Appropriate surgical antimicrobial prophylaxis (SAP) is an important measure in preventing surgical site infections (SSIs). Although antimicrobial pharmacokinetics–pharmacodynamics (PKPD) is integral to optimizing antibiotic dosing for the treatment of infections, there is less research on preventing infections postsurgery. Whereas clinical studies of SAP dose, preincision timing, and redosing are informative, it is difficult to isolate their effect on SSI outcomes. Antimicrobial PKPD aims to explain the complex relationship between antibiotic exposure during surgery and the subsequent development of SSI. It accounts for the many factors that influence the PKs and antibiotic concentrations in patients and considers the susceptibilities of bacteria most likely to contaminate the surgical site.
- antibiotic prophylaxis
- surgical prophylaxis
- cefazolin
- pharmacokinetics
- pharmacodynamics
1. Introduction
2. Dose–Response Relationship in Cefazolin Prophylaxis
Although clinical studies relating the SAP dose to SSI are informative, there are significant limitations that can impede the detection of a dose–SSI relationship. First, without the PKs, dose is a poor predictor of the antibiotic concentrations achieved in patients and antimicrobial activity in vivo. Furthermore, dose is only one component of the SAP regimen which also relies on appropriate preincision timing and redosing during surgery. Finally, SSI outcomes are affected by many other patient- and surgery-related factors such as obesity, diabetes, immune status, type of surgery, wound classification, and surgical duration. Heavier body weight (i.e., obesity) is a significant risk factor [23,24][23][24] which often complicates the study of cefazolin dosing for surgical prophylaxis. With the use of standard doses, there is a negative correlation between body weight and the mg/kg dose received by patients. For example, the mg/kg dose delivered by 2 g of cefazolin decreases as body weight increases to the cut-off of 120 kg, thereby confounding the effects of heavier body weight and lower dose as risk factors for SSI.
Abdel Jalil et al. conducted a prospective, observational study of the frequency and potential risk factors for SSI in caesarean surgery [26][25]. Compliance with a new institutional guideline to use 2 g instead of 1 g of cefazolin preoperatively for patients <120 kg was also evaluated. A dose–response relationship was observed where patients who developed SSI received a lower calculated mg/kg dose than those without infection (18.7 mg/kg versus 22.2 mg/kg, p = 0.037). Furthermore, a lower mg/kg dose of cefazolin independently associated with SSI (p = 0.035) in multivariable logistic regression analysis, as were longer hospital stay (p = 0.001), higher BMI (p = 0.003), and delivery beyond the 40th week (p = 0.005). As expected, the mg/kg dose was negatively correlated with BMI. The investigators concluded that using 2 g versus 1 g of cefazolin was beneficial, predicting that it would reduce the risk of infection by 36% in their typical patient undergoing caesarean surgery.
Morris et al. analyzed the relationship between cefazolin dose, body weight, and SSI in 38,288 cases of hip or knee arthroplasty, using data from a national (New Zealand) prospective, surveillance and quality improvement programme [28][26]. Underdosing was defined as 1 g for individuals ≥80 kg or <3 g for those ≥120 kg. The preoperative dose was administered within 1 h in 96% of cases, and surgery exceeded 4 h in only 1% of cases. The recommended cefazolin dose was given in 94.5% cases, noting that only 27% of patients ≥120 kg received 3 g. After multivariable analysis, underdosing (OR = 2.19, p < 0.0001), higher surgical risk score (p < 0.0001), revision (p < 0.0001) or hip surgery (p = 0.028), and male gender (p = 0.026) were independently associated with SSI. It was estimated that 83 heavier-weight individuals needed to be treated with the recommended dose to prevent one infection. The investigators suggested that 2 g and at least 3 g of cefazolin were appropriate for patients ≥80 kg and ≥120 kg, respectively, but were unable to address the potential need for higher doses in patients with morbid obesity undergoing arthroplasty.
In summary, available evidence supports an association between lower antibiotic concentrations in patients undergoing surgery, particularly at wound closure, and an increased risk of infection. However, the number of studies is relatively small. More research is needed to fully understand the principles of antimicrobial PKPD in surgical prophylaxis and realize its potential to improve SSI outcomes. Further study of antibiotic concentrations in serum/plasma and interstitial fluid during surgery can also help identify clinically meaningful targets for effective SAP.
