Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Braden Vogt and Version 3 by Lindsay Dong.
Urgent-start peritoneal dialysis (USPD) is defined as peritoneal dialysis initiated within 14 days of catheter insertion.
- urgent-start peritoneal dialysis
- peritoneal dialysis
- dialysis
- implementation
1. Introduction
Hemodialysis (HD) remains the most common form of renal replacement therapy in the United States, accounting for over 85% of incident dialysis in 2020 [1]. However, peritoneal dialysis (PD) is equally efficacious and allows patients to dialyze at home, leading to increased independence and quality of life for patients [2][3][2,3]. Furthermore, due to decreased healthcare costs and infrastructure, many countries are creating incentives to increase the percentage of patients on PD [4]. However, these incentives have not always been effective, and compared to locations such as Hong Kong, New Zealand, and Thailand, the United States lags far behind in PD utilization [5]. While dialysis ideally occurs after months to years of pre-dialysis care, up to 33% of patients receive little to no nephrology care before dialysis, and up to 60% of dialysis is initiated unplanned [6]. Peritoneal dialysis is a viable option for patients initiating dialysis in an unplanned manner, even prior to catheter site maturation. Typically, the catheter is placed and remains unused for at least 14 days. When initiated prior to 14 days after catheter implantation, it is termed urgent-start peritoneal dialysis (USPD). Furthermore, the majority of patients who begin dialysis while in the hospital continue the same modality as outpatients [7]. Given that a high percentage of patients initiate dialysis unplanned and many patients continue the same modality in the hospital, expanding the use of USPD may increase the use in the outpatient setting, especially among those who originally elected for PD. In an effort to maintain PD as an option for patients in the outpatient setting, USPD has been studied to determine its efficacy, especially in comparison to planned PD and urgent-start hemodialysis (USHD).
2. Clinical Considerations in Urgent-Start Peritoneal Dialysis
2.1. Patient Selection Criteria for USPD
Prior to initiating USPD, the patient must first go through a thorough evaluation. The initial evaluation can be performed by a nurse, social-worker, nurse care manager, nephrology fellow, or attending nephrologist using a standardized questionnaire [8]. There are few absolute contraindications to PD, especially if PD is to be started immediately in the inpatient setting. Broadly, PD requires a peritoneal cavity free of significant scarring or adhesions, a clean environment where exchanges can occur, and the mental/physical ability to perform PD [9]. Although some urgent-start PD may begin in the hospital, it is often initiated in outpatients, and therefore, social factors must also be considered. Due to the risk of infection, a clean environment in a stable home is required [9]. Given the increased patient responsibility in PD, including performing self-exchanges, the patient must have a high degree of motivation for PD and health literacy. When this is not met, or the patient has cognitive impairment, a caregiver or family member must meet these qualifications. Among the most important aspects of patient selection criteria is patient preference. While education in the inpatient setting may be time consuming and logistically difficult, it facilitates shared decision making and is vital to patient selection in USPD [10]. Most patients who initiate dialysis as inpatients will continue the same modality as outpatients [7]. Therefore, some patients who originally elected for outpatient PD but received USHD as inpatients may continue without their preferred modality. This process is described in Figure 1.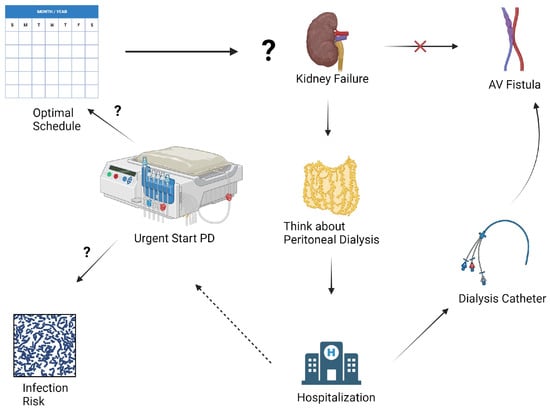
Figure 1. Rethinking Dialysis in the Urgent-Start Patient: Many patients elect for peritoneal dialysis in the outpatient setting but begin in an unplanned manner, often eventually receiving hemodialysis instead. Urgent-start peritoneal dialysis remains an understudied option to allow some of these patients to receive peritoneal dialysis in the outpatient setting. However, many clinical questions remain unanswered, including timing of initiation, terminology, and complications rates, such as infection and mechanical complications. Figure created with BioRender.com.
