Drug bioavailability is a crucial aspect of pharmacology, affecting the effectiveness of drug therapy. Understanding how drugs are absorbed, distributed, metabolized, and eliminated in patients’ bodies is essential to ensure proper and safe treatment. In addition to biochemical activity, bioavailability also plays a critical role in achieving the desired therapeutic effects. This may seem obvious, but it is worth noting that a drug can only produce the expected effect if the proper level of concentration can be achieved at the desired point in a patient’s body. Given the differences between patients, drug dosages, and administration forms, understanding and controlling bioavailability has become a priority in pharmacology.
- bioavailability
- pharmacokinetics
- therapeutic effectiveness
- pharmaceutical innovations
1. Introduction
2. Bioavailability of Drugs: Basic Concepts and Controlling Factors
The bioavailability of a drug describes the level of absorption of the active substance contained therein and the speed at which it is absorbed from the form administered to the patient, becoming available in the targeted location of the body, usually in the bloodstream. The bioavailability of a drug determines the proportion of the active substance available in the body in relation to its amount in the drug [15][11]. Drug bioavailability measurements allow for the assessment of the absorption efficiency of a drug, including its absolute and relative bioavailability, the time to reach maximum concentration, and the area under the concentration–time curve [16][12]. Absolute bioavailability is defined as a measurement that determines the percentage of the active substance entering the bloodstream after administration of a drug when the reference standard is an intravenous dose. It expresses the efficiency of the absorption of the active substance by the body. It is usually less than 100%, since not all of the active substance is absorbed in the gastrointestinal tract [17][13]. Relative bioavailability is expressed as the ratio of the bioavailability of two dosage forms of the same drug (Figure 1). The time to reach maximum concentration (tmax) measures the time it takes for an active ingredient to reach its highest concentration in the blood after drug administration. tmax is an important parameter because it can affect the rate of action of a drug. The area under the curve (AUC) measures the total amount of an active substance absorbed and available in the bloodstream as a function of time. The AUC is used to assess the total exposure of the body to an active substance (Figure 1) [19][14]. Measurements of drug bioavailability are essential for evaluating the pharmacokinetics and pharmacodynamics of drugs and for determining appropriate therapeutic doses. They are also crucial for developing new drugs and evaluating the efficacy of different administration forms [16,20][12][15].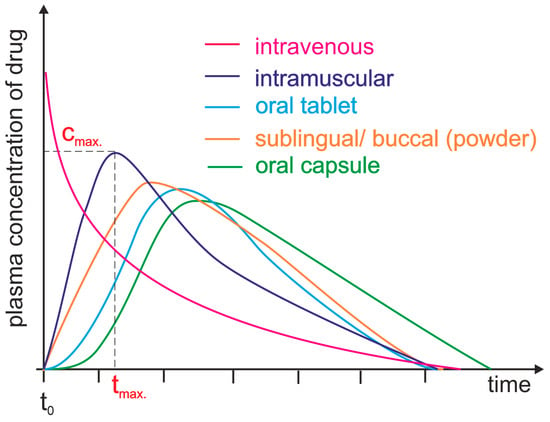
43. Methods for Assessing Drug Bioavailability
Three main categories of methods are used to assess drug bioavailability—in vitro methods, in vivo methods, and new techniques and tools. In vitro methods are laboratory-based and involve studying drug bioavailability under controlled conditions outside the living organism. These methods enable researchers to study drug absorption, metabolism, and transport processes and to evaluate the impact of physicochemical factors on drug bioavailability [68][46]. There are different in vitro methods used for drug testing. One such method is drug solubility testing, in which the solubility of a drug is measured in various environments, including the use of buffer solutions with different pH levels. This test helps determine how well a drug dissolves and is absorbed in the digestive environment [69][47]. Cell cultures are another example in which human or animal cells are used to simulate processes such as drug absorption, metabolism, and transport. These cultures can also be used to examine the effects of digestive enzyme activity or transporters on bioavailability [72][48]. Narrow liver microsomes containing microsomal enzymes accurately represent the liver’s metabolic activity, with various applications. Studying drug metabolism using hepatic microsomes allows for the estimation of how a drug may be metabolized before it is eliminated from the system [73][49]. Through in vivo techniques, the bioavailability of a drug in a living system can be investigated. These methods consider the entire bioavailability process, including drug interactions, metabolism, elimination, and patient response. In vivo methods involve administering drugs to patients or animals and then analyzing samples of blood, urine, or other body fluids to determine the concentration of the drug over time [74][50]. With the advancements in science and technology, new methods and tools for evaluating drug bioavailability are being developed. Medical imaging techniques, such as