3. Antibiotic Concentration–Response (SSI) Relationship in SAP
In 1977, Goldmann et al. may have been the first to note an association between SSI and antibiotic concentrations in patients undergoing surgery [30][27]. They conducted a prospective, double-blinded trial of extended courses of cephalothin prophylaxis following prosthetic valve replacement. Although there was no benefit to prolonging the course of antibiotics, the investigators observed that patients without detectable cephalothin in their serum at the close of surgery were more likely to develop staphylococcal SSI [27.3% (3/11) versus 1.1% (2/175), p = 0.002]. The PKPD of gentamicin prophylaxis in colorectal surgery was studied as part of a prospective, double-blinded trial that compared a single-dose versus multiple-dose regimen of gentamicin and metronidazole (n = 134) [31,32][28][29]. In the PKPD analysis, several patient- and surgery-related variables were investigated as potential risk factors for SSI. Gentamicin preincision timing, serum concentrations at incision and closure, and AUC from incision to closure were also considered. After multivariable analysis, a lower gentamicin concentration at closure (p = 0.02), diabetes (p = 0.02), stoma (p = 0.04), and older age (p = 0.05) were independently associated with infection. The PKPD of cefazolin prophylaxis was investigated as part of a prospective, non-interventional PK study of total and unbound cefazolin in patients undergoing cardiac surgery (n = 40) [33,34][30][31]. After multivariable analysis, a lower total plasma concentration at closure (OR = 1.3 per 10% decrease in concentration, p = 0.038) and longer surgery (OR = 2.9 per additional 1 h, p = 0.027,) were independently associated with SSI. In classification and regression tree (CART) analysis, a total cefazolin closure concentration <104 mg/L (~29 mg/L unbound) and surgery >346 min were significant thresholds for infection. Given the small sample size, the thresholds were more descriptive of the PKPD relationship than definitive targets. The stronger association with total as opposed to unbound cefazolin may have been due to significant variability in plasma albumin and protein binding during cardiac surgery. Takayama et al. examined cefmetazole in serum and whole (fat) tissue during lower gastrointestinal surgery (n = 105) [36][32]. Subcutaneous tissue samples were collected at the time of incision and before skin closure. The tissue was pulverized in liquid nitrogen, homogenized in a phosphate buffer, and centrifuged to obtain supernatant for the analytical assay. In univariate analysis, a lower tissue concentration at closure (1.0 mg/g versus 2.2 mg/g, p = 0.09), not redosing during surgery (p = 0.09), lower creatinine clearance (p = 0.09), and older age (p = 0.02) were associated with SSI (α = 0.1). Although the amount of antibiotic in surgical tissue is important, the methodology and interpretation of such data must be carefully considered [37,38][33][34]. Antibiotic tissue concentrations in the extracellular space, where bacteria contaminate the wound, are most relevant. Since only free antibiotic diffuses between the plasma and interstitial fluid, unbound plasma concentrations are more indicative of the pharmacologically active antibiotic in extracellular tissue. Microdialysis studies can be used to measure antibiotic in interstitial fluid that is collected from semipermeable catheters inserted or surgically placed in the tissue of interest. The probes are flushed with perfusion fluid, thereby allowing interstitial fluid to be continuously sampled during surgery. In contrast, whole tissue studies collect samples at specific times and measure the overall average amount of antibiotic per volume/weight of tissue. Since the methods lack standardization and procedures for quality control, the results are difficult to interpret [37,38][33][34]. Most techniques involve homogenizing whole tissue into a suspension of its cellular, extracellular, and vascular components, and then processing the sample to obtain supernatant. Noting that interstitial fluid accounts for only 10% to 30% of tissue volume, whole tissue concentrations do not reflect the antibiotic’s distribution or pharmacological activity in vivo. Since β-lactams like cefmetazole distribute into interstitial fluid, the concentrations in pulverized adipose tissue are diluted, thereby underestimating those in extracellular tissue [39][35]. Despite the limitations, however, the findings of Takamaya et al. support an antibiotic concentration–response relationship for cefmetazole prophylaxis [36][32]. The tissue concentrations at closure, using consistent sampling and analytical methods, were significantly lower in patients who developed SSI. Although it signals the importance of maintaining antibiotic in tissue during surgery, the specific concentrations are not clinically applicable and can not be compared to MICs or otherwise used to predict antibacterial activity at the surgical site. In summary, available evidence supports an association between lower antibiotic concentrations in patients undergoing surgery, particularly at wound closure, and an increased risk of infection. However, the number of studies is relatively small. More research is needed to fully understand the principles of antimicrobial PKPD in surgical prophylaxis and realize its potential to improve SSI outcomes. Further study of antibiotic concentrations in serum/plasma and interstitial fluid during surgery can also help identify clinically meaningful targets for effective SAP.4. Relevance and Role of PKPD in SAP
4.1. Antimicrobial PKPD and Monte Carlo Simulations
