Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Maria Isabel da Silva Santos and Version 2 by Jason Zhu.
While food markets and food production chains are experiencing exponential growth, global attention to food safety is steadily increasing. This is particularly crucial for ready-to-eat products such as fresh-cut salads and fruits, as these items are consumed raw without prior heat treatment, making the presence of pathogenic microorganisms quite frequent. Moreover, many studies on foodborne illnesses associated with these foods often overlook the transmission links from the initial contamination source. Here we overview the main pathogen sources in food contamination throught the food production chain in a One health perspective.
- minimally processed foods
- foodborne pathogens
- One Health
- fruits and vegetables food chain production
1. Minimally Processed Fruit and Vegetable Contamination
Minimally processed fruits and vegetables (MPFV) are not sterile products; instead, they undergo only a moderate decrease in the microbiota present during processing. As vegetables are raw agricultural products, MPFV will likely contain potentially pathogenic microorganisms [1][2][3][4][5][6][7][8][9][10][26,39,40,41,42,43,44,45,46,47] that can arise from different steps in the food chain production. It is, therefore, unsurprising that some of the most nutritionally recommended foods pose significant challenges in terms of food preservation and safety. In recent years, foodborne outbreaks associated with the consumption of raw fruits and vegetables have been on the rise, prompting increased attention from researchers and health authorities to investigate food safety aspects related to microbial contamination of fresh produce [8][10][11][12][13][14][15][16][4,45,47,48,49,50,51,52].
2. Main Sources of Microbiological Contamination throughout the Food Chain Production
2.1. Soil
Pathogenic microorganisms of enteric origin can persist for extended periods in human and animal feces, posing a risk of contaminating land and crops [17][18][19][20][21][22][23][53,60,61,62,63,64,65]. Notably, Escherichia coli O157:H7 can endure for over seven months in soils exposed to rainy winter conditions. Furthermore, the widespread use of inadequately composted manure or feces from domestic or wild animals to fertilize and enhance soil structure has contributed to the spread of these microorganisms in the environment [21][24][25][57,63,66]. Crops, especially those growing closer to the ground, such as lettuce, are particularly vulnerable, as they may encounter soil during cultivation, irrigation, or heavy rains [23][26][27][65,67,68]. To mitigate the risk of introducing pathogens through organic fertilizer, it is recommended to allow a minimum of 90–120 days to pass (depending on whether the edible portions are in contact with the soil or not) between manure application and plant harvesting. The risk of pathogen presence decreases as the time between manure application and produce harvest increases [25][27][28][66,68,69].
2.2. Irrigation Water
Another significant contamination source is the use of contaminated water for irrigation or the application of pesticides. Foodborne outbreak investigations by the Centers for Disease Control and Prevention (CDC) have linked irrigation water to pathogen contamination of produce [29][30][31][70,71,72]. Studies by Dobhal et al. [32][73] have shown that strains of Salmonella Typhimurium and E. coli O157:H7 can survive in pesticide solutions. This situation is more prevalent in regions with water scarcity or where effluents are utilized for irrigation.
As natural reservoirs of E. coli and Salmonella include cattle, goats, and sheep, the intensification of animal production contributes to increased environmental and water contamination through runoff from production areas. The unrestricted access of farm or wild animals to cultivated fields or irrigation water is another important factor, as they can carry strains of Shiga toxin-producing E. coli (STEC) and other pathogenic microorganisms [9][25][26][33][46,66,67,74]. Several foodborne outbreaks resulting from produce contamination through irrigation water have been reported. For instance, in Sweden in 2015, an E. coli O157 outbreak was linked to contaminated water from a river used for irrigation of lettuce. Similarly, in the United States in 2008, a large outbreak caused by the consumption of serrano and jalapeño peppers was associated with contaminated irrigation water. Another incident occurred in 2010 when alfalfa sprouts were contaminated by Salmonella, and water runoff revealed the presence of the outbreak strain. In 2015, a multistate outbreak occurred due to the consumption of tomatoes irrigated with contaminated water [34][75]. Machado-Moreira et al. [15][51] reported E. coli and L. innocua contamination in lettuce due to spray irrigation with contaminated water, while Coleman et al. [35][76] demonstrated the contamination of hydroponic tomato plants grown with nutrient solution contaminated with Salmonella enterica.
