Brain spaces around (perivascular spaces) and alongside (paravascular or Virchow–Robin spaces) vessels have gained significant attention due to the advancements of in vivo imaging tools and to their crucial role in maintaining brain health, contributing to the anatomic foundation of the glymphatic system. In fact, it is widely accepted that peri- and para-vascular spaces function as waste clearance pathways for the brain for materials such as ß-amyloid by allowing exchange between cerebrospinal fluid and interstitial fluid. Visible brain spaces on magnetic resonance imaging are often a normal finding, but they have also been associated with a wide range of neurological and systemic conditions, suggesting their potential as early indicators of intracranial pressure and neurofluid imbalance.
- perivascular spaces
- paravascular spaces
- Virchow–Robin spaces
- PVS
- glymphatic system
- neurofluids
- magnetic resonance imaging
- MRI
1. Introduction
2. Anatomy
The anatomy of PeVS and PaVS is intricate and remains a matter of debate. In humans, the cortical surface of the brain and the intracranial perforating arterioles are covered by the pia mater [6][7][9,10]. Arterioles that traverse the base of the brain and enter the basal ganglia are enveloped by two layers of leptomeninges along their length, forming a space between them that communicates with the subarachnoid space [8][9][11,12]. Arterioles in the cortex and venules have a single leptomeningeal membrane that adheres closely to the vessel wall without an outer layer, permitting that the spaces surrounding these vessels communicate with the subpial space directly and, somehow, indirectly with the subarachnoid space [10][11][12][13,14,15]. These spaces can be defined as PaVS and correspond to the “Virchow–Robin spaces”. They are bound internally by the pial sheath and externally by the basement membrane of astrocytes (glia limitans) on the arterial side and the vein wall and the glia limitans on the venous side [13][14][16,17]. The glymphatic model suggests that CSF flows through para-arterial spaces, interacts with interstitial fluid and solutes, and then is removed from the brain through para-venous spaces [15][18]. There are also other spaces within the arterial tunica media, located between the middle layers of the basement membrane of arterial smooth muscle cells [14][17]. These structures are called PeVS, and they serve as channels for interstitial fluid flow in the opposite direction to that of blood flow (also known as the intramural periarterial drainage pathway) towards the cervical lymph nodes through major cerebral arteries in the neck [13][16][16,19]. The venous vasculature does not contain PeVS [14][17]. In summary, PeVS are spaces around the blood vessels (between the basement membrane of the pial sheath and the basement membrane of the arteries), while PaVS are spaces alongside the blood vessels (outside the vessel wall) (Figure 1).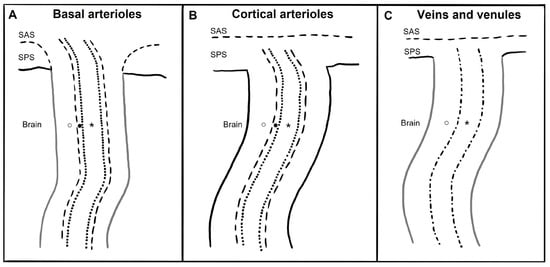
3. Imaging
4. Quantification
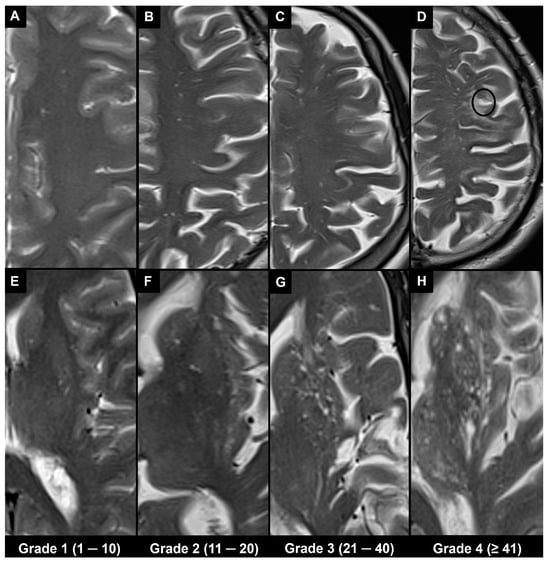
4.1. Visual Scoring
4.2. Automatic and Semi-Automatic Segmentation and Morphometry