Monte Carlo simulation studies are important in antimicrobial PKPD research and knowledge translation [12,48][12][36]. They can integrate the complexity of numerous and often interdependent variables related to the patient, antibiotic, and infection. And they can incorporate real-world variability into patient characteristics (e.g., age, body weight, renal function) and PK parameters (e.g., Vd, t½, protein binding). Instead of interpolating based on an average or typical case, simulations can predict the probability of outcomes for an infinite number of “what-if-scenarios”. Monte Carlo simulations are increasingly used to evaluate and compare SAP regimens. First, the surgical population is generated according to the desired patient characteristics. The SAP is replicated in each subject, and antibiotic concentration curves are generated based on PK models. The use of relevant, high-quality PK data is essential to produce reliable and translatable simulation results. Ideally, population PK models that describe covariate relationships between parameters, such as body weight and Vd, or renal function and t½, are used [49][37]. Unbound concentrations may be simulated using the percentage of protein binding or population PK data for unbound drug if available. The concentration curves of each subject are considered against the most likely SSI pathogens, and the probability of achieving the desired PKPD target is predicted for the population. Since the goal of SAP is to maintain adequate antibiotic concentrations throughout surgery, the relevant PKPD target is to achieve 100%ƒT>MIC, from incision to closure. Unlike the treatment of infections, however, the MIC is speculative, and the concentration threshold used to evaluate SAP is selected by the investigator. As such, Monte Carlo simulations are typically designed to determine the probability of target attainment (PTA) for 100%ƒT>MIC using a specific MIC believed to be the lowest acceptable concentration for surgical prophylaxis or the fractional target attainment (FTA) using the distribution of MICs for a population of bacteria. In all cases, simulation studies must be considered carefully with regards to their methods, input data, analysis, and interpretation of results.4.2. PKPD Considerations for Improving Cefazolin Prophylaxis
4.2.1. Pharmacokinetics of Cefazolin Prophylaxis
Cefazolin is a small hydrophilic compound with PKs characterized by an average protein binding of 80%, apparent Vd of 0.15 L/kg, and terminal t½ with normal renal function of 2 h [51][38]. The PKs of cefazolin are variable in patients depending on factors such as age, sex, body weight and composition, renal function, and comorbidities. The concentration curve for a bolus dose of cefazolin can be described by a two-compartment model, where the central compartment represents intravascular space (i.e., serum/plasma), and the peripheral compartment signifies extracellular tissue (i.e., interstitial fluid). The Cmax in plasma is determined by the dose, infusion, and central Vd. The transiently high plasma concentrations following a bolus dose are less clinically relevant since free cefazolin rapidly diffuses across the concentration gradient into tissue. The post-distributional concentrations decline during the elimination phase primarily due to renal clearance. The tissue penetration of antibiotics is an important consideration in the treatment and prevention of infections [38][34]. The diffusion of an antibiotic into tissue depends on its physiochemical properties, favoring those with smaller size, higher lipophilicity, and lower protein binding. The tissue characteristics are also relevant where well vascularized sites without additional barriers are more accessible.4.2.2. Cefazolin Prophylaxis Dose and Obesity
Although there is broad support for the 2 g dose of cefazolin for patients <120 kg [27[39][40],29], the 3 g dose for those ≥120 kg is controversial. In 2022, Coates et al. published a systematic review of cefazolin prophylaxis and dosing in patients with obesity [59][41]. Three SSI outcome studies were identified including one in caesarean surgery where patients ≥131.5 kg received either 2 g or 3 g of cefazolin preoperatively [60][42]. Two studies were conducted in elective surgery where one compared 2 g to 3 g in patients ≥100 kg [61][43], and the other examined 2 g in those <120 kg and ≥120 kg [62][44]. None of the outcome studies supported the higher dose of cefazolin for patients with obesity. Fifteen PK studies that evaluated serum/plasma or tissue concentrations against an MIC-based target of 100%ƒT>MIC were also summarevieweized. Nine studies concluded that 2 g of cefazolin was sufficient for patients with obesity, whereas six found that it was insufficient. As noted in the review, the The PK studies were difficult to interpret given the variability in patients, surgeries, sampling sites, and PK modelling and simulation methods. Most notably, the MIC threshold used to determine %ƒT>MIC and evaluate cefazolin doses ranged from 1 mg/L to 8 mg, limiting the ability to compare study results. Without evidence to the contrary, Coates et al. proposed that 2 g of cefazolin was sufficient for patients with obesity undergoing surgery lasting up to 4 h. PK studies can show relatively small differences in cefazolin concentrations with the same dose for heavier body weights extending into obesity and morbid obesity. This is explained by the distribution of cefazolin, and most β-lactams, into extracellular tissue which lessens the effects of obesity on Vd. As shown in Figure 1, the differences with 2 g of cefazolin for body weights ranging from 60 kg to 180 kg are relatively modest and narrow over time. Most relevant to surgical prophylaxis, the cefazolin concentrations are similar at a redosing time of 3 h to 4 h. However, cefazolin concentrations in interstitial fluid, represented by unbound plasma concentrations as in Figure 1 or measured using microdialysis, must be considered in context. Given the excess adipose tissue, there is significantly less interstitial fluid in the tissue of patients with obesity. Since adipose tissue is also poorly vascularized, the amount of antibiotic available at the surgical site is