- magnetic resonance imaging
- MRI
1. Introduction
2. Anatomy
The anatomy of PeVS and PaVS is intricate and remains a matter of debate. In humans, the cortical surface of the brain and the intracranial perforating arterioles are covered by the pia mater [9,10][6][7]. Arterioles that traverse the base of the brain and enter the basal ganglia are enveloped by two layers of leptomeninges along their length, forming a space between them that communicates with the subarachnoid space [11,12][8][9]. Arterioles in the cortex and venules have a single leptomeningeal membrane that adheres closely to the vessel wall without an outer layer, permitting that the spaces surrounding these vessels communicate with the subpial space directly and, somehow, indirectly with the subarachnoid space [13,14,15][10][11][12]. These spaces can be defined as PaVS and correspond to the “Virchow–Robin spaces”. They are bound internally by the pial sheath and externally by the basement membrane of astrocytes (glia limitans) on the arterial side and the vein wall and the glia limitans on the venous side [16,17][13][14]. The glymphatic model suggests that CSF flows through para-arterial spaces, interacts with interstitial fluid and solutes, and then is removed from the brain through para-venous spaces [18][15]. There are also other spaces within the arterial tunica media, located between the middle layers of the basement membrane of arterial smooth muscle cells [17][14]. These structures are called PeVS, and they serve as channels for interstitial fluid flow in the opposite direction to that of blood flow (also known as the intramural periarterial drainage pathway) towards the cervical lymph nodes through major cerebral arteries in the neck [16,19][13][16]. The venous vasculature does not contain PeVS [17][14]. In summary, PeVS are spaces around the blood vessels (between the basement membrane of the pial sheath and the basement membrane of the arteries), while PaVS are spaces alongside the blood vessels (outside the vessel wall) (Figure 1).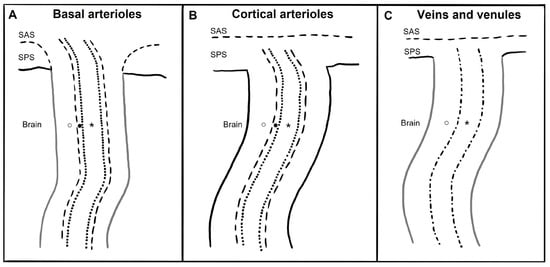
3. Imaging
4. Quantification
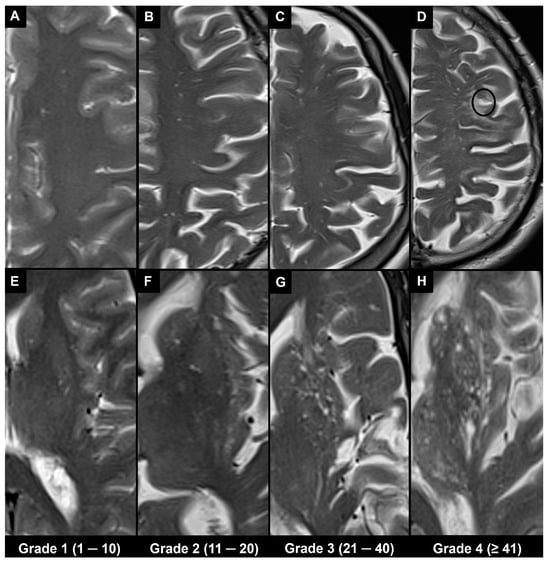
4.1. Visual Scoring
4.2. Automatic and Semi-Automatic Segmentation and Morphometry
Advances in technology have led to the emergence of various automatic and semi-automatic methods for segmenting and quantifying PVS. Once the PVS are segmented, various metrics and morphological features can be computed from segmentation masks [24,52][20][39]. The PVS volume is an indicator of the amount of fluid within the PVS [33][29]. The mean cross-sectional diameter can be utilized to differentiate PVS from other cerebral small vessel disease-related lesions [53][40]. Linearity represents the similarity of a particular PVS cluster to the tubular morphology [54][41], while solidity reflects the shape complexity of PVS, where a lower solidity indicates a more tortuous and less compact shape [24][20].5. Associations
5.1. Physiological