The situation is particularly concerning due to variations in water regimes observed in recent years, including seasonal floods leading to fecal contamination and subsequent crop contamination. Conversely, dry summers have resulted in an increased reliance on wastewater, derived from effluent treatment on farms, to irrigate vegetable crops. As E. coli and Salmonella spp. can survive well in sediments, seasonal flooding during rainy seasons further contributes to increased contamination [36][37][77,78]. The use of untreated human sewage can also be a source of various pathogens, including Shigella spp., Salmonella enterica, different E. coli pathotypes, and enteric viruses [29][37][38][70,78,79]. Additionally, natural disasters such as fires and seasonal floods can lead to fecal contamination and subsequent produce contamination [39][24].
2.3. Insects
Insects are also a source of contamination for crops [9][17][46,53]. Flies are attracted to manure and can carry and transmit pathogenic microorganisms [40][80]. Experiments with the fruit fly (Ceratitis capitata) contaminated with E. coli strain labeled with a fluorescent protein have demonstrated that this insect can transmit pathogenic bacteria to intact fruits [41][81]. In addition to transmitting pathogenic microorganisms, insects can damage plant tissues by destroying the waxy cuticle, which is the first defense barrier, making them more vulnerable to pathogen penetration [40][80].
2.4. Human Manipulation
During harvesting, the contamination of products is exacerbated by poor hygiene practices among rural workers and the lack of sanitation facilities [3][22][24][27][37][40,57,64,68,78]. In the post-harvest phase, various factors can contribute to contamination. These include the use of contaminated ice or water, inadequate hygiene practices by handling staff or consumers, damage to plant tissues, issues with transport equipment, the presence of animals or pests in the environment, water quality during production and processing, use of contaminated equipment, cross-contamination, and improper storage conditions [9][22][42][43][46,64,82,83].
Concerning ready-to-eat vegetables, the primary source of contamination during the processing of lettuce and other minimally processed (MP) vegetables is the cutting stage. This operation has drawbacks, as it is during this stage that vegetables are most susceptible to mechanical damage. Moreover, an increase in the specific surface area makes tissues less effective barriers to the penetration of microorganisms. This results in a loss of cellular integrity, leading to physiological changes when the substrates encounter endogenous enzymes, rapid enzymatic catalysis reactions, and the growth of harmful bacteria [3][11][22][44][45][46][47][4,7,40,64,84,85,86].
3. Main Types of Contamination
3.1. Microbial Quality Indicators
Being simple tests to perform, the detection and counting of aerobic mesophilic or psychotropic microorganisms and of Enterobacteriaceae and coliforms have been the most widely used by the minimally processed fruits and vegetables (MPFV) industry as hygiene and quality indicators. This is done to compare the mesophilic or psychotropic microorganisms’ counts in MPFV at the time they are processed with those that are present in the natural product [37][44][7,78]. MPFV are referred to as more susceptible to microbial multiplication than unprocessed products due to the presence of cutting surfaces, increased nutrients available, plant tissue respiration, and confinement within the package. Additionally, there are no treatments to ensure microbiological stability [48][49][88,89]. Several studies report that the mesophilic or psychotropic levels present in lettuce or packaged salads vary widely between 3.0 and 9.40 log cfu.g−1.
Most of the bacteria identified in raw vegetables belong to the group of rod-shaped Gram-negative bacteria (80 to 90%) and include Pseudomonas spp., Flavobacterium spp., Enterobacter spp., Alcaligenes spp., Xantomonas spp., Klebsiella spp., Serratia spp., and Chromobacterium spp. The family Enterobacteriaceae, which includes the coliform group, constitutes about 10% of the microorganisms found in the total enumerations [49][50][89,98]. Poubol and Izumi [51][99], in mango cubes preserved in a CO2 atmosphere, reported that the predominant microbiota was Gram-negative rod-shaped bacteria, of which 60% were Enterobacteriaceae. Thus, high levels of these microorganisms are habitual in minimally processed fruits and vegetables (MPFV) and are not indicative of fecal contamination; however, they may compromise their sensorial and nutritional quality [52][100].