2.2. Timing of Initiation and Current Data Limitations
Conventional-start PD is defined as dialysis beginning 14 days or more after placement of a PD catheter. Given that a high percentage of patients require dialysis unplanned, the term “urgent start peritoneal dialysis” is applied to dialysis that begins prior to 14 days. However, recent literature has called for further dividing of USPD terminology, as some patients initiate PD within 24 h, while others begin after 13 days. Given the patients who require dialysis within 24 h are quite different from those who begin after 13 days, and there may be large differences in catheter site maturation, new definitions have been proposed. In 2018, Blake et al. proposed the terms “urgent start” for those who began within 72 h, and “early start” for those who began within 14 days [11]. Since publication, there has been an increase in literature that specifically separates these groups.2.3. Catheter Insertion Techniques
Multiple techniques are available to insert catheters for PD. These techniques can be performed both in inpatient and outpatient settings, and depending on the technique, can be implanted by different specialties. Techniques include open surgical, laparoscopic, interventional radiology-guided insertion, or percutaneously by nephrology. Among nonsurgical techniques, both fluoroscopy and ultrasound have demonstrated effectiveness [12][13]. Most commonly, a PD catheter is placed and secured using a double purse string technique.2.4. Peritoneal Dialysis Prescription and Modality Choices
When determining an initial PD prescription, there are various forms of PD a provider may choose. Given the concern for increased complications in USPD compared to conventional PD, investigators are interested in whether a certain prescription may decrease complications. Options include automated peritoneal dialysis (APD) and continuous ambulatory peritoneal dialysis (CAPD). Typically, patients receiving USPD will receive incremental PD (IPD) in which their prescription considers residual kidney function. One study of patients undergoing USPD compared APD and intermittent peritoneal dialysis (IPD) and showed that serum potassium and phosphorus were lower in the APD group, suggesting electrolyte clearance may be superior in APD [13][20].3. Outcomes and Efficacy of Urgent-Start Peritoneal Dialysis
3.1. Mechanical Complications and Technique Failure
Given most PD outcome data include patients who initiated PD after 14 days, clinical outcomes among those undergoing USPD are less well-defined. Mechanical complications such as catheter leaks and migrations are common in USPD. Rates of catheter leak at 30 days vary widely from 2.6% to 12% [14][15][16][25,26,27], and migration rates ranged from 2% to 12% at 30 days [14][15][16][25,26,27]. Overall catheter complications were also highly variable, with one study of 2059 patients reporting a 7.6% rate over a mean 36.5-month follow-up [17][28], compared to another study that showed a rate of 33.3% at 90 days [18][29]. Additionally, there is interest in determining if outcomes differ between conventional-start PD and USPD, and recent literature has investigated this relationship. The primary fear among patients who undergo USPD is increased mechanical complications, such as catheter dysfunction, and leakage, due to an immature site. Assuming the accuracy of this proposed mechanism, patients beginning with 72 h may have more mechanical complications than patients beginning with 14 days.3.2. Infectious Complications