It is widely known that the visibility of PVS increases with age, especially in the basal ganglia, centrum semiovale, and hippocampus [66][42]. A recent study documented low PVS volumes in the basal ganglia and centrum semiovale in healthy subjects up to the age of 35 despite high Potter visual scores in the white matter of young subjects; also, it was suggested that in the basal ganglia, a Potter grade 1 and a Potter grade 3 could be considered physiological until the age of 50 and from the age of 70 onward, respectively, while in the centrum semiovale, a Potter grade 4 could be considered physiological from the age of 50 [67][43]. A higher PVS burden has been associated with the male sex, and it is also seen in healthy adolescents [33,65][29][44]. A circadian dynamic nature of the amount of MRI-visible PVS (higher PVS burden is visible on MRI at later times of the day) with a predominantly asymmetric distribution has been suggested. This could be associated with circadian fluctuations in respiration or/and blood pressure (which are known regulators of perivascular flow) or may be linked to the circadian control of flow through aquaporin-4 (a water channel that facilitates fluid transport from the PVS to the cerebral parenchyma) [33][29].5.2. Pathological
It is widely known that the visibility of PVS in the basal ganglia (but not in the centrum semiovale) increases with hypertension [66][42], and hypertension was found to be related to a low DTI-ALPS index [70][45]. Historically, MRI biomarkers of cerebral small vessel disease have included enlarged PVS along with other indicators such as recent small subcortical infarcts, lacunes, white matter hyperintensities (WMH) of presumed vascular origin, cerebral microbleeds, and brain atrophy, which are often present in association with stroke or cognitive decline.6. Differential Diagnosis
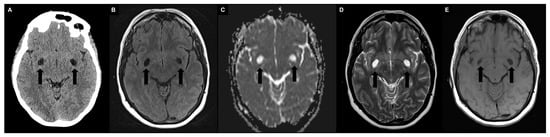
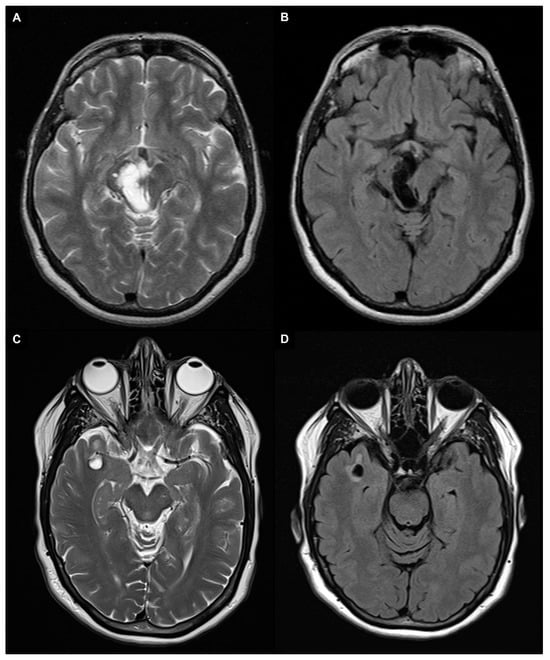
Enlarged PVS (diameter between 3–5 and 15 mm) most frequently need to be differentiated from lacunes and WMH as they are similar in signal characteristics and they often coexist in the context of cerebral small vessel disease (Figure 5A–F) [29,104][25][46]. When PVS appear notably enlarged (e.g., giant PVS with diameter ≥ 15 mm), causing mass effect, and presenting cystic configurations, they must be distinguished from other cystic pathologies of possible congenital, vascular, inflammatory, neoplastic, or hereditary nature (Figure 5G–L) [105,106][47][48].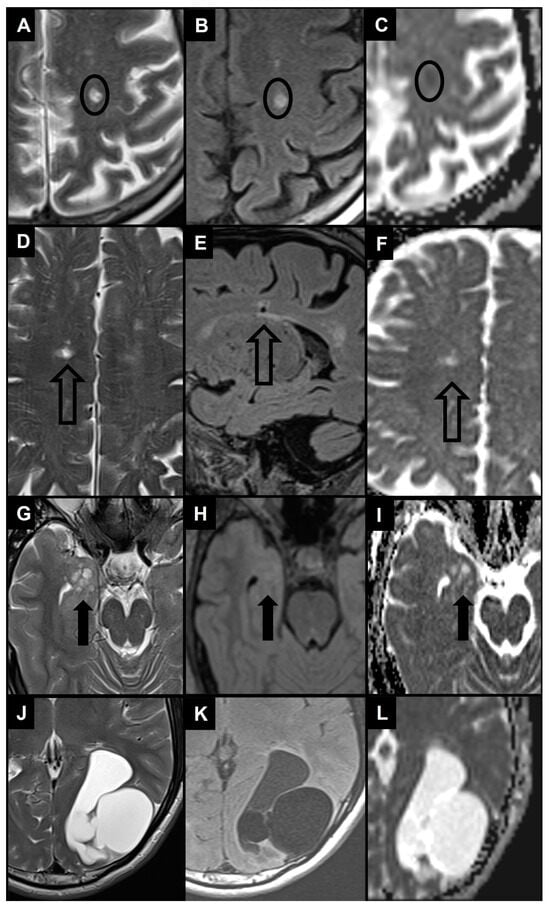
6.1. Recent Small Subcortical Infarct
6.2. Lacune of Presumed Vascular Origin
6.3. WMH
WMH of presumed vascular origin are bright on FLAIR and T2-weighted images and may appear as iso- or hypointense on T1-weighted sequences, without cavitation (different signal from CSF) [29][25]. The distribution patterns of WMH and PVS are similar, as they tend to be symmetric. However, WMH are often located in the periventricular region and follow the contour of the lateral ventricles, while PVS are typically not present in this area.6.4. Benign Intracranial Cysts