computed tomography (CT), magnetic resonance imaging (MRI), and positron emission tomography (PET), are some of the techniques that are currently being developed. These techniques enable the monitoring and tracking of drug distribution in the body, allowing for the observation of the drug’s path post-administration and the assessment of its concentration in various tissues and organs [79][51]. Other advanced techniques include pharmacogenetic studies, which deal with the impact of genetic differences on drug responses. They allow for the determination of the effect of genetic polymorphism in metabolic enzymes and transporters on drug bioavailability in different individuals [80][52]. Pharmacokinetic modeling, or computer simulation, has become a valuable medical tool that uses mathematical models and algorithms to predict drug performance in living organisms, considering factors like dosage, absorption, transport rates, and enzyme concentrations, thereby optimizing treatment efficacy [81][53].54. Drugs with Poorly Described Bioavailability
Drugs with poorly described bioavailability are those for which there is limited information regarding the ADME process in the body. There may be various reasons for the lack of detailed data on drug bioavailability [21][16]. In this context, four distinct groups of drugs can be identified: (1) drugs with complex metabolism and elimination, (2) drugs with limited solubility, (3) drugs with specific absorption, and (4) other cases. Drugs with complex metabolism and elimination undergo intricate chemical metabolism and removal processes, influenced by factors such as interactions with other drugs, differences in gene-type metabolism, diseases, and the overall health of the patient [34][23]. Warfarin is a drug used for preventing and treating thrombosis. However, its metabolism is quite complex. It is mainly metabolized in the liver by cytochrome P450 enzymes through a series of steps involving hydroxylation, reduction, and conjugation. After metabolism, the drug is eliminated from the body as metabolites through the kidneys. However, the activity of cytochrome P450 enzymes varies widely due to genetic differences and interactions with other drugs and food. Carbamazepine is a medication used to treat epilepsy, trigeminal neuralgia, and bipolar affective disorder. Certain enzymes, particularly CYP3A4 and CYP2C9 isoenzymes, metabolize the drug in the liver. Its metabolites are excreted in both urine and feces. Carbamazepine’s metabolism and bioavailability can be significantly affected by interactions with other drugs that inhibit or induce the cytochrome enzymes [84,85][54][55]. Digoxin is a medication used to treat heart failure and certain cardiac arrhythmias. Although it is primarily metabolized in the liver, it is eliminated from the body mainly through renal excretion. The metabolism of digoxin is complex, with glucuronidation being the primary metabolic pathway. However, the therapeutic window for digoxin is narrow, which means that even small changes in bioavailability and elimination can cause toxicity or a lack of effectiveness [86,87][56][57]. Drugs with low water solubility show difficulty dissolving in body fluids, which affects their bioavailability and therapeutic effectiveness due to the hydrophobicity of the drug or the formation of complexes with other substances [88,89][58][59]. Analgesics like diclofenac possess limited solubility in water, which adversely affects their absorption from the gastrointestinal tract and therefore, their bioavailability. Various strategies can be employed to increase the solubility and improve the absorption of these drugs. These may include modifying the formulation to obtain a more soluble form or using specific carriers that facilitate drug delivery to the site of action [90][60]. Certain antifungal medications, including itraconazole, exhibit a restricted capacity to dissolve in water, reducing their absorption in the gastrointestinal tract. To overcome this issue, solubility-enhancing substances are administered, or suitable formulations are developed to enhance the effectiveness and bioavailability of these drugs [91][61]. Paclitaxel is a common anticancer drug used to treat various malignancies in humans. However, it shows limited solubility in water, which makes it difficult to administer and absorb. To overcome this challenge, unique formulations enhance its solubility and delivery to the site of action [92][62]. Drugs with specific absorption are those whose absorption in the gastrointestinal tract depends on specific mechanisms or conditions. These drugs may be subject to interactions with other substances, pH changes, the presence of transporters, or specific absorption processes. One example of such a drug is levothyroxine, a synthetic hormone used to treat hypothyroidism. Its absorption depends on the presence of iodine in the gut. Iodine ions are essential for forming the active thyroid hormone (thyroxine—T4). Consequently, patients taking levothyroxine must take it on an empty stomach and avoid substances such as calcium, iron, or fiber that may affect the absorption of iodine and the drug itself [95][63]. Apart from to the examples outlined above, there are numerous other instances in which drug bioavailability is poorly defined or understood. Herbal treatments, anticancer medications, and novel medications are some examples of these. The bioavailability of certain plant-based drugs, such as herbal dietary supplements, can be inadequately described due to the complexity of their active ingredients, which can vary in their chemical form [99,100][64][65]. Hypericin is a natural compound in the St. John’s wort (Hypericum perforatum) plant. It is used for various health conditions, including treating depression and fighting against different viruses. However, the bioavailability of hypericin is not well understood because it is a complex chemical compound that can undergo several transformations in the body. Different forms of hypericin may include various pharmacokinetic properties, as well as bioavailability [99][64]. Data on bioavailability may be limited for new drugs that have not undergone comprehensive clinical trials. The absorption, distribution, metabolism, and elimination of a drug are all evaluated in basic pharmacokinetic studies. Nevertheless, data regarding bioavailability are scarce, particularly in large-scale clinical trials with a diverse patient group [21][16]. An example of a new drug with limited information regarding its bioavailability is tecovirimat (Tpoxx), an antiviral drug that has demonstrated efficacy in animal studies and has been approved by the Food and Drug Administration for the treatment of smallpox, a severe and life-threatening infection caused by the Variola virus of the Orthopoxvirus genus. It belongs to a group of drugs known as orthopoxvirus-specific antivirals. Tecovirimat is an investigational drug and is not currently approved for routine use. It is used in emergencies as part of preparatory measures against smallpox outbreaks [103][66].65. Conclusions
Bioavailability data for many active compounds is sparse, despite substantial pharmacological study. These extensive pharmacokinetic studies are required for a broad list of drugs [119][67]. However, such studies are expensive and complicated; thus, few are performed, and therefore, few can be added to the bioavailability dataset [106][68]. Moreover, the pharmacokinetic characteristics of individuals vary greatly. Age, gender, genetics, health, and other parameters affect drug absorption and transport. However, a number of results obtained from such studies can be utilized to build generalized models showing the action of APIs in the human body [24][19]. It was established that drug bioavailability depends on administration [121][69]. Intravenous medications enter the bloodstream directly, while oral pharmaceuticals must pass through the digestive system and may be destroyed or absorbed incorrectly. Many bioavailability details remain undiscovered, despite broad studies for varied dosing techniques [122][70]. Since not all drug-food interactions are known, the need remains for further thorough studies of this aspect [123][71]. In regards to drug therapy safety, bioavailability studies determine doses to reduce dangerous blood active component concentrations, identify medication interaction risk factors, and improve safety [124][72]. Individualized treatment based on genetics, health, age, and drug interactions is possible because these studies disclose internal factors impacting drug absorption, distribution, and metabolism [125][73]. Medication bioavailability research is essential for treating rare and complex diseases. Understanding the active ingredient absorption derived from tablets, capsules, injections, and patches improves drug development. Understanding bioavailability improves drug use and health care by optimizing prescription design, treating rare disorders, and discovering new formulations [126][74].References
- Herkenne, C.; Alberti, I.; Naik, A.; Kalia, Y.N.; Mathy, F.X.; Preat, V.; Guy, R.H. In vivo methods for the assessment of topical drug bioavailability. Pharm. Res. 2008, 25, 87–103.
- Olivares-Morales, A.; Hatley, O.J.; Turner, D.; Galetin, A.; Aarons, L.; Rostami-Hodjegan, A. The use of ROC analysis for the qualitative prediction of human oral bioavailability from animal data. Pharm. Res. 2014, 31, 720–730.
- Caldwell, J.; Gardner, I.; Swales, N. An introduction to drug disposition: The basic principles of absorption, distribution, metabolism, and excretion. Toxicol. Pathol. 1995, 23, 102–114.
- Martinez, M.N.; Amidon, G.L. A mechanistic approach to understanding the factors affecting drug absorption: A review of fundamentals. J. Clin. Pharmacol. 2002, 42, 620–643.
- Doogue, M.P.; Polasek, T.M. The ABCD of clinical pharmacokinetics. Ther. Adv. Drug Saf. 2013, 4, 5–7.