further reduced. Therefore, a cefazolin dose (e.g., 2 g) that produces similar cefazolin concentrations in the interstitial fluid of nonobese and obese patients does not necessarily provide comparable surgical prophylaxis. Given the lower amounts of interstitial fluid and blood flow in adipose tissue, it is possible that higher interstitial fluid concentrations and PKPD targets would be beneficial in obesity. It is an important consideration that supports using a higher cefazolin dose for heavier body weights. Although strong evidence for the 3 g dose in patients ≥120 kg is lacking, as previously discussed, clinical studies of cefazolin dose and SSI have limitations that make it difficult to detect differences that may exist between doses. Furthermore, PK-simulation studies may not consider the potential need for higher concentrations in obesity. Although the weight-based cut-offs of 120 kg and 35 kg/m2 have been shown to poorly predict those who required more than 2 g of cefazolin [66][45], better approaches are not available at this time. Finally, whereas the additional risks of using a 3 g versus 2 g dose are minimal, the benefits include increasing cefazolin concentrations in interstitial fluid, extending the duration of prophylaxis coverage, and potentially preventing SSIs in a high-risk patient population.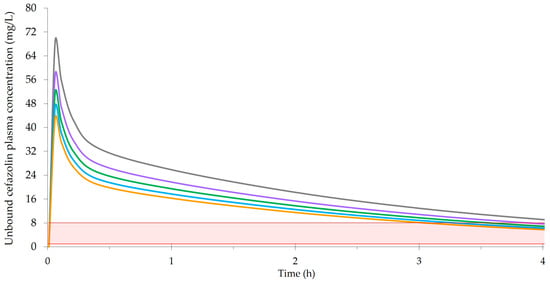
4.2.3. Preincision Timing of Cefazolin Prophylaxis
SAP must be administered prior to incision to be effective [67,68,69][46][47][48]. Although there is general agreement to give the first dose within 60 min of incision, a 120 min window may be acceptable when considering antibiotics with long t½’s or prolonged infusions, e.g., vancomycin [21]. There are also suggestions of added benefit for specific times within the 60 min window. While some studies reported lower infection rates when SAP was administered closer to incision [68[47][49][50][51],70,71,72], others found no difference [73,74,75][52][53][54] or a higher rate of SSI [76][55]. In 2017, de Jong et al. published a meta-analysis of different SAP timing intervals for 54,552 patients from 14 studies [69][48]. Although the risk of SSI was significantly higher when SAP was given more than 120 min before incision (OR = 5.26, CI95% 3.29–8.39) or after incision (OR = 1.89, CI95% 1.05–3.40), differences were not observed for specific times within the 120 min window. The authors also noted considerable heterogeneity in the antibiotics and dosing regimens, and the evidence overall was low to moderate. Figure 2 exemplifies the potential effects of preincision timing on a 2 g bolus dose of cefazolin for a body weight of 80 kg. It is based on the same population-PK model and data described for Figure 1 [63][56]. In addition to unbound plasma concentrations, Figure 2 displays cefazolin concentrations in interstitial fluid. The tissue concentrations increase more gradually as free cefazolin diffuses into the peripheral compartment. The rate of tissue penetration can also be characterized by the time to achieve maximum cefazolin concentrations (Tmax) following a preoperative dose. One study in abdominal aortic aneurysm repair surgery observed rapid diffusion into subcutaneous tissue (microdialysis) with a median Tmax of 2.0 min [54][57]. Separate investigations of cefazolin penetration into the skeletal muscle (microdialysis) of pediatric patients reported a median Tmax of 37.6 min in cardiac surgery, and values from 30 min to 38.5 min in spinal surgery [77,78][58][59]. The findings of such studies are variable and significantly influenced by the methods for sampling and data analysis. As depicted by the concentration curves in Figure 2, adjusting the preincision timing to ensure maximum tissue concentrations at the time of incision is unlikely to be beneficial or necessary.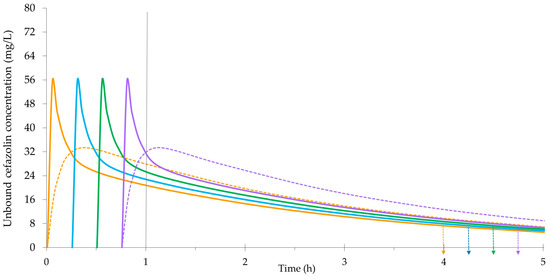
4.2.4. Redosing Cefazolin Prophylaxis during Surgery
Redosing during surgery may be required to ensure adequate cefazolin concentrations at closure [79][60]. In 2022, Wolfhagen et al. published a meta-analysis of SAP redosing for 9470 patients from 10 studies [80][61]. Redosing was associated with a significant reduction in SSI in the observational cohort studies only (OR = 0.55, CI95% 0.38–0.79). Again, there was notable heterogeneity in the antibiotics and redosing protocols, leading to an overall low certainty of the evidence. Based on the longstanding recommendation of redosing every 2 t½’s, cefazolin is typically given every 3 h or 4 h assuming normal renal function. As kidney function declines, the duration of cefazolin prophylaxis coverage is extended and redosing may not be required [81][62]. On the other hand, more aggressive redosing may be used in situations where standard SAP regimens are inadequate.4.2.5. Conclusions
Optimal antibiotic dosing is based on the principles of antimicrobial PKPD. For SAP, PKPD relates antibiotic exposure during surgery to the subsequent development of SSI. It can incorporate the complexity of numerous and often interdependent variables related to the patient, antibiotic regimen, concentrations achieved in patients, and susceptibilities of the most likely SSI pathogens. It also shows the inextricable connection between SAP dose, preincision timing, and redosing, and why it is so difficult to isolate their effect on SSI outcomes in clinical studies.References
- Badia, J.M.; Casey, A.L.; Petrosillo, N.; Hudson, P.M.; Mitchell, S.A.; Crosby, C. Impact of Surgical Site Infection on Healthcare Costs and Patient Outcomes: A Systematic Review in Six European Countries. J. Hosp. Infect. 2017, 96, 1–15.
- Eckmann, C.; Kramer, A.; Assadian, O.; Flessa, S.; Huebner, C.; Michnacs, K.; Muehlendyck, C.; Podolski, K.M.; Wilke, M.; Heinlein, W.; et al. Clinical and Economic Burden of Surgical Site Infections in Inpatient Care in Germany: A Retrospective, Cross-Sectional Analysis from 79 Hospitals. PLoS ONE 2022, 17, e0275970.