3.2. Pathogenic Microorganisms and Foodborne Disease-Related Cases
As previously mentioned, in addition to plant deteriorating microorganisms, it is crucial to consider pathogenic microorganisms transmitted by the produce as well. Over the last thirty years, the epidemiology of infectious diseases originating from food has undergone a significant shift, with plant products emerging as new vehicles for the transmission of zoonotic agents [15][29][53][54][51,70,106,107]. The scientific literature documents numerous outbreaks of this nature, some resulting in the tragic loss of hundreds of lives [12][17][29][44][49][54][55][7,48,53,70,89,107,108]. Salmonella spp., E. coli O157:H7, and L. monocytogenes are identified as the primary pathogenic microorganisms causing the most concern in such outbreaks [12][29][54][56][48,70,107,109]. A study conducted in Norway did not detect Salmonella spp. in any of the 118 samples [57][105].
Regarding outbreaks in 2021, vegetables, fruit juices, and related food products were responsible for 9.6% (n = 34) of confirmed outbreaks with strong evidence, while fruits, berries, and juices and their products accounted for 0.60% (n = 2) of such outbreaks, representing a significant increase, more than twice compared to 2020. It is noteworthy that a diverse range of causative agents were involved, including several Salmonella serovars implicated in 11 outbreaks, Shiga toxin-producing E. coli (STEC), Enteroinvasive E. coli (EIEC), Enterotoxigenic E. coli (ETEC), Yersinia enterocolitica, bacterial toxins such as Staphylococcus aureus, Clostridium botulinum, Bacillus cereus, unspecified bacterial toxins, viruses including Norovirus, and Cryptosporidium parvum. A total of 1715 individuals fell ill, with 131 hospitalizations, although there were no reported deaths. In addition to the three mentioned pathogens, other less frequent agents were also observed, impacting the safety of plant products and consequently the health of consumers. It is important to note that the average size of outbreaks attributed to this type of food (50 cases/outbreak) was significantly higher than those occurring due to the consumption of animal-origin foods (11 cases/outbreak) [58][23]. Among these occurrences, a notable outbreak was linked to Galia from Honduras. The implicated pathogen was Salmonella Braenderup sequence type 22, responsible for 348 illnesses and 68 hospitalizations between March and July 2021 in 12 European countries, including the United Kingdom.
It is worth mentioning that since 2012, Hepatitis A virus (HAV) outbreaks have been a recurrent problem in Europe, associated with frozen berries’ consumption. In June 2018, in Sweden, an HAV outbreak occurred linked to frozen strawberries imported from Poland. In October of the same year, in Austria, an HAV outbreak with a strain with the same genotype as the Sweden strain was also reported. The study has also concluded that the strawberries were acquired from the same producer from Poland [59][110]. Later, in Germany, from October 2018 until January 2020, the same HAV strain was responsible for 65 cases of the illness in 2 peaks (August to December 2018 and June to September 2019). The epidemiological research allowed peopleus to conclude that frozen strawberry cakes were the implicated food vehicle in both outbreak waves. The traceback investigations and phylogenetic analyses have demonstrated the strain (the same identified in Sweden and Austria outbreaks and the Polish producer) was also found in berries, sewage, and stools in Egypt, raising the hypothesis that the contamination occurred in this country. As the producer from Poland has received strawberries from Egypt through a German distributor, a unique contaminated batch may have caused all referred outbreaks [60][111].
