1. The Mechanisms of Immunotherapies against SUDs
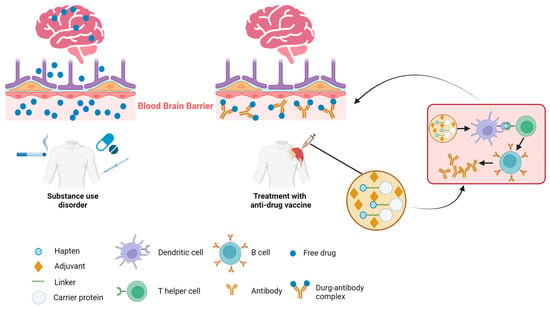
Potential detrimental effects of SUDs on various organ systems have been observed, with the most significant impact being on the central nervous system (CNS). Given the CNS’s inherent vulnerability to the adverse effects of drug abuse, immunotherapy emerges as a particularly effective therapeutic approach for addressing drug addiction, particularly when the CNS is involved. There are two key mechanisms underlying the effectiveness of immunotherapy for CNS-mediated drug addiction (
Figure 1). The initial mechanism centers on the binding of drug molecules to antibodies, which are too large to pass through the blood–brain barrier (BBB) and penetrate into the brain. This action decreases the amount of free drug circulating and hampers the drug’s interaction with brain receptors, thereby mitigating its effects such as addiction, respiratory depression, and bradycardia. The secondary mechanism is characterized by decelerating the rate at which abused drugs reach the brain
[1][32]. Antibody–drug binding has been shown to increase the half-life of the target drug. This is attributed to that the drug, once bound to the antibodies, becomes protected from enzymatic degradation. Consequently, this reduction in the drug’s clearance from the body results in an extended presence of the drug–antibody complex in circulation. This prolongs the period during which the drug is sequestered and prevented from interacting with its targets, such as receptors in the brain or other organs, thereby attenuating the pharmacodynamic effects of drugs
[2][33]. Together, these mechanisms contribute to the vaccine’s ability to counteract ongoing drug overdose or diminish the reinforcing effects of the drug. By leveraging these mechanisms, immunotherapy holds a promise as a strategy to mitigate the impact of drug addiction, particularly when the CNS is significantly impacted. Further research is essential to refine and validate these mechanisms and their therapeutic potential.
Figure 1. Mechanism of action of anti-drug immunotherapies. Multiple routes of addictive substance uptake into the body leading to drug transmission across the blood–brain barrier and subsequent interaction with brain (left). Intramuscular administration of a vaccine comprising the hapten conjugated to a carrier protein and adjuvants elicits an antibody response against the targeted drug. The presence of antibodies prevents the target drug from crossing the blood–brain barrier into the brain, thus mitigating the drug’s effects in the brain (right).
2. Recent Progress in Anti-Drug Vaccine Research
2.1. Opioid Vaccines
Prescription opioid (PO) pain relievers constitute the cornerstone of modern pain management therapy. However, they also rank among the most frequently misused and abused medications, such as oxycodone, hydrocodone, and especially fentanyl (the wave of overdose deaths attributed to illicit fentanyl since 2013 is unprecedented)
[3][4][2,46]. Traditional pharmacological therapies, such as the mu-opioid receptor (MOR) agonists methadone and buprenorphine, have been useful in treating opioid dependence
[5][6][47,48]. Additionally, MOR antagonists like naltrexone and naloxone are effective in reversing opioid overdoses
[7][49]. However, these medications have not been fully successful in addressing the alarming increase in opioid abuse in recent times. Moreover, they can be associated with significant side effects, limiting their overall effectiveness and acceptance in some cases
[8][9][50,51]. A vaccine-mediated pharmacokinetic strategy could combat the deadly and addictive effects of opioids. This approach involves using a small-molecule-immunogenic protein conjugate to trigger the production of drug-specific IgG antibodies. These antibodies can then attach to freely circulating opioid molecules, preventing them from entering the central nervous system (CNS) and inducing activation of the MOR