- Patel, M.; Kumar, R.; Kishor, K.; Mlsna, T.; Pittman, C.U., Jr.; Mohan, D. Pharmaceuticals of emerging concern in aquatic systems: Chemistry, occurrence, effects, and removal methods. Chem. Rev. 2019, 119, 3510–3673.
- Hatton, G.B.; Madla, C.M.; Rabbie, S.C.; Basit, A.W. Gut reaction: Impact of systemic diseases on gastrointestinal physiology and drug absorption. Drug Discov. Today 2019, 24, 417–427.
- Wagner, J.G. History of pharmacokinetics. Pharmacol. Therapeut. 1981, 12, 537–562.
- Lin, L.; Wong, H. Predicting oral drug absorption: Mini review on physiologically-based pharmacokinetic models. Pharmaceutics 2017, 9, 41.
- Wang, Y.; Wang, Y.; Pi, C.; Feng, X.; Hou, Y.; Zhao, L.; Wei, Y. The influence of nanoparticle properties on oral bioavailability of drugs. Int. J. Nanomed. 2020, 15, 6295–6310.
- Alston, A.B.; Digigow, R.; Fluhmann, B.; Wacker, M.G. Putting square pegs in round holes: Why traditional pharmacokinetic principles cannot universally be applied to iron-carbohydrate complexes. Eur. J. Pharm. Biopharm. 2023, 188, 6–14.
- Hedaya, M.A. Basic Pharmacokinetics, 2nd ed.; CRC Press: Boca Raton, FL, USA, 2012.
- Wang, F.; Yang, G.; Zhou, Y.; Song, H.; Xiong, L.; Wang, L.; Shen, X. Pharmacokinetics of niazirin from Moringa oleifera Lam in rats by UPLC-MS/MS: Absolute bioavailability and dose proportionality. eFood 2022, 3, e39.
- Currie, G.M. Pharmacology, part 2: Introduction to pharmacokinetics. J. Nucl. Med. Technol. 2018, 46, 221–230.
- Tuntland, T.; Ethell, B.; Kosaka, T.; Blasco, F.; Zang, R.X.; Jain, M.; Hoffmaster, K. Implementation of pharmacokinetic and pharmacodynamic strategies in early research phases of drug discovery and development at Novartis Institute of Biomedical Research. Front. Pharmacol. 2014, 5, 174.
- Wei, M.; Zhang, X.; Pan, X.; Wang, B.; Ji, C.; Qi, Y.; Zhang, J.Z. HobPre: Accurate prediction of human oral bioavailability for small molecules. J. Cheminform. 2022, 14, 1–10.
- Rowland, M.; Tozer, T.N. Clinical Pharmacokinetics and Pharmacodynamics: Concepts and Applications, 4th ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2011.
- Kalaimathi, K.; Shine, K.; Gandhi, G.R.; Vijayakumar, S.; Ayyanar, M.; Amalraj, S.; Jose, J. Cyanobacterial metabolites as novel potential suppressors of breast cancer: A comparative in silico pharmacological assessment. Intell. Pharm. 2023, 1, 133–144.
- Stillhart, C.; Vučićević, K.; Augustijns, P.; Basit, A.W.; Batchelor, H.; Flanagan, T.R.; Müllertz, A. Impact of gastrointestinal physiology on drug absorption in special populations—An UNGAP review. Eur. J. Pharm. Sci. 2020, 147, 105280.
- Belayneh, A.; Molla, F. The effect of coffee on pharmacokinetic properties of drugs: A review. Biomed. Res. Int. 2020, 2020, 7909703.
- Sochacka, J.; Lipska, I. Rola α1-kwaśnej glikoproteiny surowicy krwi ludzkiej w procesie wiązania leków, sytuacja w Polsce i na świecie. Farmacja Polska 2014, 70, 55–62.
- Park, J.H.; Pyun, W.Y.; Park, H.W. Cancer metabolism: Phenotype, signaling and therapeutic targets. Cells 2020, 9, 2308.
- Li, Y.; Meng, Q.; Yang, M.; Liu, D.; Hou, X.; Tang, L.; Bi, H. Current trends in drug metabolism and pharmacokinetics. Acta Pharm. Sin. B 2019, 9, 1113–1144.
- Alqahtani, M.S.; Kazi, M.; Alsenaidy, M.A.; Ahmad, M.Z. Advances in oral drug delivery. Front. Pharmacol. 2021, 12, 618411.