Another major outbreak occurred between May and July 2011, marking a significant historical reference due to an unusually high number of cases and the challenges in finding the source of infection. This outbreak took place in Germany, resulting in 3816 cases, of which 845 developed hemolytic uremic syndrome (HUS) and 54 fatalities were reported. Notably, a majority (88%) of HUS cases were observed in adults, contrasting with typical infections by VTEC strains that usually affect children. Moreover, females, particularly those aged between 30 and 34 years, were the most affected, constituting 68% of HUS cases and 58% of gastroenteritis cases. The epidemic strain was identified as E. coli O104:H4 enteroaggregative, which had acquired the stx2a conversion bacteriophage. This outbreak gained international attention, with cases reported in 15 other countries in Europe and the USA. In France, eight cases were reported in individuals who attended a community event, and the isolated strain in these patients was genetically compatible with the epidemic strain from Germany. The investigations traced the outbreak back to the consumption of fenugreek sprouts, with the seeds of the implicated batch imported from Egypt in 2009 [61][62][63][112,113,114].
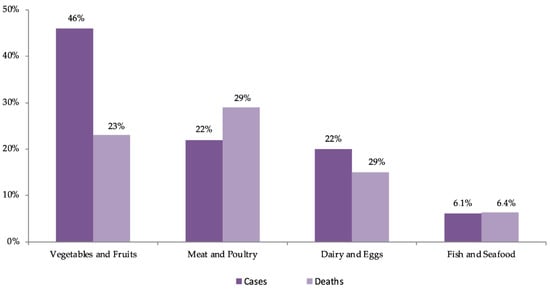
As illustrated in Figure 1, data from the USA estimate that between 1998 and 2008, fruits and vegetables were responsible for 46% of outbreaks, mostly caused by norovirus, Salmonella spp., and E. coli O157:H7, with leafy vegetables being the most frequent vehicle. Leafy vegetables were responsible for 2.2 million cases per year, representing 22% of all cases and constituting the food product responsible for the largest number of patients. Approximately 24,000 people (41%) are hospitalized each year due to the consumption of plant-origin products, with 38% attributed to fruits and vegetables and 16% to leafy vegetables, making dairy products the leading cause of hospitalizations. In terms of the number of deaths, fruits and vegetables account for 333 cases per year (23%), considerably lower than the 43% attributed to the consumption of animal products (terrestrial). In summary, leafy vegetables account for the largest number of patients (22%), making them the second most frequent cause of hospitalizations (14%) and the fifth cause of death (6%) [12][48].
However, in the USA, between September 2013 and May 2016, an outbreak caused by L. monocytogenes, associated with frozen vegetables consumption, occurred, which affected only nine persons (all were hospitalized), and three of them have died, which corresponds to 33.3%, and this percentage is superior to that reported in the literature [65][116]. The outbreaks occurred, particularly, in 2011 caused by E. coli O104:H4 in vegetable sprouts, in 2006 by contamination of spinach MP with E. coli O157:H7, in 1996 also with E. coli O157:H7 in lettuce, and Salmonella spp. in tomato, juice, fruits, and sprouts reinforce the concern with products that are consumed raw and calls attention to the need to increase preventive strategies [55][63][66][67][108,114,117,118].
A study conducted by the Interagency Food Safety Analytics Collaboration, utilizing data from 1998 through 2020, estimated the percentage of illnesses caused by three priority pathogens—Salmonella spp., E. coli O157, and L. monocytogenes—in the year 2020. Unfortunately, no results were provided for the fourth priority pathogen, Campylobacter. The study, based on 1287 outbreaks, indicated that 960 were caused by or suspected to be caused by Salmonella spp., 272 by E. coli O157, and 55 by L. monocytogenes.