- Gillespie, B.M.; Harbeck, E.; Rattray, M.; Liang, R.; Walker, R.; Latimer, S.; Thalib, L.; Andersson, A.E.; Griffin, B.; Ware, R.; et al. Worldwide Incidence of Surgical Site Infections in General Surgical Patients: A Systematic Review and Meta-Analysis of 488,594 Patients. Int. J. Surg. 2021, 95, 106136.
- Umscheid, C.A.; Mitchell, M.D.; Doshi, J.A.; Agarwal, R.; Williams, K.; Brennan, P.J. Estimating the Proportion of Healthcare-Associated Infections That Are Reasonably Preventable and the Related Mortality and Costs. Infect. Control Hosp. Epidemiol. 2011, 32, 101–114.
- Schreiber, P.W.; Sax, H.; Wolfensberger, A.; Clack, L.; Kuster, S.P. The Preventable Proportion of Healthcare-Associated Infections 2005–2016: Systematic Review and Meta-Analysis. Infect. Control Hosp. Epidemiol. 2018, 39, 1277–1295.
- Bowater, R.J.; Stirling, S.A.; Lilford, R.J. Is Antibiotic Prophylaxis in Surgery a Generally Effective Intervention?: Testing a Generic Hypothesis Over a Set of Meta-Analyses. Ann. Surg. 2009, 249, 551–556.
- Menz, B.D.; Charani, E.; Gordon, D.L.; Leather, A.J.; Moonesinghe, S.R.; Phillips, C.J. Surgical Antibiotic Prophylaxis in an Era of Antibiotic Resistance: Common Resistant Bacteria and Wider Considerations for Practice. IDR 2021, 14, 5235–5252.
- Bratzler, D.W.; Dellinger, E.P.; Olsen, K.M.; Perl, T.M.; Auwaerter, P.G.; Bolon, M.K.; Fish, D.N.; Napolitano, L.M.; Sawyer, R.G.; Slain, D.; et al. Clinical Practice Guidelines for Antimicrobial Prophylaxis in Surgery. Am. J. Health-Syst. Pharm. 2013, 70, 195–283.
- Rodríguez-Gascón, A.; Solinís, M.Á.; Isla, A. The Role of PK/PD Analysis in the Development and Evaluation of Antimicrobials. Pharmaceutics 2021, 13, 833.
- Rao, G.G.; Landersdorfer, C.B. Antibiotic Pharmacokinetic/Pharmacodynamic Modelling: MIC, Pharmacodynamic Indices and Beyond. Int. J. Antimicrob. Agents 2021, 58, 106368.
- Velkov, T.; Bergen, P.J.; Lora-Tamayo, J.; Landersdorfer, C.B.; Li, J. PK/PD Models in Antibacterial Development. Curr. Opin. Microbiol. 2013, 16, 573–579.
- Rizk, M.L.; Bhavnani, S.M.; Drusano, G.; Dane, A.; Eakin, A.E.; Guina, T.; Jang, S.H.; Tomayko, J.F.; Wang, J.; Zhuang, L.; et al. Considerations for Dose Selection and Clinical Pharmacokinetics/Pharmacodynamics for the Development of Antibacterial Agents. Antimicrob. Agents Chemother. 2019, 63, e02309-18.
- Li, J.; Lovern, M.; Riccobene, T.; Carrothers, T.J.; Newell, P.; Das, S.; Talley, A.K.; Tawadrous, M. Considerations in the Selection of Renal Dosage Adjustments for Patients with Serious Infections and Lessons Learned from the Development of Ceftazidime-Avibactam. Antimicrob. Agents Chemother. 2020, 64, e02105-19.
- Sumi, C.D.; Heffernan, A.J.; Lipman, J.; Roberts, J.A.; Sime, F.B. What Antibiotic Exposures Are Required to Suppress the Emergence of Resistance for Gram-Negative Bacteria? A Systematic Review. Clin. Pharmacokinet. 2019, 58, 1407–1443.
- Crass, R.L.; Cojutti, P.G.; Pai, M.P.; Pea, F. Reappraisal of Linezolid Dosing in Renal Impairment To Improve Safety. Antimicrob. Agents Chemother. 2019, 63, e00605-19.
- Zelenitsky, S.A.; Ariano, R.E. An Updated Vancomycin Dosing Protocol for Initiating Therapy in Patients Undergoing Intermittent High-Flux Hemodialysis. Am. J. Health-Syst. Pharm. 2022, 79, 1006–1010.
- Parker, S.L.; Abdul-Aziz, M.H.; Roberts, J.A. The Role of Antibiotic Pharmacokinetic Studies Performed Post-Licensing. Int. J. Antimicrob. Agents 2020, 56, 106165.
- Mouton, J.W.; Brown, D.F.J.; Apfalter, P.; Cantón, R.; Giske, C.G.; Ivanova, M.; MacGowan, A.P.; Rodloff, A.; Soussy, C.-J.; Steinbakk, M.; et al. The Role of Pharmacokinetics/Pharmacodynamics in Setting Clinical MIC Breakpoints: The EUCAST Approach. Clin. Microbiol. Infect. 2012, 18, E37–E45.