There are several types of noncancerous cystic masses resulting from congenital abnormalities with different embryological origins [109][50]. Choroidal fissure cysts refer to non-cancerous cysts that develop within the choroidal fissure [110][51]; hippocampal sulcus remnant cysts resemble a “string of beads” between the cornu ammonis and dentate gyrus [111][52]. The differentiation with PVS is based on their specific location within the brain. Neuroglial cysts do not have any communication with the ventricular system or arachnoid space and are distinct from PVS as they are solitary lesions, while arachnoid cysts are extra-axial CSF fluid collections commonly observed in the perisellar cysterns and middle cranial fossa; thus, their location and solitary nature are the main distinguishing factors separating them from clusters of PVS.6.5. Neoplastic Intracranial Cysts
It is possible to misclassify enlarged PVS as multinodular and vacuolating neuronal tumors and dysembryoplastic neuroepithelial tumors. Multinodular and vacuolating neuronal tumors are a type of benign, mixed glial neuronal lesion associated with seizures. They are a cluster of small, cystic, and nodular lesions located in the subcortical region in the deep cortical ribbon or in the convexities white matter. They show T2/FLAIR hyperintensity and rarely exhibit progression or contrast enhancement [40,112][30][53]. Dysembryoplastic neuroepithelial tumors are WHO grade I tumors that are typically found in the medial temporal lobes and cause complex partial seizures. They are generally benign and slow-growing, with a distinct “bubbly” cystic appearance associated with T2/FLAIR signal abnormality and faint contrast enhancement [40,113][30][54].6.6. Vascular and Inflammatory Cysts
Porencephalic cysts, secondary to a focal cerebral injury in early pregnancy, may occur in the periventricular white matter [114][55]. These cysts have unusual T2/FLAIR signals, connections with the ventricular system, and/or subarachnoid space, which distinguishes them from enlarged PVS. Cystic periventricular leukomalacia, resulting from hypoxic ischemic events during pre- or peri-natal age, is commonly observed in premature infants with cerebral palsy. Loss of periventricular white matter, mostly in periatrial regions, is evident with focal ventricular enlargement near abnormal hyperintense white matter in T2/FLAIR images. The damage tends to be symmetric, and thinning of the corpus callosum may also occur. Previous hemorrhage may also cause hypointensity in SWI [35,115][56][57].6.7. Infectious Cysts
Multiple cystic lesions in the brain can be caused by rare infectious processes. The most prevalent parasitic infection in the CNS and a major cause of acquired epilepsy worldwide is neurocysticercosis, caused by Taenia solium. The gray-white matter junction, basal ganglia, brainstem, cerebellum, subarachnoid space, ventricles, or spinal cord may contain fluid-filled oval cysts with an internal scolex (cysticerci).6.8. Inherited Cysts
