Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by MASSIMO BONUCCI and Version 2 by Sirius Huang.
Multiple Myeloma (MM) is the second most prevalent hematologic malignancy, and its incidence has been increasing enormously. The prognosis of MM has changed radically with the introduction of new drugs that have improved life expectancy; recurrences are a common occurrence during the course of the disease and are characterized by an increase in refractory to treatment. Moreover, MM patients are challenged by quality of life-related concerns while limited conventional therapy may be offered. This includes bone pain and dialysis due to the complications of acute renal failure.
- Multiple Myeloma
- nutrition
- acupuncture
- vitamin D
- supplementation
- integrative medicine
1. Introduction
The last few years were characterized by a significant improvement in available therapies for this disease, including new-generation immune modulators and proteasome inhibitors (PIs), monoclonal antibodies, or immunotherapy (bispecific T-cell engagers or Chimeric Antigen Receptor T cell therapies, so-called CAR-T) [2].
Following this progress, the median overall survival has more than tripled [2]. However, MM is still an incurable disease and has become a chronic condition with patients experiencing many symptoms related to the disease itself or its treatment, which impacts health-related quality of life (QoL) [4][5][6][7][4,5,6,7]. These include pain, fatigue, sexual dysfunction, sleep disorders, immune deficiency, anxiety, depression, and/or loss of control [5][6][7][8][5,6,7,8], making patients with MM the most symptomatic in the haemato-oncologic field [9]. In the last few years, Integrative Oncology (IO) has been developed, and subsequently, Integrative Hematology (IH) was defined as a separate entity [10]. IO is a “patient-centered, evidence-informed field of cancer care that utilizes mind and body practices, natural products, and/or lifestyle modifications from different traditions alongside conventional cancer treatments, and aims to optimize health, QoL, and clinical outcomes across the cancer care continuum” [11].
Specifically, in the case of MM, patients have been shown to use complementary and alternative medicine widely but, generally, without informing their hematologist [12], potentially leading to safety issues [13]. The integrative approach to the treatment of myeloma therefore has many objectives: firstly, a reduction in disease-related symptoms such as bone pain, which is very detrimental to the patient’s life [9][14][15][9,14,15]; and a reduction in treatment side effects, allowing greater compliance to them as well as greater effectiveness. Another goal is to reduce the toxicity of drugs and improve the performance of the immune system. A patient with MM has many unmet needs, and a patient-centered approach, which includes mind–body techniques, can help to better manage the disease and therapies.
2. Natural Compounds and Vitamins: Their Potential Role in the Treatment of MM
2.1. Curcumin
Curcumin (diferuloylmethane), the main bioactive component of Turmeric (curcuma longa), has demonstrated anti-inflammatory, antibacterial, and anticancer in vitro effects against many cancer cell lines [16][43]. In MM, its action is expressed both by affecting specific signaling pathways and with an epigenetic modulatory effect. Among the various effects, Nuclear factor kappa B (NFκB) inhibition appears to be particularly important in this disease: one of the backbones of MM therapy is, in fact, constituted by PIs, which cause NFκB inhibition. This would suggest a possible hypothetical interaction between curcumin and PIs. In vitro, curcumin has been shown to enhance the cytotoxic effect of bortezomib (the first PI) [17][44]; it also synergizes with carfilzomib through a major downregulation of NFkB [18][45]. Curcumin was also reported to downregulate the expression of cyclin D1, inhibit STAT3 phosphorylation, and reduce IL6, even in patients with unfavorable cytogenetics and regardless of Tumor Protein 53 (TP53) status: this sensitivity to curcumin is also present both in the cells of patients at diagnosis and at recurrence, demonstrating that resistance phenomena do not occur [19][20][46,47]. Finally, it inhibits osteoclastogenesis by inhibiting RANKL [21][48]. The main reason for the incurability of MM could be related to the presence of cancer stem cells (CSCs): they confer treatment resistance and are associated with recurrence and poor prognosis. Recently, curcumin has been demonstrated to be efficient