[10][52]. The vaccination using an oxycodone hapten containing a tetraglycine linker at the C6 position conjugated to keyhole limpet hemocyanin (6OXY(Gly)4–KLH) has produced notable effects in relation to increasing drug binding, reducing drug distribution, and blunting analgesia for both oxycodone and hydrocodone
[11][12]. The oxycodone vaccine (Oxy(Gly)4-sKLH) will be tested in participants with opioid use disorder (OUD). Its Phase I and II clinical trials will be completed this year (NCT04458545)
[12][11]. Indeed, prior research has demonstrated that TT, native keyhole limpet hemocyanin (nKLH), and GMP-grade KLH dimer (dKLH) carriers provide consistent oxycodone derivatized at the C6 position (6OXY) conjugate vaccine immunogenicity and attenuate oxycodone-induced hotplate antinociception
[13][53]. OXY-dKLH also effectively diminished oxycodone-induced respiratory depression and heart rate hold, which are significant implications in addressing the opioid overdose crisis
[10][52]. The synthesis of oxycodone-TT (Oxy-TT) and hydrocodone-TT (Hydro-TT) vaccines was successfully accomplished. A recent study has conclusively demonstrated that Oxy-TT and Hydro-TT vaccines effectively reduce mortality resulting from lethal doses of hydrocodone and oxycodone
[14][13]. This finding highlights the potential of active vaccination as a viable approach to combat the ongoing prescription opioid overdose epidemic.
Due to the fact that synthetic opioid-related (predominately illicit fentanyl and fentanyl analogs) overdose rose dramatically from 2014 to the present
[15][16][54,55], the development of novel therapeutics is a public health priority. Indeed, fentanyl vaccines have shown promising effects in preclinical studies, particularly in providing protection against overdose and mitigating the analgesic and respiratory effects of fentanyl in rhesus monkeys
[17][18][56,57]. In addition, a conjugate fentanyl-TT vaccine significantly blunted fentanyl reinforcement and prevented the expression of withdrawal-associated increases in rats
[19][14]. Given the evolution in drug supply over time, including increased synthesis of fentanyl analogs, a successful vaccine must demonstrate efficacy for fentanyl and related compounds, which may complicate development. In a preclinical animal study, FEN-CRM + dmLT (a fentanyl-like hapten was combined with the carrier protein CRM197 and an adjuvant derived from heat-labile enterotoxins from
E. coli (LT) named dmLT) generated significant amounts of anti-fentanyl antibodies that were associated with a significant blockade of fentanyl’s analgesic effects in mice. In the meantime, cross-reactivity assays demonstrated that anti-fentanyl antibodies exhibit binding affinity to fentanyl and sufentanil, while displaying no binding interaction with morphine, methadone, buprenorphine, or oxycodone
[20][15]. In another study, Carfen-ester-TT (the methyl ester functional group of carfentanil as the point of linker attachment) and Carfen-p-phenyl-TT (positions the linker at the para position of the phenethyl ring) can effectively target fentanyl and carfentanil, eliciting high-affinity antibodies against both drugs in mice
[21][58]. These results indicated a specific recognition and binding capacity of the antibodies to fentanyl-related compounds, supporting the targeted nature of the vaccine against these opioids. Recently, the incorporation of synthetic toll-like receptor (TLR) 7/8 agonists as vaccine adjuvants increased vaccine efficacy against fentanyl challenge, overdose, and self-administration in mice, rats, or Hanford miniature pigs
[22][23][59,60]. The development of opioid immunotherapies poses significant challenges. However, as the opioid crisis continues to persist, the pressing need for novel treatment approaches in the face of the enduring fentanyl overdose crisis is undeniable. An anti-fentanyl vaccine emerges as a promising avenue, offering a potentially innovative treatment and risk-mitigation strategy for overdose. Importantly, this approach may have a broader applicability to a larger target audience when compared to currently available interventions.