- Ambrose, P.G.; Bhavnani, S.M.; Andes, D.R.; Bradley, J.S.; Flamm, R.K.; Pogue, J.M.; Jones, R.N. Old In Vitro Antimicrobial Breakpoints Are Misleading Stewardship Efforts, Delaying Adoption of Innovative Therapies, and Harming Patients. Open Forum Infect. Dis. 2020, 7, ofaa084.
- Berríos-Torres, S.I.; Umscheid, C.A.; Bratzler, D.W.; Leas, B.; Stone, E.C.; Kelz, R.R.; Reinke, C.E.; Morgan, S.; Solomkin, J.S.; Mazuski, J.E.; et al. Centers for Disease Control and Prevention Guideline for the Prevention of Surgical Site Infection, 2017. JAMA Surg. 2017, 152, 784–791.
- World Health Organization. Global Guidelines for the Prevention of Surgical Site Infection, 2nd ed.; World Health Organization: Geneva, Switzerland, 2018; ISBN 978-92-4-155047-5.
- Calderwood, M.S.; Anderson, D.J.; Bratzler, D.W.; Dellinger, E.P.; Garcia-Houchins, S.; Maragakis, L.L.; Nyquist, A.-C.; Perkins, K.M.; Preas, M.A.; Saiman, L.; et al. Strategies to Prevent Surgical Site Infections in Acute-Care Hospitals: 2022 Update. Infect. Control Hosp. Epidemiol. 2023, 44, 695–720.
- Winfield, R.D.; Reese, S.; Bochicchio, K.; Mazuski, J.E.; Bochicchio, G.V. Obesity and the Risk for Surgical Site Infection in Abdominal Surgery. Am. Surg. 2016, 82, 331–336.
- Thelwall, S.; Harrington, P.; Sheridan, E.; Lamagni, T. Impact of Obesity on the Risk of Wound Infection Following Surgery: Results from a Nationwide Prospective Multicentre Cohort Study in England. Clin. Microbiol. Infect. 2015, 21, 1008.e1–1008.e8.
- Abdel Jalil, M.H.; Abu Hammour, K.; Alsous, M.; Awad, W.; Hadadden, R.; Bakri, F.; Fram, K. Surgical Site Infections Following Caesarean Operations at a Jordanian Teaching Hospital: Frequency and Implicated Factors. Sci. Rep. 2017, 7, 12210.
- Morris, A.J.; Roberts, S.A.; Grae, N.; Frampton, C.M. Surgical Site Infection Rate Is Higher Following Hip and Knee Arthroplasty When Cefazolin Is Underdosed. Am. J. Health-Syst. Pharm. 2020, 77, 434–440.
- Goldmann, D.A.; Hopkins, C.C.; Karchmer, A.W.; Abel, R.M.; McEnany, M.T.; Akins, C.; Buckley, M.J.; Moellering, R.C. Cephalothin Prophylaxis in Cardiac Valve Surgery. A Prospective, Double-Blind Comparison of Two-Day and Six-Day Regimens. J. Thorac. Cardiovasc. Surg. 1977, 73, 470–479.
- Zelenitsky, S.A.; Ariano, R.E.; Harding, G.K.M.; Silverman, R.E. Antibiotic Pharmacodynamics in Surgical Prophylaxis: An Association between Intraoperative Antibiotic Concentrations and Efficacy. Antimicrob. Agents Chemother. 2002, 46, 3026–3030.
- Zelenitsky, S.A.; Silverman, R.E.; Duckworth, H.; Harding, G.K.M. A Prospective, Randomized, Double-Blind Studyof Single High Dose versus Multiple Standard Dose Gentamicin Both in Combination Withmetronidazole for Colorectal Surgicalprophylaxis. J. Hosp. Infect. 2000, 46, 135–140.
- Zelenitsky, S.A.; Calic, D.; Arora, R.C.; Grocott, H.P.; Lakowski, T.M.; Lillico, R.; Ariano, R.E. Antimicrobial Prophylaxis for Patients Undergoing Cardiac Surgery: Intraoperative Cefazolin Concentrations and Sternal Wound Infections. Antimicrob. Agents Chemother. 2018, 62, e01360-18.
- Calic, D.; Ariano, R.E.; Arora, R.C.; Grocott, H.P.; Lakowski, T.M.; Lillico, R.; Zelenitsky, S.A. Evaluation of Cefazolin Antimicrobial Prophylaxis during Cardiac Surgery with Cardiopulmonary Bypass. J. Antimicrob. Chemother. 2018, 73, 768–771.
- Takayama, Y.; Komatsu, T.; Nakamura, T.; Tomoda, Y.; Toda, M.; Miura, H.; Sato, T.; Atsuda, K.; Okamoto, H.; Hanaki, H. Association of Serum and Fat Tissue Antibiotic Concentrations with Surgical Site Infections in Lower Gastrointestinal Surgery. Surgery 2022, 171, 1000–1005.
- Mouton, J.W.; Theuretzbacher, U.; Craig, W.A.; Tulkens, P.M.; Derendorf, H.; Cars, O. Tissue Concentrations: Do We Ever Learn? J. Antimicrob. Chemother. 2007, 61, 235–237.
- Jager, N.G.L.; Van Hest, R.M.; Lipman, J.; Roberts, J.A.; Cotta, M.O. Antibiotic Exposure at the Site of Infection: Principles and Assessment of Tissue Penetration. Expert Rev. Clin. Pharmacol. 2019, 12, 623–634.