against these cells, increasing apoptosis [22][49]. As an epigenetic modulator, curcumin also appears to act in MM by inducing DNA methyltransferase (DNMT)-mediated mTOR methylation: hypermethylation of the mTOR promoter region would inhibit the antiapoptotic action of this molecular pathway [23][50]; unlike the hypomethylating drugs used in hematology, such as azacitidine, curcumin would not cause an overall change in DNA methylation but only the specific one caused by DNMT3a and DNMT3b, and this could give it more peculiar anti-myeloma activity. Finally, in some mouse models, it increases chemosensitivity to dexamethasone, doxorubicin, and melphalan and synergizes not only with the action of bortezomib and carfilzomib but also with immunomodulatory imide drugs (IMiDs) such as lenalidomide and thalidomide [24][51]; synergy with lenalidomide is expressed through the suppression of the cereblon gene, which is exactly the target of the IMiDs. However, the literature on the association of these promising in vitro effects with effective clinical action is presently limited. The first study, published in 2009, involved 26 patients with MGUS treated with 4 g daily of curcumin; in this study, the monoclonal component decreased in 50% of patients, in keeping with a reduction in markers of bone resorption [25][52]. Following, the authors published a randomized double-blind placebo-controlled trial in both MGUS and smoldering myeloma: they used curcumin in doses of 4 and 8 g daily, and this led to a reduction in the chain k/λ ratio by 35 and 36%, respectively, as well as the markers of bone resorption [26][53]. As not all cases of MGUS and smoldering myeloma evolve into frank disease, the use of conventional chemotherapy is not justified in these cases; precisely for this reason, supplements such as curcumin express all their chemopreventive potential in this phase of the pathogenesis of the disease. In this regard, Zaidi et al. [27][54] published a case study in which curcumin (8 g daily) was associated with hyperbaric sessions that led to disease control in a case of refractory relapsed MM for 60 months, with an excellent safety profile. A more recently published case study reported the efficacy of curcumin in replacing dexamethasone in patients who were intolerant to the latter. The authors treated 15 patients who were under treatment with regimens containing either IMiDs or PI combined with dexamethasone, substituting the latter with C3 complex curcumin at a dosage of 3–4 g daily. The researchers concluded that curcumin may act as a steroid-sparing agent in patients with MM who are intolerant of dexamethasone, with an excellent tolerability profile [28][55]. These data are exciting considering that in MM, we often use therapeutic regimens, if effective, up to progression; if these medications, as often happens, contain cortisone, the patient is frequently subjected to massive and prolonged doses of steroids and their heavy long-term side effects. Even with the aim of reducing steroid load and toxicity, curcumin is, therefore, an engaging weapon to take into consideration. Finally, a pilot randomized trial was conducted [29][56] in which 33 newly diagnosed patients, ineligible for transplant, were randomized to receive melphalan 4 mg/m2 plus prednisone 40 mg/m2 for 7 days and curcumin 8 g/daily for 28 days or placebo for 4 cycles. Curcumin-treated patients showed a higher treatment response rate (75% vs. 33.3%) with a contextual reduction in NF-κB, IL-6, VEGF, and TNF-α levels. These few but promising results emphasize the need for more well-designed clinical studies to explore the potential additive healing effect of curcumin, as well as to identify the type of biochemical form most available (e.g., extract, liposomal, and water-soluble form).2.2. Epigallocatechin Gallate (EGCG)
EGCG has shown an antiapoptotic effect on MM cells in vitro through the stimulation of ROS and a reduction in the levels of peroxiredoxin (an antioxidant molecule); moreover, a crucial role is played by the selective interaction with the laminin 1 receptor, which is much higher in patients with MM than in controls and whose absence prevents the apoptotic effect of EGCG [30][57]. Other mechanisms involve the inactivation of the enhancer of zeste homolog2 (EZH2) and the mitochondrial apoptosis pathway [31][58]. Although the in vitro antitumor efficacy of EGCG in MM is undisputed, its in vivo role and, in particular, its interaction with bortezomib, a backbone of the induction therapy, is controversial. In 2009, two contradictory