Yet another pathogenic microorganism that has raised some questions about its possible transmission through the consumption of produce is Clostridioides difficile (previously known as Clostridium difficile) [68][121]. This is an anaerobic spore-forming pathogenic bacteria that acts negatively in the gastrointestinal tract, causing a serious illness, particularly in hospitalized persons, subject to prolonged treatment with antibiotics. However, in the last two decades the incidence of C. difficile infection (CDI) has increased in the community, oftentimes in people with no history of hospitalization or antibiotic treatment [69][70][71][72][122,123,124,125]. The rapid expansion of community-acquired CDI raised the hypothesis that C. difficile present in the environment, animals, and retail foods causes this infection in humans [70][72][73][74][123,125,126,127]. In addition, several studies demonstrate the presence of C. difficile in several foods, including meat, ready-to-eat salads, and raw vegetables (such as cucumber, onions, carrots, etc.) [75][76][77][78][128,129,130,131]. Given that C. difficile is present in water, animal feces, and livestock manure compost, it could easily be transferred to vegetables.
4. Major Decontamination Methodologies: Related Problems and Possible Solutions
It is crucial to emphasize that MPFV do not undergo any stage ensuring the elimination of the risk related to their consumption, as they lack heat treatment to eliminate pathogens, spores, and toxins at safety levels. Therefore, the vegetable sanitation/disinfection stage, especially in MPFV, becomes critical for food safety. MPFV plants are cut, and the damage to cells makes them more susceptible to microbiological multiplication and biochemical alterations, intensifying respiratory rates and enzymatic activity [1][6][9][49][79][80][81][82][26,43,46,89,134,135,136,137].
While washing and disinfection steps of plant products are moderately effective, they are by no means efficient when dealing with internalized pathogenic microorganisms. Pathogens can penetrate plant tissues either in the pre-harvest phase through internalization or in the post-harvest phase through infiltration, complicating the situation. Infiltration, or the suction effect, can occur when a product at room temperature is submerged in colder water, creating a vacuum that sucks water and, if present, pathogenic microorganisms into the tissues through pores, channels, or fissures [33][82][83][84][85][86][87][15,74,137,138,139,140,141]. Studies have shown that tomatoes submerged in an E. coli O157:H7 suspension exhibited contamination, and Salmonella Typhimurium was found to infiltrate baby spinach during washing operations, dependent on humidity, temperature, and illumination conditions [88][89][142,143]. Internalization may also occur during flowering, with pathogenic microorganisms entering through flowers carried by water or insects, through roots from contaminated soil or water, through wounds or cracks, or by entrapment in the waxy film [90][144]. Laboratory studies have demonstrated the entry of pathogens into plant tissues through natural openings such as stomata, root, and flower junctions, or through tissue damage. After binding to plant tissues, microorganisms have the capability to form biofilms, thereby improving their capacity to endure within the plant structure [33][91][92][74,145,146]. In essence, the internalization of pathogenic microorganisms can take place at any point in the plant’s life cycle, progressing to subsequent phases such as seed, germination, mature plant, flower, and fruit [16][52].
4.1. Chlorine Disinfection
Currently, the predominant disinfection methods involve the application of chlorine-based disinfectants [6][11][4,43]. However, these disinfectants pose risks to human health by generating carcinogenic compounds [44][7] and are not highly effective, as their disinfecting impact diminishes rapidly, allowing surviving bacterial populations to multiply more rapidly than those in non-disinfected products [6][9][43,46]. Chlorinated water is commonly utilized for disinfecting MPFV due to its cost-effectiveness and ease of use [6][43]. The efficacy of decontamination is assessed not only by the reduction achieved but, more crucially, by the ability to sustain this reduction over the product’s shelf life. Nevertheless, the use of active chlorine raises health concerns due to the formation of toxic by-products such as trihalomethanes and chloramines. This concern has led to restrictions on chlorine’s usage in several European countries, including the Netherlands, Sweden, Germany, Switzerland, Denmark, and Belgium [44][49][7,89]. A study by Coroneo et al. [93][147] investigated the presence of these derivatives during the disinfection process, concluding that toxic or carcinogenic compounds, specifically trihalomethanes, are formed and persist in the final product.