- Dadhwal, U.S. A Few Comments on “Association of Serum and Fat Tissue Antibiotic Concentrations with Surgical Site Infections in Lower Gastrointestinal Surgery” by Yoko Takayama et al. Surgery 2023, 173, 558–559.
- Chua, H.C.; Tam, V.H. Optimizing Clinical Outcomes Through Rational Dosing Strategies: Roles of Pharmacokinetic/Pharmacodynamic Modeling Tools. Open Forum Infect. Dis. 2022, 9, ofac626.
- De Velde, F.; Mouton, J.W.; De Winter, B.C.M.; Van Gelder, T.; Koch, B.C.P. Clinical Applications of Population Pharmacokinetic Models of Antibiotics: Challenges and Perspectives. Pharmacol. Res. 2018, 134, 280–288.
- Grayson, M.L.; Cosgrove, S.; Crowe, S.; Hope, W.; McCarthy, J.; Mills, J.; Mouton, J.W.; Paterson, D. (Eds.) Kucers’ the Use of Antibiotics: A Clinical Review of Antibacterial, Antifungal, Antiparasitic, and Antiviral Drugs, 7th ed.; CRC Press: Boca Raton, FL, USA, 2017; ISBN 978-1-4987-4796-7.
- Rondon, A.J.; Kheir, M.M.; Tan, T.L.; Shohat, N.; Greenky, M.R.; Parvizi, J. Cefazolin Prophylaxis for Total Joint Arthroplasty: Obese Patients Are Frequently Underdosed and at Increased Risk of Periprosthetic Joint Infection. J. Arthroplast. 2018, 33, 3551–3554.
- Karamian, B.A.; Toci, G.R.; Lambrechts, M.J.; Siegel, N.; Sherman, M.; Canseco, J.A.; Hilibrand, A.S.; Kepler, C.K.; Vaccaro, A.R.; Schroeder, G.D. Cefazolin Prophylaxis in Spine Surgery: Patients Are Frequently Underdosed and at Increased Risk for Infection. Spine J. 2022, 22, 1442–1450.
- Coates, M.; Shield, A.; Peterson, G.M.; Hussain, Z. Prophylactic Cefazolin Dosing in Obesity—A Systematic Review. Obes. Surg. 2022, 32, 3138–3149.
- Ahmadzia, H.K.; Patel, E.M.; Joshi, D.; Liao, C.; Witter, F.; Heine, R.P.; Coleman, J.S. Obstetric Surgical Site Infections: 2 Grams Compared With 3 Grams of Cefazolin in Morbidly Obese Women. Obstet. Gynecol. 2015, 126, 708–715.
- Peppard, W.J.; Eberle, D.G.; Kugler, N.W.; Mabrey, D.M.; Weigelt, J.A. Association between Pre-Operative Cefazolin Dose and Surgical Site Infection in Obese Patients. Surg. Infect. 2017, 18, 485–490.
- Hussain, Z.; Curtain, C.; Mirkazemi, C.; Gadd, K.; Peterson, G.M.; Zaidi, S.T.R. Prophylactic Cefazolin Dosing and Surgical Site Infections: Does the Dose Matter in Obese Patients? Obes. Surg. 2019, 29, 159–165.
- Hites, M.; Deprez, G.; Wolff, F.; Ickx, B.; Verleije, A.; Closset, J.; Loi, P.; Prévost, J.; Taccone, F.S.; Racapé, J.; et al. Evaluation of Total Body Weight and Body Mass Index Cut-Offs for Increased Cefazolin Dose for Surgical Prophylaxis. Int. J. Antimicrob. Agents 2016, 48, 633–640.
- Classen, D.C.; Evans, R.S.; Pestotnik, S.L.; Horn, S.D.; Menlove, R.L.; Burke, J.P. The Timing of Prophylactic Administration of Antibiotics and the Risk of Surgical-Wound Infection. N. Engl. J. Med. 1992, 326, 281–286.
- Steinberg, J.P.; Braun, B.I.; Hellinger, W.C.; Kusek, L.; Bozikis, M.R.; Bush, A.J.; Dellinger, E.P.; Burke, J.P.; Simmons, B.; Kritchevsky, S.B. Timing of Antimicrobial Prophylaxis and the Risk of Surgical Site Infections: Results From the Trial to Reduce Antimicrobial Prophylaxis Errors. Ann. Surg. 2009, 250, 10–16.
- De Jonge, S.W.; Gans, S.L.; Atema, J.J.; Solomkin, J.S.; Dellinger, P.E.; Boermeester, M.A. Timing of Preoperative Antibiotic Prophylaxis in 54,552 Patients and the Risk of Surgical Site Infection: A Systematic Review and Meta-Analysis. Medicine 2017, 96, e6903.
- Koch, C.G.; Nowicki, E.R.; Rajeswaran, J.; Gordon, S.M.; Sabik, J.F.; Blackstone, E.H. When the Timing Is Right: Antibiotic Timing and Infection after Cardiac Surgery. J. Thorac. Cardiovasc. Surg. 2012, 4, 931–937.e4.