studies were published in this regard. Golden et al., demonstrated that EGCG and other polyphenols derived from green tea prevented tumor cell apoptosis induced by bortezomib in vitro and in vivo at concentrations also easily achievable in humans: the antagonistic action of EGCG was evident only with boronic acid-based PIs, so the binding with the boronic acid of the molecule appears to be the mechanism underlying this inhibitory mechanism [32][59]. In the second work, however, a synergistic effect between the two substances was demonstrated, and this would be due, in the opinion of the authors, to the higher dosage of EGCG and bortezomib used [33][60]. The discrepancy of these data, the lack of clinical studies, and the possible difference between what happens in vitro and what occurs in vivo due to certain variables such as absorption and bioavailability impose a prudent attitude, especially until well-designed clinical trials are available. Some more recent studies affirmed again the antagonism between the two substances [34][35][61,62]; in particular, Qiu et al. [35][62] have shown that EGCG may neutralize bortezomib-induced apoptosis, activate Wnt/β-catenin signaling, and result in the accumulation of beta catenin, which subsequently activated c-myc and cyclin D1. The authors conclude by discouraging green tea intake during bortezomib therapy. Finally, EGCG is very interesting for its action on glutaminolysis: MM cells have a glutamine addiction, which is responsible for their dependence on glutamine uptake. In a recent study [36][63], Li et al., showed that the combination of EGCG and telaglenastat, a glutaminase inhibitor, synergistically inhibits proliferation and induces apoptosis in MM cells in vitro. Targeting glutamine metabolism, therefore, should be a winning strategy.2.3. Vitamin D
Vitamin D deficiency is found in most patients with MM at diagnosis, as in many other types of cancer. This deficit is described as “alarming” in patients with bone involvement [37][64]. Even some peculiar polymorphisms of the vitamin D receptor (VDR) gene may be a molecular marker of the risk of development of the disease [38][65]. Low levels of vitamin D correlate with an increased C-reactive protein (CRP) and the ISS stage at the time of diagnosis: they may, therefore, be predictive of more advanced disease [39][66]. It is very interesting to observe how the action of some drugs used in MM also passes through the modulation of the molecular pathway of vitamin D: bortezomib, for example, upregulates the production of VDR, and this effect is amplified in the presence of vitamin D. Thalidomide- or bortezomib-induced neuropathy is more severe in the case of concomitant vitamin D deficiency, which, however, does not appear to influence the incidence [40][67]. Vitamin D and its active metabolite, calcitriol, act as modulators of the immune system: absolute lymphocyte count recovery and relapse-free survival after ASCT are improved after daily administration of calcitriol of 0.25 μg, as shown in a randomized-controlled trial (RCT) vs. placebo [41][68]. Interestingly, vitamin D can increase CD38 expression in plasma cells, thereby amplifying the binding of CD38-targeting antibodies; however, the cytotoxicity of the latter could be compromised in case of vitamin D deficiency, which would cause a worse performance of the macrophages associated with myeloma (MAMs). Lenalidomide and pomalidomide can restore the vitamin D pathway in the MAMs, improving their cytotoxicity. In doing so, vitamin D becomes a crucial link to improve the synergy between immune modulators and monoclonal antibodies [42][69]. The above data may support the rationale to test vitamin D levels at diagnosis and supplement them before starting therapy and during treatment with anti-CD38 and immunomodulatory drugs. Noteworthily, vitamin D levels do not appear to be significantly associated with the coexistence of bone disease [43][70]. In Figure 1, the main mechanisms of action of the supplements most studied in the MM are presented.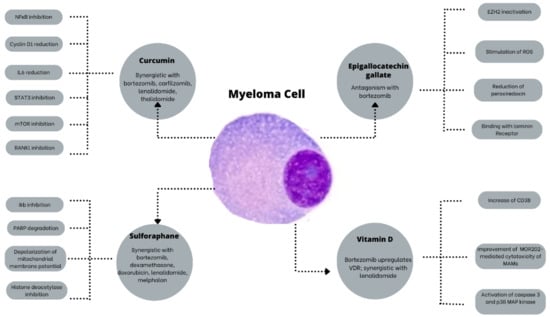
Figure 1. The main mechanisms of action of the most studied supplements in MM. EZH2: Enhancer of zeste homolog2; IkB: NkB inhibitor; IL6: interleukin 6; MAMs: Macrophages associated with myeloma; mTOR: Mammalian target of rapamycin; NfkB: Nuclear factor kappa B; PARP: poly ADP ribose polymerase; RANKL: Receptor activator of nuclear factor kappa-Β ligand; ROS: Reactive oxygen species; STAT3: Signal transducer and activator of transcription 3; VDR: Vitamin D receptor.