Heroin is a potent and highly addictive opioid drug that poses significant risks to individuals and public health
[24][61]. In the treatment of heroin abuse, long-acting oral opioid agents are often employed to provide a controlled and stable replacement therapy, such as methadone, levo-acetylmethadol (LAAM), and buprenorphine. These medications are used as part of medication-assisted treatment (MAT) approaches and work by mimicking drug action at the opioid receptors, which helps to alleviate cravings and withdrawal symptoms. Naltrexone and naloxone are other medications commonly used as pharmacotherapies for both abstinence and prevention of relapse in heroin addiction and OUD treatment. There are obvious deficiencies in both drug mimicry and drug antagonism. MAT may expose individuals to opiates, leading to tolerance and withdrawal from the treatment agent. Naltrexone and naloxone do not remain inactive in the absence of exogenous opioids. Instead, they actively block the binding of both exogenous opioids (e.g., heroin) and the body’s endogenous opioids (e.g., enkephalins and endorphins) to opioid receptors in the brain and other parts of the body causing negative emotional effects in the long-term treated patient. The first studies to provide the proof of concept for the use of active vaccination for treating heroin dependence were by Bonese et al.
[25][62]. However, this approach was ultimately abandoned due to apprehensions that individuals might readily transition to other opioids. Heroin is a prodrug, which means that it undergoes chemical transformations in the body to form active metabolites. It rapidly undergoes deacetylation, converting it into two primary metabolites: 6-acetylmorphine (6 AM) and morphine. The early report of a 6 AM-like hapten known as morphine-6-hemisuccinyl-bovine serum albumin (M-6-H-BSA) was explored 50 years ago by Bonese et al.
[25][62]. Subsequently, Anton et al. developed a morphine-tetanus toxoid (M-TT) vaccine, which has shown the capability to elicit a strong and long-lasting immune response against heroin
[26][16]. A similar vaccine utilizing 6-succinylmorphine conjugated to BSA (M-6-S-BSA) could generate high-titer anti-morphine antibodies with satisfactory specificity
[27][17]. Due to the fact that morphine is another component of the heroin metabolite, the utilization of a morphine-based hapten linked to KLH (M-KLH) has been shown to have the potential advantage of multivalent opioid vaccines. M-KLH could induce substantial levels and concentrations of antibodies with a strong affinity for heroin, 6-AM, and morphine and reduce brain 6-AM and morphine concentrations
[28][18]. M-KLH could also effectively prevent the heroin-primed reinstatement and reduce heroin-induced locomotor activity
[29][30][63,64]. Subsequently, a first-generation heroin vaccine based on two heroin- and morphine-like haptens exhibited blocked antinociceptive effects of heroin and inhibited acquisition of heroin self-administration
[31][65]. KLH-6-SM (keyhole limpet hemocyanin-6-succinylmorphine) is regarded as a candidate vaccine for opioid dependence depending on its ability to produce antibodies that show specificity for morphine or other heroin metabolites
[32][19]. A significant leap forward was made in a second generation heroin vaccine, which has been identified through optimization of the adjuvant (CpG ODN + alum), carrier protein (TT) and hapten (HerCOOH), achieved a greater than 15-fold heroin ED50 shift in rodents and mitigated heroin-induced decreases in operant responding in non-human primates
[33][66].
2.2. Nicotine Vaccines
Tobacco use disorder stands as the primary cause of both disease and preventable fatalities globally. Nicotine, a psychoactive ingredient naturally present in tobacco, functions as an agonist for nicotinic acetylcholine receptors and leads to escalation and compulsive-like pattern of smoking. Quitting smoking without medical interventions can be a challenging and often very difficult endeavor for smokers
[34][71]. An effective approach for addressing tobacco use disorder involves diminishing the psychoactive impact of nicotine by impeding its access to the brain. Early preclinical studies suggest that immunization results in ~30–90% less nicotine entering the brain after acute nicotine exposure and slows nicotine elimination from the body, which may contribute to reduction in smoking
[35][72].