- Koch, C.G.; Li, L.; Hixson, E.; Tang, A.; Gordon, S.; Longworth, D.; Phillips, S.; Blackstone, E.; Henderson, M.J. Is It Time to Refine? An Exploration and Simulation of Optimal Antibiotic Timing in General Surgery. J. Am. Coll. Surg. 2013, 217, 628.
- Sommerstein, R.; Atkinson, A.; Kuster, S.P.; Thurneysen, M.; Genoni, M.; Troillet, N.; Marschall, J.; Widmer, A.F.; Swissnoso; Balmelli, C.; et al. Antimicrobial Prophylaxis and the Prevention of Surgical Site Infection in Cardiac Surgery: An Analysis of 21,007 Patients in Switzerland†. Eur. J. Cardio-Thorac. Surg. 2019, 56, 800–806.
- Weber, W.P.; Mujagic, E.; Zwahlen, M.; Bundi, M.; Hoffmann, H.; Soysal, S.D.; Kraljević, M.; Delko, T.; Von Strauss, M.; Iselin, L.; et al. Timing of Surgical Antimicrobial Prophylaxis: A Phase 3 Randomised Controlled Trial. Lancet Infect. Dis. 2017, 17, 605–614.
- De Jonge, S.W.; Boldingh, Q.J.J.; Koch, A.H.; Daniels, L.; De Vries, E.N.; Spijkerman, I.J.B.; Ankum, W.M.; Kerkhoffs, G.M.M.J.; Dijkgraaf, M.G.; Hollmann, M.W.; et al. Timing of Preoperative Antibiotic Prophylaxis and Surgical Site Infection: TAPAS, An Observational Cohort Study. Ann. Surg. 2021, 274, e308–e314.
- Paasch, C.; Schildberg, C.; Lünse, S.; Heisler, S.; Meyer, J.; Kirbach, J.; Kobelt, E.; Hunger, R.; Haller, I.-E.; Helmke, C.; et al. Optimal Timing for Antimicrobial Prophylaxis to Reduce Surgical Site Infections: A Retrospective Analysis of 531 Patients. Sci. Rep. 2023, 13, 9405.
- Weber, W.P.; Marti, W.R.; Zwahlen, M.; Misteli, H.; Rosenthal, R.; Reck, S.; Fueglistaler, P.; Bolli, M.; Trampuz, A.; Oertli, D.; et al. The Timing of Surgical Antimicrobial Prophylaxis. Ann. Surg. 2008, 247, 918.
- Naik, B.I.; Roger, C.; Ikeda, K.; Todorovic, M.S.; Wallis, S.C.; Lipman, J.; Roberts, J.A. Comparative Total and Unbound Pharmacokinetics of Cefazolin Administered by Bolus versus Continuous Infusion in Patients Undergoing Major Surgery: A Randomized Controlled Trial. Br. J. Anaesth. 2017, 118, 876–882.
- Douglas, A.; Udy, A.A.; Wallis, S.C.; Jarrett, P.; Stuart, J.; Lassig-Smith, M.; Deans, R.; Roberts, M.S.; Taraporewalla, K.; Jenkins, J.; et al. Plasma and Tissue Pharmacokinetics of Cefazolin in Patients Undergoing Elective and Semielective Abdominal Aortic Aneurysm Open Repair Surgery. Antimicrob. Agents Chemother. 2011, 55, 5238–5242.
- Himebauch, A.S.; Nicolson, S.C.; Sisko, M.; Moorthy, G.; Fuller, S.; Gaynor, J.W.; Zuppa, A.F.; Fox, E.; Kilbaugh, T.J. Skeletal Muscle and Plasma Concentrations of Cefazolin during Cardiac Surgery in Infants. J. Thorac. Cardiovasc. Surg. 2014, 148, 2634–2641.
- Himebauch, A.S.; Sankar, W.N.; Flynn, J.M.; Sisko, M.T.; Moorthy, G.S.; Gerber, J.S.; Zuppa, A.F.; Fox, E.; Dormans, J.P.; Kilbaugh, T.J. Skeletal Muscle and Plasma Concentrations of Cefazolin during Complex Paediatric Spinal Surgery. Br. J. Anaesth. 2016, 117, 87–94.
- Caruso, T.J.; Wang, E.Y.; Colletti, A.A.; Sharek, P.J. Intraoperative Antibiotic Redosing Compliance and the Extended Postoperative Recovery Period: Often Overlooked Areas That May Reduce Surgical Site Infections. Pediatr. Anesth. 2019, 29, 290–291.
- Wolfhagen, N.; Boldingh, Q.J.J.; De Lange, M.; Boermeester, M.A.; De Jonge, S.W. Intraoperative Redosing of Surgical Antibiotic Prophylaxis in Addition to Preoperative Prophylaxis Versus Single-Dose Prophylaxis for the Prevention of Surgical Site Infection: A Meta-Analysis and GRADE Recommendation. Ann. Surg. 2022, 275, 1050–1057.
- Lanoiselée, J.; Chaux, R.; Hodin, S.; Bourayou, S.; Gibert, A.; Philippot, R.; Molliex, S.; Zufferey, P.J.; Delavenne, X.; Ollier, E. Population Pharmacokinetic Model of Cefazolin in Total Hip Arthroplasty. Sci. Rep. 2021, 11, 19763.