2.4. Others
Ascorbic acid can reduce Bortezomib-induced neurotoxicity by leading to the recovery of damaged Schwann cells; unfortunately, it has been shown to inhibit Bortezomib cytotoxicity in vitro and in vivo, so its supplementation in patients who are on treatment with this PI is not recommended [44][45][71,72]. Despite its importance for the immune cells, it is ineffective in improving bone marrow recovery after ASCT both in MM and lymphoma patients, so its use is not advised in this setting [46][73]. Sulforaphane is an isothiocyanate derived from cruciferous vegetables, which has been shown to have similar action to bortezomib in inhibiting the degradation of inhibitory kappa B kinases (IkB), which, in turn, inhibits the proteasome complex. Moreover, it shows synergy with dexamethasone, doxorubicin, bortezomib, and melphalan. In in vivo models, it leads to a reduction in the burden of disease and an increase in survival [47][74]. Resveratrol has shown strong antiangiogenic activity by regulating factors such as VEGF, matrix metalloproteinase-2 (MMP2), and matrix metalloproteinase-9 (MMP9). By constitutively activating STAT3 and NFκB, it overcomes an essential mechanism of chemoresistance and it has a synergistic interaction with Bortezomib and Thalidomide [48][75]. There is insufficient clinical evidence to understand the clinical efficacy of resveratrol. In a single phase II study, it was administered in association with bortezomib: in this clinical experience, the toxicity profile was unacceptable, with 50% of patients developing severe renal failure. To date, resveratrol in combination with bortezomib is strongly discouraged. Further studies are needed to clarify the safety of this natural compound in this setting of patients [49][76]. Cannabinoids are compounds found in plants from the genus Cannabis, of which the most widely used is Cannabis Sativa. In recent years, their role in managing the patient’s symptoms has emerged and they are used primarily to reduce chronic pain and chemotherapy-induced nausea and vomiting and stimulate appetite [50][77]. Since many different cell lines express CB1/CB2 receptors for cannabinoids, their anti-cancer potential has been extensively investigated recently, in in vitro and in vivo models: among the various plant components most studied for their antiapoptotic activity are delta-trans-9-tetrahydrocannabinol (THC) and cannabidiol (CBD), with the latter being free of psychoactive effects. In contrast to the in vivo and in vitro settings, clinical research is limited, though suggests good patient tolerability even at high doses, particularly in glioblastoma and MM [51][78]. In MM, in vitro studies have demonstrated reduced viability of myeloma cells and proapoptotic activity in cannabinoid-treated MM cells, including dexamethasone-resistant cells. Cannabinoids can reduce the expression of the β5i subunit of the immunoproteasome, therefore increasing the efficacy of carfilzomib, a second-generation PI. In addition, they allow resistance mechanisms effectively linked to the expression levels of β5i to overcome [52][79]. These compounds are, therefore, promising not only for improving the symptoms and QoL of patients, but also for their anticancer and synergistic activities with currently used drugs. Further studies are needed to confirm this promising action. Table 1 shows the potential use of the substances described above.Table 1.
Potential use of supplements or natural compounds in Multiple Myeloma.
| Substance | Dose | Potential Chemotherapy Interaction | References |
|---|---|---|---|
| Vitamin D | To reach blood levels >30 ng/ml | Synergism with lenalidomide, pomalidomide, anti-CD38 | [40][41][42][67,68,69] |
| Curcumin | 6–8 g daily or liposomal formulation | Synergism with bortezomib, carfilzomib, thalidomide, melphalan | [17][18][24][25][26][27][28][29][44,45,51,52,53,54,55,56] |
| Epigallocatechin 3 gallate | 1 g daily | Antagonism with bortezomib | [34][35][61,62] |
| Vitamin C | 6–8 g daily | Antagonism with bortezomib | [44][45][71,72] |
| Cannabinoids | ? | Synergism with carfilzomib | [52][79] |
| Sulforaphane | To be found | Synergism with dexamethasone, doxorubicin, bortezomib, and melphalan | [47][74] |
| Resveratrol | To be found | Antagonism with bortezomib; possible side effects, not recommended | [48][49][75,76] |