Among hereditary disorders, mucopolysaccharidoses should be considered in the differential diagnosis of enlarged PVS. They are a group of metabolic disorders identified by a lack of enzymes causing an inability to break down glycosaminoglycan, leading to toxic intracellular substrate accumulation. Enlarged PVS are a common occurrence due to the accumulation of glycosaminoglycan, with a cribriform appearance on T1-weighted images of the basal ganglia, corpus callosum, and white matter. The PVS appear isointense to CSF on both T2-weighted and FLAIR images, but there may be an increased signal intensity in the surrounding white matter, which could signify dys- or demyelination, edema, or gliosis. The clinical picture is characterized by macrocephaly, musculoskeletal deformities, and mental and motor impairment [35,122,123][56][58][59].7. Conclusions
The imaging of PVS has become an important target of routine brain MRI interpretation, also related to the increased diagnostic capacity of current MRI equipment and sequences. Visible PVS on MRI have been associated with a wide range of neurological and systemic conditions, although this finding is currently not specific. Radiologists play a crucial role in identifying and characterizing PVS as they may provide important diagnostic and prognostic information considering their potential as an early indicator of vascular dysfunction and neurodegenerative/neuroinflammatory disorders. Thus, it is important for brain specialists to be familiar with the terminology and classification systems for PVS, as well as their normal and abnormal appearances, clinical meaning, and differential diagnosis.References
- Wardlaw, J.M.; Benveniste, H.; Nedergaard, M.; Zlokovic, B.V.; Mestre, H.; Lee, H.; Doubal, F.N.; Brown, R.; Ramirez, J.; MacIntosh, B.J.; et al. Perivascular Spaces in the Brain: Anatomy, Physiology and Pathology. Nat. Rev. Neurol. 2020, 16, 137–153.
- Robin, C. Recherches Sur Quelques Particularites de La Structure Des Capillaires de l’encephale. J. Physiol. Homme Anim. 1859, 2, 537–548.
- Virchow, R. Ueber die Erweiterung kleinerer Gefäfse. Arch. Für Pathol. Anat. Physiol. Für Klin. Med. 1851, 3, 427–462.
- Iliff, J.J.; Wang, M.; Liao, Y.; Plogg, B.A.; Peng, W.; Gundersen, G.A.; Benveniste, H.; Vates, G.E.; Deane, R.; Goldman, S.A.; et al. A Paravascular Pathway Facilitates CSF Flow through the Brain Parenchyma and the Clearance of Interstitial Solutes, Including Amyloid β. Sci. Transl. Med. 2012, 4, 147ra111.
- Gouveia-Freitas, K.; Bastos-Leite, A.J. Perivascular Spaces and Brain Waste Clearance Systems: Relevance for Neurodegenerative and Cerebrovascular Pathology. Neuroradiology 2021, 63, 1581–1597.
- Weller, R.O.; Hawkes, C.A.; Kalaria, R.N.; Werring, D.J.; Carare, R.O. White Matter Changes in Dementia: Role of Impaired Drainage of Interstitial Fluid. Brain Pathol. Zur. Switz. 2015, 25, 63–78.
- Absinta, M.; Ha, S.-K.; Nair, G.; Sati, P.; Luciano, N.J.; Palisoc, M.; Louveau, A.; Zaghloul, K.A.; Pittaluga, S.; Kipnis, J.; et al. Human and Nonhuman Primate Meninges Harbor Lymphatic Vessels That Can Be Visualized Noninvasively by MRI. eLife 2017, 6, e29738.