- Settimo, L.; Bellman, K.; Knegtel, R.M. Comparison of the accuracy of experimental and predicted pKa values of basic and acidic compounds. Pharm. Res. 2014, 31, 1082–1095.
- Gaohua, L.; Miao, X.; Dou, L. Crosstalk of physiological pH and chemical pKa under the umbrella of physiologically based pharmacokinetic modeling of drug absorption, distribution, metabolism, excretion, and toxicity. Expert Opin. Drug Met. 2021, 17, 1103–1124.
- Vinarov, Z.; Abdallah, M.; Agundez, J.A.; Allegaert, K.; Basit, A.W.; Braeckmans, M.; Augustijns, P. Impact of gastrointestinal tract variability on oral drug absorption and pharmacokinetics: An UNGAP review. Eur. J. Pharm. Sci. 2021, 162, 105812.
- Wong, K.H.; Riaz, M.K.; Xie, Y.; Zhang, X.; Liu, Q.; Chen, H.; Yang, Z. Review of current strategies for delivering Alzheimer’s disease drugs across the blood-brain barrier. Int. J. Mol. Sci. 2019, 20, 381.
- Elliott, R.O.; He, M. Unlocking the Power of Exosomes for Crossing Biological Barriers in Drug Delivery. Pharmaceutics 2021, 13, 122.
- Kratzer, I.; Ek, J.; Stolp, H. The molecular anatomy and functions of the choroid plexus in healthy and diseased brain. Biochim. Biophys. Acta (BBA)-Biomembr. 2020, 1862, 183430.
- Uchida, Y.; Goto, R.; Usui, T.; Tachikawa, M.; Terasaki, T. Blood-Arachnoid Barrier as a Dynamic Physiological and Pharmacological Interface between Cerebrospinal Fluid and Blood. In Drug Delivery to the Brain: Physiological Concepts, Methodologies and Approaches; Springer International Publishing: Cham, Germany, 2022; pp. 93–121.
- Kiecker, C. The origins of the circumventricular organs. J. Anat. 2018, 232, 540–553.
- Pandit, R.; Chen, L.; Götz, J. The blood-brain barrier: Physiology and strategies for drug delivery. Adv. Drug Deliver. Rev. 2020, 165, 1–14.
- Villaseñor, R.; Lampe, J.; Schwaninger, M.; Collin, L. Intracellular transport and regulation of transcytosis across the blood–brain barrier. Cell. Mol. Life Sci. 2019, 76, 1081–1092.
- Yazdani, S.; Jaldin-Fincati, J.R.; Pereira, R.V.; Klip, A. Endothelial cell barriers: Transport of molecules between blood and tissues. Traffic 2019, 20, 390–403.
- Kadry, H.; Noorani, B.; Cucullo, L. A blood–brain barrier overview on structure, function, impairment, and biomarkers of integrity. Fluids Barriers CNS 2020, 17, 1–24.
- Sánchez-Félix, M.; Burke, M.; Chen, H.H.; Patterson, C.; Mittal, S. Predicting bioavailability of monoclonal antibodies after subcutaneous administration: Open innovation challenge. Adv. Drug Deliver. Rev. 2020, 167, 66–77.
- Bannigan, P.; Aldeghi, M.; Bao, Z.; Häse, F.; Aspuru-Guzik, A.; Allen, C. Machine learning directed drug formulation development. Adv. Drug Deliver. Rev. 2021, 175, 113806.
- Tanguay, M.; Girard, J.; Scarsi, C.; Mautone, G.; Larouche, R. Pharmacokinetics and comparative bioavailability of a levothyroxine sodium oral solution and soft capsule. Clin. Pharm. Dug Dev. 2019, 8, 521–528.
- Shariare, M.H.; Altamimi, M.A.; Marzan, A.L.; Tabassum, R.; Jahan, B.; Reza, H.M.; Kazi, M. In vitro dissolution and bioavailability study of furosemide nanosuspension prepared using design of experiment (DoE). Saudi Pharm. J. 2019, 27, 96–105.
- Alghamdi, M.A.; Fallica, A.N.; Virzì, N.; Kesharwani, P.; Pittalà, V.; Greish, K. The promise of nanotechnology in personalized medicine. J. Pers. Med. 2022, 12, 673.