Peritonitis is a common complication of PD [3]. There is interest in determining the approximate rate of peritonitis in USPD and whether it is different to conventional-start PD. Reported peritonitis rates at 30 days in USPD range from 0% to 8.6% [14][15][16][19][25,26,27,36]. Catheter site infection rates also vary widely from 0% to 12% [15][16][17][26,27,28]. One study of 310 diabetic patients found a 0.3% rate, while another smaller study of 26 patients found 12%, likely reflecting sample size differences. Additionally, one study found overall infectious complications to be 17% [20][38]. Although the crude rates were inconsistent, none of the studies demonstrated a statistically significant difference in peritonitis rates at 30 days when compared to conventional PD [14][15][16][21][22][24,25,26,27,35].3.3. Survival Rates and Patient Outcomes in USPD Compared to Other Modalities
.3. Survival Rates and Patient Outcomes in USPD Compared to Other Modalities
Studies have compared outcomes between USPD and USHD to guide modality selection. USHD has a significantly higher 30-day bacteremia rate (13.4–21%) than USPD (3.0–3.1%) [23][24][39,40]. One such study reported a higher mortality rate due to infection, although the trend was not significant (p = 0.11) [23][39]. A Cochrane review also found more bacteremia with USHD versus USPD [25][41]. While the available evidence suggests USHD has a higher rate of bacteremia, overall complications may also be higher. Overall dialysis complications in USPD at 30 days were reported as 4.5–5.7% in USPD, compared to 10.7–24% in USHD [24][26][27][40,42,43].3.4. Impact of USPD on Healthcare Utilization
The use of peritoneal dialysis is increasing in developing countries, partially due to potentially lower costs and infrastructure needs compared to hemodialysis. However, the impact of complications on costs in urgent-start PD is unclear. One study analyzed costs in the first 90 days for USPD versus USHD. Mean costs were lower with USPD (USD 16,398) versus USHD (USD 19,352), primarily due to lower access-related costs (USD 2492 for USPD versus USD 5227 for USHD) [28][46]. The higher USHD costs reflect initial catheter placement and subsequent permanent access creation. Patients starting with USHD then transitioning to PD had similar costs to USHD alone (USD 19,400) [28][46].4. Barriers and Strategies to Optimize Urgent-Start Peritoneal Dialysis
4.1. Multidisciplinary Approach and Team Collaboration
Implementing USPD presents logistical challenges including coordination across multiple specialties and ensuring adequate staff familiarity with the modality. A summary of barriers is presented in Figure 2. A standardized evaluation helps identify appropriate candidates, considering social support, medical history, and functional status [8]. Extensive patient education is required as PD relies heavily on patient involvement, presenting workflow challenges when initiating PD urgently in the inpatient setting. Nurses, physicians, dieticians, psychologists, and administrators play a critical role in a successful PD program. Adequate nurse staffing ratios are crucial, since nurses complete many USPD tasks and may lack familiarity compared to conventional PD initiation [8]. Involving nurses in USPD protocol development can optimize success [8]. Post-initiation, vigilant nursing care may reduce complications through early issue recognition and intervention. Timely catheter placement also remains a barrier, as operators are often less comfortable with PD versus HD catheters [29][48], and catheters must be placed as soon as possible to initiate USPD. Operating room implantation, while facilitating adhesiolysis, presents logistical hurdles. Percutaneous insertion by interventional radiology or nephrology allows for urgent bedside placement in uncomplicated cases [30][49].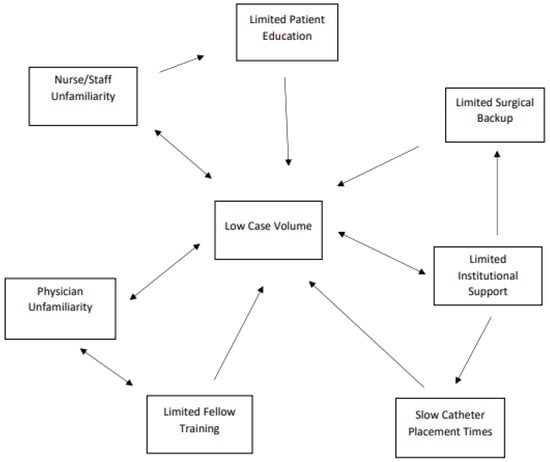
Figure 2.
Summary of interconnected barriers to urgent-start peritoneal dialysis implementation.