- Bouvy, W.H.; Biessels, G.J.; Kuijf, H.J.; Kappelle, L.J.; Luijten, P.R.; Zwanenburg, J.J.M. Visualization of Perivascular Spaces and Perforating Arteries with 7 T Magnetic Resonance Imaging. Investig. Radiol. 2014, 49, 307–313.
- Weller, R.O.; Djuanda, E.; Yow, H.-Y.; Carare, R.O. Lymphatic Drainage of the Brain and the Pathophysiology of Neurological Disease. Acta Neuropathol. 2009, 117, 1–14.
- Ringstad, G.; Valnes, L.M.; Dale, A.M.; Pripp, A.H.; Vatnehol, S.-A.S.; Emblem, K.E.; Mardal, K.-A.; Eide, P.K. Brain-Wide Glymphatic Enhancement and Clearance in Humans Assessed with MRI. JCI Insight 2018, 3, e121537.
- Eide, P.K.; Vatnehol, S.A.S.; Emblem, K.E.; Ringstad, G. Magnetic Resonance Imaging Provides Evidence of Glymphatic Drainage from Human Brain to Cervical Lymph Nodes. Sci. Rep. 2018, 8, 7194.
- Roher, A.E.; Kuo, Y.-M.; Esh, C.; Knebel, C.; Weiss, N.; Kalback, W.; Luehrs, D.C.; Childress, J.L.; Beach, T.G.; Weller, R.O.; et al. Cortical and Leptomeningeal Cerebrovascular Amyloid and White Matter Pathology in Alzheimer’s Disease. Mol. Med. Camb. Mass. 2003, 9, 112–122.
- Bakker, E.N.T.P.; Bacskai, B.J.; Arbel-Ornath, M.; Aldea, R.; Bedussi, B.; Morris, A.W.J.; Weller, R.O.; Carare, R.O. Lymphatic Clearance of the Brain: Perivascular, Paravascular and Significance for Neurodegenerative Diseases. Cell. Mol. Neurobiol. 2016, 36, 181–194.
- Bacyinski, A.; Xu, M.; Wang, W.; Hu, J. The Paravascular Pathway for Brain Waste Clearance: Current Understanding, Significance and Controversy. Front. Neuroanat. 2017, 11, 101.
- Tarasoff-Conway, J.M.; Carare, R.O.; Osorio, R.S.; Glodzik, L.; Butler, T.; Fieremans, E.; Axel, L.; Rusinek, H.; Nicholson, C.; Zlokovic, B.V.; et al. Clearance Systems in the Brain-Implications for Alzheimer Disease. Nat. Rev. Neurol. 2015, 11, 457–470.
- Carare, R.O.; Bernardes-Silva, M.; Newman, T.A.; Page, A.M.; Nicoll, J.A.R.; Perry, V.H.; Weller, R.O. Solutes, but Not Cells, Drain from the Brain Parenchyma along Basement Membranes of Capillaries and Arteries: Significance for Cerebral Amyloid Angiopathy and Neuroimmunology. Neuropathol. Appl. Neurobiol. 2008, 34, 131–144.
- George, I.C.; Arrighi-Allisan, A.; Delman, B.N.; Balchandani, P.; Horng, S.; Feldman, R. A Novel Method to Measure Venular Perivascular Spaces in Patients with MS on 7T MRI. AJNR Am. J. Neuroradiol. 2021, 42, 1069–1072.
- Jochems, A.C.C.; Blair, G.W.; Stringer, M.S.; Thrippleton, M.J.; Clancy, U.; Chappell, F.M.; Brown, R.; Jaime Garcia, D.; Hamilton, O.K.L.; Morgan, A.G.; et al. Relationship Between Venules and Perivascular Spaces in Sporadic Small Vessel Diseases. Stroke 2020, 51, 1503–1506.
- Brown, W.R.; Moody, D.M.; Challa, V.R.; Thore, C.R.; Anstrom, J.A. Venous Collagenosis and Arteriolar Tortuosity in Leukoaraiosis. J. Neurol. Sci. 2002, 203–204, 159–163.