- Leopoldo, M.; Nardulli, P.; Contino, M.; Leonetti, F.; Luurtsema, G.; Colabufo, N.A. An updated patent review on P-glycoprotein inhibitors (2011–2018). Expert Opin. Ther. Pat. 2019, 29, 455–461.
- Australian Product Information Tivicay (dolutegravir) Film-Coated Tablets and TIVICAY PD (dolutegravir) Dispersible Tablets. Available online: https://www.tga.gov.au/sites/default/files/2022-08/auspar-tivicay-tivicay-pd-220705-pi.pdf (accessed on 10 October 2023).
- Shultz, M.D. Two decades under the influence of the rule of five and the changing properties of approved oral drugs: Miniperspective. J. Med. Chem. 2018, 62, 1701–1714.
- U.S. FDA Approves GlaxoSmithKline’s HIV Drug Tivicay. Available online: https://www.reuters.com/article/us-glaxosmithkline-hivdrug-idUSBRE97B0WU20130812 (accessed on 5 October 2023).
- Bagchi, S.; Chhibber, T.; Lahooti, B.; Verma, A.; Borse, V.; Jayant, R.D. In-vitro blood-brain barrier models for drug screening and permeation studies: An overview. Drug Des. Dev. Ther. 2019, 13, 3591–3605.
- Ren, S.; Liu, M.; Hong, C.; Li, G.; Sun, J.; Wang, J.; Xie, Y. The effects of pH, surfactant, ion concentration, coformer, and molecular arrangement on the solubility behavior of myricetin cocrystals. Acta Pharm. Sin. B 2019, 9, 59–73.
- Santbergen, M.J.; Van der Zande, M.; Gerssen, A.; Bouwmeester, H.; Nielen, M.W. Dynamic in vitro intestinal barrier model coupled to chip-based liquid chromatography mass spectrometry for oral bioavailability studies. Anal. Bioanal. Chem. 2020, 412, 1111–1122.
- Attwa, M.W.; AlRabiah, H.; Mostafa, G.A.; Kadi, A.A. Development of an LC-MS/MS method for quantification of sapitinib in human liver microsomes: In silico and in vitro metabolic stability evaluation. Molecules 2023, 28, 2322.
- Shinha, K.; Nihei, W.; Ono, T.; Nakazato, R.; Kimura, H. A pharmacokinetic–pharmacodynamic model based on multi-organ-on-a-chip for drug–drug interaction studies. Biomicrofluidics 2020, 14, 044108.
- Perez-Medina, C.; Teunissen, A.J.; Kluza, E.; Mulder, W.J.; Van der Meel, R. Nuclear imaging approaches facilitating nanomedicine translation. Adv. Drug Deliver. Rev. 2020, 154, 123–141.
- Kulkarni, J.A.; Witzigmann, D.; Thomson, S.B.; Chen, S.; Leavitt, B.R.; Cullis, P.R.; van der Meel, R. The current landscape of nucleic acid therapeutics. Nat. Nanotechnol. 2021, 16, 630–643.
- Dałek, P.; Drabik, D.; Wołczańska, H.; Foryś, A.; Jagas, M.; Jędruchniewicz, N.; Langner, M. Bioavailability by design—Vitamin D3 liposomal delivery vehicles. Nanomed. Nanotechnol. Biol. Med. 2022, 43, 102552.
- Li, H.; Zhang, M.; Xiong, L.; Feng, W.; Williams, R.O., III. Bioavailability improvement of carbamazepine via oral administration of modified-release amorphous solid dispersions in rats. Pharmaceutics 2020, 12, 11–1023.
- Fuhr, L.M.; Marok, F.Z.; Hanke, N.; Selzer, D.; Lehr, T. Pharmacokinetics of the CYP3A4 and CYP2B6 inducer carbamazepine and its drug–drug interaction potential: A physiologically based pharmacokinetic modeling approach. Pharmaceutics 2021, 13, 270.
- Hsin, C.H.; Stoffel, M.S.; Gazzaz, M.; Schaeffeler, E.; Schwab, M.; Fuhr, U.; Taubert, M. Combinations of common SNPs of the transporter gene ABCB1 influence apparent bioavailability, but not renal elimination of oral digoxin. Sci. Rep. 2020, 10, 12457.
- Ibrahim, N.A.M. An up-to-date review of digoxin toxicity and its management. Int. J. Res. Pharm. Pharm. Sci. 2019, 4, 59–64.