Advances in technology have led to the emergence of various automatic and semi-automatic methods for segmenting and quantifying PVS. Once the PVS are segmented, various metrics and morphological features can be computed from segmentation masks [20][39][24,52]. The PVS volume is an indicator of the amount of fluid within the PVS [29][33]. The mean cross-sectional diameter can be utilized to differentiate PVS from other cerebral small vessel disease-related lesions [40][53]. Linearity represents the similarity of a particular PVS cluster to the tubular morphology [41][54], while solidity reflects the shape complexity of PVS, where a lower solidity indicates a more tortuous and less compact shape [20][24].5. Associations
5.1. Physiological
It is widely known that the visibility of PVS increases with age, especially in the basal ganglia, centrum semiovale, and hippocampus [42][66]. A recent study documented low PVS volumes in the basal ganglia and centrum semiovale in healthy subjects up to the age of 35 despite high Potter visual scores in the white matter of young subjects; also, it was suggested that in the basal ganglia, a Potter grade 1 and a Potter grade 3 could be considered physiological until the age of 50 and from the age of 70 onward, respectively, while in the centrum semiovale, a Potter grade 4 could be considered physiological from the age of 50 [43][67]. A higher PVS burden has been associated with the male sex, and it is also seen in healthy adolescents [29][44][33,65]. A circadian dynamic nature of the amount of MRI-visible PVS (higher PVS burden is visible on MRI at later times of the day) with a predominantly asymmetric distribution has been suggested. This could be associated with circadian fluctuations in respiration or/and blood pressure (which are known regulators of perivascular flow) or may be linked to the circadian control of flow through aquaporin-4 (a water channel that facilitates fluid transport from the PVS to the cerebral parenchyma) [29][33].5.2. Pathological
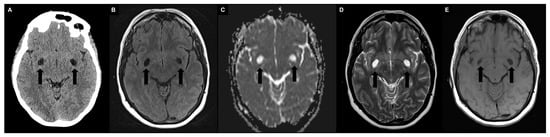
It is widely known that the visibility of PVS in the basal ganglia (but not in the centrum semiovale) increases with hypertension [42][66], and hypertension was found to be related to a low DTI-ALPS index [45][70]. Historically, MRI biomarkers of cerebral small vessel disease have included enlarged PVS along with other indicators such as recent small subcortical infarcts, lacunes, white matter hyperintensities (WMH) of presumed vascular origin, cerebral microbleeds, and brain atrophy, which are often present in association with stroke or cognitive decline.6. Differential Diagnosis
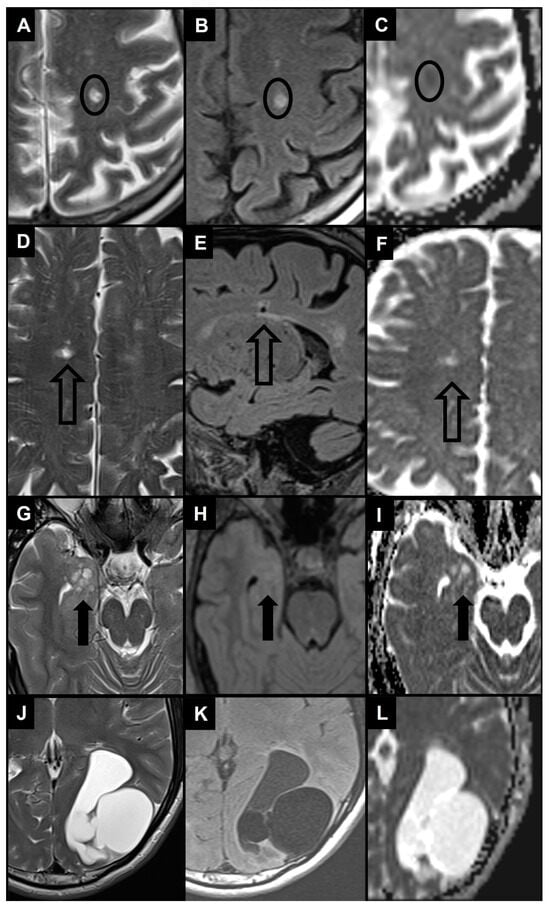
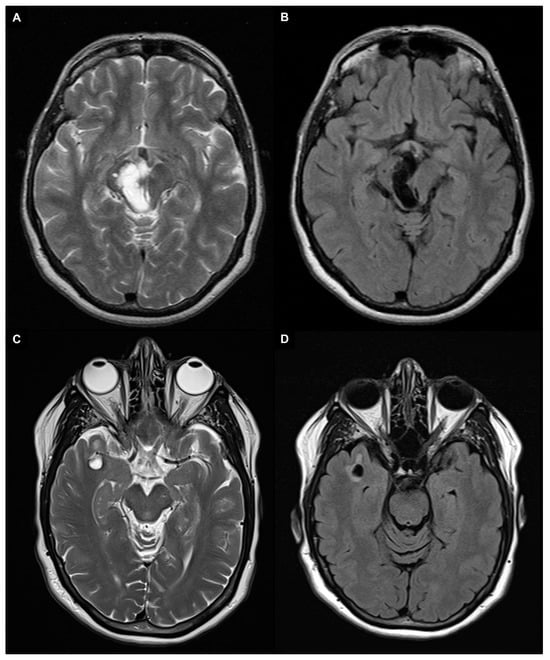
Enlarged PVS (diameter between 3–5 and 15 mm) most frequently need to be differentiated from lacunes and WMH as they are similar in signal characteristics and they often coexist in the context of cerebral small vessel disease (Figure 5A–F) [25][46][29,104]. When PVS appear notably enlarged (e.g., giant PVS with diameter ≥ 15 mm), causing mass effect, and presenting cystic configurations, they must be distinguished from other cystic pathologies of possible congenital, vascular, inflammatory, neoplastic, or hereditary nature (Figure 5G–L) [47][48][105,106].