- Barisano, G.; Lynch, K.M.; Sibilia, F.; Lan, H.; Shih, N.-C.; Sepehrband, F.; Choupan, J. Imaging Perivascular Space Structure and Function Using Brain MRI. NeuroImage 2022, 257, 119329.
- Montagne, A.; Nikolakopoulou, A.M.; Zhao, Z.; Sagare, A.P.; Si, G.; Lazic, D.; Barnes, S.R.; Daianu, M.; Ramanathan, A.; Go, A.; et al. Pericyte Degeneration Causes White Matter Dysfunction in the Mouse Central Nervous System. Nat. Med. 2018, 24, 326–337.
- Perosa, V.; Oltmer, J.; Munting, L.P.; Freeze, W.M.; Auger, C.A.; Scherlek, A.A.; van der Kouwe, A.J.; Iglesias, J.E.; Atzeni, A.; Bacskai, B.J.; et al. Perivascular Space Dilation Is Associated with Vascular Amyloid-β Accumulation in the Overlying Cortex. Acta Neuropathol. 2022, 143, 331–348.
- Oztürk, M.H.; Aydingöz, U. Comparison of MR Signal Intensities of Cerebral Perivascular (Virchow-Robin) and Subarachnoid Spaces. J. Comput. Assist. Tomogr. 2002, 26, 902–904.
- Naganawa, S.; Nakane, T.; Kawai, H.; Taoka, T. Differences in Signal Intensity and Enhancement on MR Images of the Perivascular Spaces in the Basal Ganglia versus Those in White Matter. Magn. Reson. Med. Sci. MRMS Off. J. Jpn. Soc. Magn. Reson. Med. 2018, 17, 301–307.
- Wardlaw, J.M.; Smith, E.E.; Biessels, G.J.; Cordonnier, C.; Fazekas, F.; Frayne, R.; Lindley, R.I.; O’Brien, J.T.; Barkhof, F.; Benavente, O.R.; et al. Neuroimaging Standards for Research into Small Vessel Disease and Its Contribution to Ageing and Neurodegeneration. Lancet Neurol. 2013, 12, 822–838.
- Yu, L.; Hu, X.; Li, H.; Zhao, Y. Perivascular Spaces, Glymphatic System and MR. Front. Neurol. 2022, 13, 844938.
- Mallio, C.A.; Quattrocchi, C.C.; Rovira, À.; Parizel, P.M. Gadolinium Deposition Safety: Seeking the Patient’s Perspective. AJNR Am. J. Neuroradiol. 2020, 41, 944–946.
- Parillo, M.; Mallio, C.A.; Van der Molen, A.J.; Rovira, À.; Ramalho, J.; Ramalho, M.; Gianolio, E.; Karst, U.; Radbruch, A.; Stroomberg, G.; et al. Skin Toxicity after Exposure to Gadolinium-Based Contrast Agents in Normal Renal Function, Using Clinical Approved Doses: Current Status of Preclinical and Clinical Studies. Investig. Radiol. 2023, 58, 530–538.
- Barisano, G.; Sheikh-Bahaei, N.; Law, M.; Toga, A.W.; Sepehrband, F. Body Mass Index, Time of Day and Genetics Affect Perivascular Spaces in the White Matter. J. Cereb. Blood Flow. Metab. Off. J. Int. Soc. Cereb. Blood Flow. Metab. 2021, 41, 1563–1578.
- Rudie, J.D.; Rauschecker, A.M.; Nabavizadeh, S.A.; Mohan, S. Neuroimaging of Dilated Perivascular Spaces: From Benign and Pathologic Causes to Mimics. J. Neuroimaging Off. J. Am. Soc. Neuroimaging 2018, 28, 139–149.
- Papayannis, C.E.; Saidon, P.; Rugilo, C.A.; Hess, D.; Rodriguez, G.; Sica, R.E.P.; Rey, R.C. Expanding Virchow Robin Spaces in the Midbrain Causing Hydrocephalus. AJNR Am. J. Neuroradiol. 2003, 24, 1399–1403.