- Pawar, S.R.; Barhate, S.D. Solubility enhancement (Solid Dispersions) novel boon to increase bioavailability. J. Drug Deliv. Ther. 2019, 9, 583–590.
- Kareem, S.H.K.A. Quality by Design Approach for Bioavailability Enhancement of Some Hydrophobic Drugs. Available online: https://shodhgangotri.inflibnet.ac.in/bitstream/20.500.14146/13393/1/final%20synopsis%20corrected.pdf (accessed on 5 October 2023).
- Pireddu, R.; Schlich, M.; Marceddu, S.; Valenti, D.; Pini, E.; Fadda, A.M.; Sinico, C. Nanosuspensions and microneedles roller as a combined approach to enhance diclofenac topical bioavailability. Pharmaceutics 2020, 12, 1140.
- Sardana, K.; Mathachan, S.R. Super bioavailable itraconazole and its place and relevance in recalcitrant dermatophytosis: Revisiting skin levels of itraconazole and minimum inhibitory concentration data. Indian Dermatol. Online J. 2021, 12, 1.
- Bardelmeijer, H.A.; Beijnen, J.H.; Brouwer, K.R.; Rosing, H.; Nooijen, W.J.; Schellens, J.H.; van Tellingen, O. Increased oral bioavailability of paclitaxel by GF120918 in mice through selective modulation of P-glycoprotein. Clin. Cancer Res. 2000, 6, 4416–4421.
- Virili, C.; Brusca, N.; Capriello, S.; Centanni, M. Levothyroxine therapy in gastric malabsorptive disorders. Front. Endocrinol. 2021, 11, 621616.
- Oglah, M.K.; Bashir, M.K.; Mustafa, Y.F. Hypericin and its analogues: A review of their biological activities. Turk. J. Field Crops 2021, 26, 259–269.
- Lin, Y.; Li, Y.; Zeng, Y.; Tian, B.; Qu, X.; Yuan, Q.; Song, Y. Pharmacology, toxicity, bioavailability, and formulation of magnolol: An update. Front. Pharmacol. 2021, 12, 632767.
- O’Laughlin, K.; Tobolowsky, F.A.; Elmor, R.; Overton, R.; O’Connor, S.M.; Damon, I.K.; Veillard, M. Clinical use of tecovirimat (Tpoxx) for treatment of monkeypox under an investigational new drug protocol—United States, May–August 2022. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 1190.
- Bohn, T.; Desmarchelier, C.; Dragsted, L.O.; Nielsen, C.S.; Stahl, W.; Rühl, R.; Borel, P. Host-related factors explaining interindividual variability of carotenoid bioavailability and tissue concentrations in humans. Mol. Nutr. Food Res. 2017, 61, 1600685.
- Deore, A.B.; Dhumane, J.R.; Wagh, R.; Sonawane, R. The stages of drug discovery and development process. Asian J. Pharm. Res. Dev. 2019, 7, 62–67.
- Trucillo, P. Drug carriers: Classification, administration, release profiles, and industrial approach. Processes 2021, 9, 470.
- Landersdorfer, C.B.; Gwee, A.; Nation, R.L. Clinical pharmacological considerations in an early intravenous to oral antibiotic switch: Are barriers real or simply perceived? Clin. Microbiol. Infec. 2023, 29, 1120–1125.
- Koziolek, M.; Alcaro, S.; Augustijns, P.; Basit, A.W.; Grimm, M.; Hens, B.; Corsetti, M. The mechanisms of pharmacokinetic food-drug interactions–A perspective from the UNGAP group. Eur. J. Pharm. Sci. 2019, 134, 31–59.
- Drenth-van Maanen, A.C.; Wilting, I.; Jansen, P.A. Prescribing medicines to older people—How to consider the impact of ageing on human organ and body functions. Brit. J. Clin. Pharmacol. 2020, 86, 1921–1930.
- Baillie, T.A.; Cayen, M.N.; Fouda, H.; Gerson, R.J.; Green, J.D.; Grossman, S.J.; Shipley, L.A. Drug metabolites in safety testing. Toxicol. Appl. Pharm. 2002, 182, 188–196.
- May, M.; Schindler, C.; Engeli, S. Modern pharmacological treatment of obese patients. Ther. Adv. Endocrinol. Metab. 2020, 11, 1–19.