In the early 21st century, some Phase II clinical trials have failed due to side effects (such as flu-like symptoms, injection site pain, headache, and so on) or inadequate antibody titers
[36][22]. Nabi Biopharmaceuticals has reported encouraging outcomes from Phase II trials of NicVAX. The NicVAX vaccine exhibited a favorable safety profile and was well-tolerated by participants. Notably, the vaccine prompted the production of elevated levels of anti-nicotine antibodies
[37][73]. A clinical study demonstrated that immunization using NicVAX led to a significant decrease in β2*-nicotinic acetylcholine receptor (β2*-nAChR) occupancy by nicotine. This effect was achieved by trapping nicotine in the bloodstream and subsequently reducing its passage into the brain
[38][20]. This strategy could potentially facilitate a gradual reduction in dependence, resulting in decreased cravings and thwarting relapse prompted by nicotine re-exposure. However, Phase III trials demonstrated identical rates of abstinence between active and placebo vaccine conditions
[39][40][74,75]. More efforts to achieve this pharmacokinetic goal through vaccines have been undertaken
[41][76]. A novel nanoparticle (NP)-based nicotine vaccine (NanoNicVac) was developed
[42][23]. Thereafter, various novel nicotine vaccines were developed according to the density and location of haptens
[43][44][77,78]. The strategic integration of toll-like receptor (TLR) adjuvants increased total anti-nicotine IgG titers, affected IgG subtype distribution in mice, and reduced the brain nicotine levels in mice after nicotine challenge. Such design has the potential to amplify the immunological effectiveness of the hybrid nanoparticle-based nicotine vaccine
[45][79]. It was observed that a nicotine vaccine containing 20% PEGylation (referred to as NanoNicVac 20.0) exhibited notably higher stability in comparison to vaccines with lower levels of PEGylation. The inclusion of 20% PEGylation in NanoNicVac appears to confer on the vaccine a favorable combination of enhanced safety, superior stability, and heightened immunological effectiveness in mice
[46][80]. FH VLPs (FljB was displayed at high densities on hepatitis b core (HBc) virus-like particle (VLP) surface upon c/e1 loop insertion) were found to be a more immunogenic carrier than the widely used keyhole limpet hemocyanin for nicotine vaccine development with good local and systemic safety
[47][24]. Recently, Hu lab developed two nicotine vaccines using lipid-poly (lactic-co-glycolic acid) (PLGA) and lipid-polylactic acid (PLA) hybrid nanoparticles, respectively. It was observed that the lipid-PLA-based nicotine vaccine (referred to as PLA vaccine) exhibited significantly enhanced stability compared to the lipid-PLGA-based nicotine vaccine (referred to as PLGA vaccine) in both in vitro and in vivo settings. However, mice immunized with either the PLA vaccine or the PLGA vaccine alone did not achieve sufficiently high concentrations of long-lasting nicotine-specific antibodies. Interestingly, mice that were initially administered two injections of the PLGA vaccine, followed by a subsequent third injection of the PLA vaccine, demonstrated elevated concentrations of nicotine-specific antibodies persisting for up to three months
[48][81]. Intranasal immunization with a Nic-KLH/MPL vaccine can induce systemic and mucosal antibodies that specifically neutralize nicotine
[49][82]. Therefore, for these attempts to be successful, antibody titers must be sufficient to effectively block nicotine’s entry into the brain.
Another crucial point to consider is that many animal models used for vaccine studies entail the intravenous or subcutaneous administration of nicotine in isolation. This methodology significantly diverges from the real-world scenario of nicotine inhalation, tobacco consumption, and exposure to the multitude of chemicals found in cigarettes that humans experience. Indeed, antagonizing the effects of nicotine has shown promise in conjunction with varenicline, considered the most effective smoking cessation treatment available. Animal studies, especially in rats across laboratories and across specific vaccine compounds, have indicated that immunization leads to reduced nicotine penetration into the brain and diminished behavioral responses to nicotine, including locomotor effects
[50][51][83,84]. However, the limited published human studies exploring various nicotine vaccines have not yet provided substantial evidence supporting vaccine efficacy as a treatment for nicotine dependence. To date, five nicotine vaccines have been tested across 16 Phase I–III clinical trials. However, due to insufficient anti-nicotine antibody production, insufficient specificity or affinity of antibodies produced from vaccination and high individual variability in antibody titer concentration post-vaccination, the expected results were not obtained
[36][52][53][21,22,85]. Further research and clinical trials are needed to comprehensively assess the potential of vaccine-based treatments for nicotine dependence in humans.