- Loh, D.D.L.; Swaminathan, S.K. Tumefactive Perivascular Spaces Causing Obstructive Hydrocephalus. Radiology 2023, 307, e221724.
- Kwee, R.M.; Kwee, T.C. Tumefactive Virchow-Robin Spaces. Eur. J. Radiol. 2019, 111, 21–33.
- Cheraya, G.; Bajaj, S.; Sharma, S.; Gandhi, D.; Shah, J.; Parikh, N.; Gupta, N. Giant Perivascular Spaces in Brain: Case Report with a Comprehensive Literature Review. Precis. Cancer Med. 2022, 5, 29.
- Lakhani, D.A.; Joseph, J. Giant Tumefactive Perivascular Spaces. Radiology 2023, 307, 222559.
- Rawal, S.; Croul, S.E.; Willinsky, R.A.; Tymianski, M.; Krings, T. Subcortical Cystic Lesions within the Anterior Superior Temporal Gyrus: A Newly Recognized Characteristic Location for Dilated Perivascular Spaces. AJNR Am. J. Neuroradiol. 2014, 35, 317–322.
- Lim, A.T.; Chandra, R.V.; Trost, N.M.; McKelvie, P.A.; Stuckey, S.L. Large Anterior Temporal Virchow-Robin Spaces: Unique MR Imaging Features. Neuroradiology 2015, 57, 491–499.
- Potter, G.M.; Chappell, F.M.; Morris, Z.; Wardlaw, J.M. Cerebral Perivascular Spaces Visible on Magnetic Resonance Imaging: Development of a Qualitative Rating Scale and Its Observer Reliability. Cerebrovasc. Dis. Basel Switz. 2015, 39, 224–231.
- Moses, J.; Sinclair, B.; Law, M.; O’Brien, T.J.; Vivash, L. Automated Methods for Detecting and Quantitation of Enlarged Perivascular Spaces on MRI. J. Magn. Reson. Imaging JMRI 2023, 57, 11–24.
- Zong, X.; Park, S.H.; Shen, D.; Lin, W. Visualization of Perivascular Spaces in the Human Brain at 7T: Sequence Optimization and Morphology Characterization. NeuroImage 2016, 125, 895–902.
- Boespflug, E.L.; Schwartz, D.L.; Lahna, D.; Pollock, J.; Iliff, J.J.; Kaye, J.A.; Rooney, W.; Silbert, L.C. MR Imaging-Based Multimodal Autoidentification of Perivascular Spaces (mMAPS): Automated Morphologic Segmentation of Enlarged Perivascular Spaces at Clinical Field Strength. Radiology 2018, 286, 632–642.
- Francis, F.; Ballerini, L.; Wardlaw, J.M. Perivascular Spaces and Their Associations with Risk Factors, Clinical Disorders and Neuroimaging Features: A Systematic Review and Meta-Analysis. Int. J. Stroke Off. J. Int. Stroke Soc. 2019, 14, 359–371.
- Kim, H.G.; Shin, N.-Y.; Nam, Y.; Yun, E.; Yoon, U.; Lee, H.S.; Ahn, K.J. MRI-Visible Dilated Perivascular Space in the Brain by Age: The Human Connectome Project. Radiology 2023, 306, e213254.
- Piantino, J.; Boespflug, E.L.; Schwartz, D.L.; Luther, M.; Morales, A.M.; Lin, A.; Fossen, R.V.; Silbert, L.; Nagel, B.J. Characterization of MR Imaging-Visible Perivascular Spaces in the White Matter of Healthy Adolescents at 3T. AJNR Am. J. Neuroradiol. 2020, 41, 2139–2145.
- Kikuta, J.; Kamagata, K.; Takabayashi, K.; Taoka, T.; Yokota, H.; Andica, C.; Wada, A.; Someya, Y.; Tamura, Y.; Kawamori, R.; et al. An Investigation of Water Diffusivity Changes along the Perivascular Space in Elderly Subjects with Hypertension. AJNR Am. J. Neuroradiol. 2022, 43, 48–55.