4.2. Other Chemical Methods of Disinfection
Recent advancements have introduced various methodologies relying on chemical disinfectants, including chlorine dioxide [7][11][44][4,7,44], organic acids [6][11][44][4,7,43], hydrogen peroxide [3][7][44][7,40,44], electrolyzed water [6][7][11][44][4,7,43,44], ozonated water [6][7][11][44][4,7,43,44], and calcium-based solutions [44][94][7,148]. These methods have demonstrated ease of application and a potent bactericidal effect. However, most of them come with certain drawbacks. For instance, the use of chlorine dioxide, while effective in reducing bacterial populations, has been found to impact some organoleptic characteristics. Another consideration is the significant reduction of the native microbial population, which, by decreasing competition for space and nutrients, may potentially result in a subsequent increase in the development of pathogenic microorganisms [49][89].
2.4.3. Physical Methods of Disinfection
Recent developments have introduced physical treatments such as ionizing radiation [3][11][44][4,7,40], ultraviolet [6][11][44][95][4,7,43,149], infrared [11][44][96][4,7,150], modified atmosphere packaging [3][44][7,40], or combinations such as ultrasound with ε-polylysine [97][151], aimed at preserving these types of products. Modified atmosphere packaging is a technique currently employed in the industry. These methods may be either bacteriostatic or bactericidal, demonstrating high efficiency in inhibiting microbial contaminations [46][85]. However, they come with certain challenges; for example, irradiation cannot be used as an isolated step of continuous washing, as it alone does not remove chemical residues or soil [7][44][7,44].
5. Possible Future Solutions: The Use of Natural Disinfectants and Smart Packaging as an Alternative for Decontamination of Minimally Processed Fruits and Vegetables
As consumer preferences shift towards natural and minimally processed products with fewer chemical additives and extended shelf life, the use of synthetic antimicrobials is becoming more restricted due to potential toxicity concerns. Consequently, there is a growing need to identify alternative antibacterial substances, preferably of biological origin, that are both effective and harmless to human health and the environment. Natural antibacterial compounds have emerged as a promising alternative, gaining increased interest in their potential to eliminate pathogenic microorganisms, especially considering their resistance to antibiotics [98][99][100][101][102][152,153,154,155,156].
Numerous studies have explored new disinfection methods with the dual purpose of eliminating pathogens and preventing the degradation of vegetable products [7][101][103][44,155,157]. It is crucial to investigate techniques that not only decontaminate the product but also maintain low levels of microbiota over its shelf life. These compounds are derived from various sources, including plants (essential oils), microorganisms (such as lactic acid bacteria producing both lactic acid and antimicrobial polypeptides), and animals (for example, lysozyme) [99][103][104][153,157,158]. Antibacterial bioactive compounds are biological substances produced as defense against other organisms, and since these natural products and their components are generally recognized as safe (GRAS), concerns about their safety in preventing the development of pathogenic microorganisms or product alteration are minimal.
In recent decades, alternative compounds with the potential for food disinfection have emerged, including acetic acid, ascorbic acid, lactic acid, essential oils, and cheese whey, among others [98][104][152,158], all of which have less reported secondary effects and are more biodegradable. Smart packaging, an emerging technology in the food packaging industry, integrates active and intelligent features to enhance food safety and quality [105][106][159,160]. Over the past decades, innovative applications have surfaced, including the use of bioactive compounds such as essential oils (EO) in various packaging forms such as coating, nanoencapsulation, and synergistic pairings with other antibacterial agents [91][145]. Additionally, using materials with smart packaging properties, such as being impermeable to oxygen, light, moisture, and certain gases, contributes to minimizing spoilage by reducing microbial activity, with nanocomposite materials providing added resistance [105][106][159,160].
To optimize smart packaging development, it is crucial to consider cultural, social, and cognitive factors influencing consumer acceptance [107][161]. Tailoring these technologies to meet consumer preferences and needs, along with effective communication addressing consumer concerns and educating them on the benefits, will be key for successful implementation. However, despite these advancements, there are still limited natural disinfectants proposed in scientific studies that have reached the market. Traditional chemical methods, such as chlorinated compounds, continue to be used, emphasizing the importance of developing natural disinfectant products that can effectively replace chlorine-based products without compromising safety, environmental impact, or the organoleptic characteristics of the product.