2.3. Cocaine Vaccines
Cocaine, a highly addictive substance, necessitates innovative approaches for combating its abuse. Target based small-molecule approaches have not yielded highly effective medications to treat SUDs. Thus, pharmacotherapies, aimed to modulate or disrupt the drug’s effect at its site of action, have yet to be approved for the treatment of cocaine dependence. The direction of treatment shifts to the drug itself. Developing an active immunization against cocaine presents a potential solution by impeding the drug’s entry into the CNS, thereby obstructing its effects. To effectively intercept nearly all target drug molecules before they reach the blood–brain barrier, the antibody concentration in the bloodstream must be sufficiently high. Moreover, in order to maintain vaccine efficacy, it is crucial for this antibody level to remain consistent over a certain duration
[54][7]. Importantly, such an approach is anticipated to yield fewer side effects compared to treatments focused on altering central neurotransmitter activity.
The first reported anti-cocaine vaccine used unmodified cocaine as a hapten, conjugated to the surface of the cholera toxin B (CTB) subunit protein and co-administered with an alum adjuvant. It elicited a robust antibody response and hindered the pleasure associated with cocaine use
[55][86]. Exploration of three rhesus monkeys immunized with a different cocaine vaccine (bovine serum albumin conjugate in alum) indicated that the immune response could induce a specific pharmacokinetic shift in cocaine distribution, effectively counteracting a behavioral response to the drug
[56][87]. The route of administration may also be a factor affecting vaccine immunity. The presence of cocaine-specific antibodies in the mucosal lining after intranasal immunization might play a crucial role in impeding the direct entry of cocaine into the brain through the olfactory bulb. A cocaine vaccine combined with M7-NH2, a mucosal adjuvant and mast-cell-activating oligopeptide, could enhance cocaine-specific antibodies in mucosal secretions compared to the traditional adjuvant
[57][88].
2.4. Methamphetamine Vaccine
Methamphetamine (METH), an illicit psychostimulatory phenethylamine, induces a profoundly addictive and euphoric high by modulating monoamine neurotransmitter systems and increasing extracellular dopamine levels in the brain. Due to the involvement of multiple monoamine neurotransmitters, there are no established pharmacotherapies, namely receptor modulations, for the treatment of METH use disorder or overdose reversal at present. Therefore, researchers should utilize the field of immunopharmacotherapy with the aim of creating an active vaccine for METH. However, no MA vaccines have yet advanced to clinical trials.
Several preclinical studies have investigated the effectiveness of METH vaccines, yielding relatively promising outcomes. The initial active anti-METH vaccine did not produce a significant therapeutic effect. Then three haptenic compounds, MH2(R), MH6, and MH7, have been shown to produce antibodies with a high affinity and concentration capable of capturing the drug in the bloodstream
[58][97]. Among these, MH6-KLH could block METH-induced locomotor and thermoregulatory disruptions in rats, exhibiting notable potential for developing a potentially significant METH vaccine
[59][29]. Phenyl-substituted meth haptens have also been documented as active vaccination agents, such as SMO9. Repeated immunization with a high dose of SMO9-KLH did not result in any adverse effects on health, body weight, or performance during food-maintained behavioral testing. The antibodies generated by the SMO9-KLH vaccine were effective at sequestering METH in the bloodstream and prevented rats from METH-induced impairment of food responses
[60][30]. Additional endeavors in the development of METH vaccines involve the utilization of a succinyl methamphetamine hapten (SMA)–KLH conjugate formulated with MPLA, which demonstrated a reduction in METH-induced locomotor effects in mice
[61][98]. The SMA-TT vaccine attenuated acquisition and reinstatement of MA place conditioning. Furthermore, in vaccinated mice, the levels of METH in the brain were observed to decrease after the administration
[62][63][31,99]. Despite the encouraging preliminary results, no methamphetamine vaccines have advanced to human clinical trials at this point.