- Mahammedi, A.; Wang, L.L.; Williamson, B.J.; Khatri, P.; Kissela, B.; Sawyer, R.P.; Shatz, R.; Khandwala, V.; Vagal, A. Small Vessel Disease, a Marker of Brain Health: What the Radiologist Needs to Know. AJNR Am. J. Neuroradiol. 2022, 43, 650–660.
- Cervantes-Arslanian, A.; Garcia, H.H.; Rapalino, O. Imaging of Infectious and Inflammatory Cystic Lesions of the Brain, a Narrative Review. Expert. Rev. Neurother. 2023, 23, 237–247.
- Sharma, V.; Prabhash, K.; Noronha, V.; Tandon, N.; Joshi, A. A Systematic Approach to Diagnosis of Cystic Brain Lesions. South Asian J. Cancer 2013, 2, 98–101.
- Erkinjuntti, T.; Inzitari, D.; Pantoni, L.; Wallin, A.; Scheltens, P.; Rockwood, K.; Roman, G.C.; Chui, H.; Desmond, D.W. Research Criteria for Subcortical Vascular Dementia in Clinical Trials. J. Neural Transm. Suppl. 2000, 59, 23–30.
- Robles, L.A.; Paez, J.M.; Ayala, D.; Boleaga-Duran, B. Intracranial Glioependymal (Neuroglial) Cysts: A Systematic Review. Acta Neurochir. 2018, 160, 1439–1449.
- Altafulla, J.J.; Suh, S.; Bordes, S.; Prickett, J.; Iwanaga, J.; Loukas, M.; Dumont, A.S.; Tubbs, R.S. Choroidal Fissure and Choroidal Fissure Cysts: A Comprehensive Review. Anat. Cell Biol. 2020, 53, 121–125.
- Yamashita, K.; Zong, X.; Hung, S.-C.; Lin, W.; Castillo, M. Hippocampal Sulcus Remnant: Common Finding in Nonelderly Adults on Ultra-High-Resolution 7T Magnetic Resonance Imaging. J. Comput. Assist. Tomogr. 2020, 44, 43–46.
- Buffa, G.B.; Chaves, H.; Serra, M.M.; Stefanoff, N.I.; Gagliardo, A.S.; Yañez, P. Multinodular and Vacuolating Neuronal Tumor of the Cerebrum (MVNT): A Case Series and Review of the Literature. J. Neuroradiol. J. Neuroradiol. 2020, 47, 216–220.
- Luzzi, S.; Elia, A.; Del Maestro, M.; Elbabaa, S.K.; Carnevale, S.; Guerrini, F.; Caulo, M.; Morbini, P.; Galzio, R. Dysembryoplastic Neuroepithelial Tumors: What You Need to Know. World Neurosurg. 2019, 127, 255–265.
- Abergel, A.; Lacalm, A.; Massoud, M.; Massardier, J.; des Portes, V.; Guibaud, L. Expanding Porencephalic Cysts: Prenatal Imaging and Differential Diagnosis. Fetal Diagn. Ther. 2017, 41, 226–233.
- Kwee, R.M.; Kwee, T.C. Virchow-Robin Spaces at MR Imaging. Radiogr. Rev. Publ. Radiol. Soc. N. Am. Inc. 2007, 27, 1071–1086.
- Hinojosa-Rodríguez, M.; Harmony, T.; Carrillo-Prado, C.; Van Horn, J.D.; Irimia, A.; Torgerson, C.; Jacokes, Z. Clinical Neuroimaging in the Preterm Infant: Diagnosis and Prognosis. NeuroImage Clin. 2017, 16, 355–368.
- Zafeiriou, D.I.; Batzios, S.P. Brain and Spinal MR Imaging Findings in Mucopolysaccharidoses: A Review. AJNR Am. J. Neuroradiol. 2013, 34, 5–13.
- Matheus, M.G.; Castillo, M.; Smith, J.K.; Armao, D.; Towle, D.; Muenzer, J. Brain MRI Findings in Patients with Mucopolysaccharidosis Types I and II and Mild Clinical Presentation. Neuroradiology 2004, 46, 666–672.
