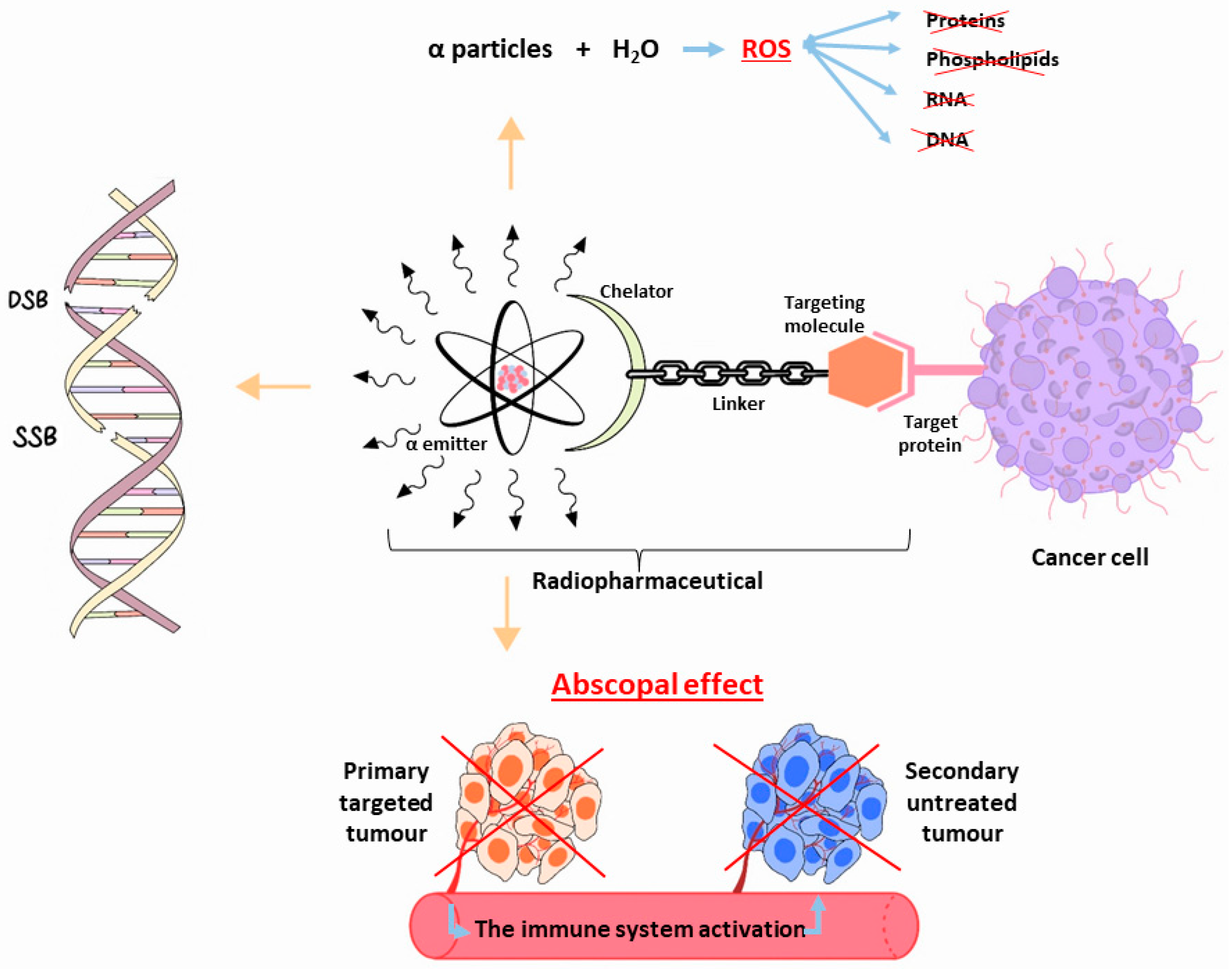
α radioisotopes can offer a treatment choice to individuals who are not responding to β− or gamma-radiation therapy or chemotherapy drugs. Only a few α-particle emitters are suitable for targeted alpha therapy (TAT) and clinical applications. The majority of available clinical research involves 225Ac and its daughter nuclide 213Bi. Additionally, the 225Ac disintegration cascade generates γ decays that can be used in single-photon emission computed tomography (SPECT) imaging, expanding the potential theranostic applications in nuclear medicine. Despite the growing interest in applying 225Ac, the restricted global accessibility of this radioisotope makes it difficult to conduct extensive clinical trials for many radiopharmaceutical candidates.
- targeted alpha therapy
- 225Ac
- physical properties
- production routes
- theranostic application
1. Introduction
2. 225Ac: Physical Characteristics
Actinium is a radioactive component with atomic number 89 [20]. Only two of its 32 isotopes, 228Ac and 227Ac, are naturally produced as a result of the disintegration of 232Th and 235U, respectively [20,21][20][21]. With its long half-life of 21.7 years and predominant β− emissions decay, 227Ac represents the most common actinium isotope. However, 228Ac, which is also a β− emitter, is highly uncommon [20,21][20][21]. 225Ac is the initial element in the actinide family, and its radioactive parents are parts of the now-extinct “neptunium series” [19,21][19][21]. This α-emitter isotope has a long half-life of 9.9 days [5,22][5][22]. Starting from 225Ac to reach 209Bi (T1/2 = 1.9 × 1019 y), the decay series includes six short-lived radionuclide daughters [5,23][5][23]. This radioactive cascade is represented by 221Fr (T1/2 = 4.8 min; 6.3 MeV α particle and 218 keV γ emission), 217At (T1/2 = 32.3 ms; 7.1 MeV α particle), 213Bi (T1/2 = 45.6 min; 5.9 MeV α particle, 492 keV β− particle and 440 keV γ emission), 213Po (T1/2 = 3.72 µs; 8.4 MeV α particle), 209Tl (T1/2 = 2.2 min; 178 keV β− particle), 209Pb (T1/2 = 3.23 h; 198 keV β− particle) [24] (Figure 2) [14].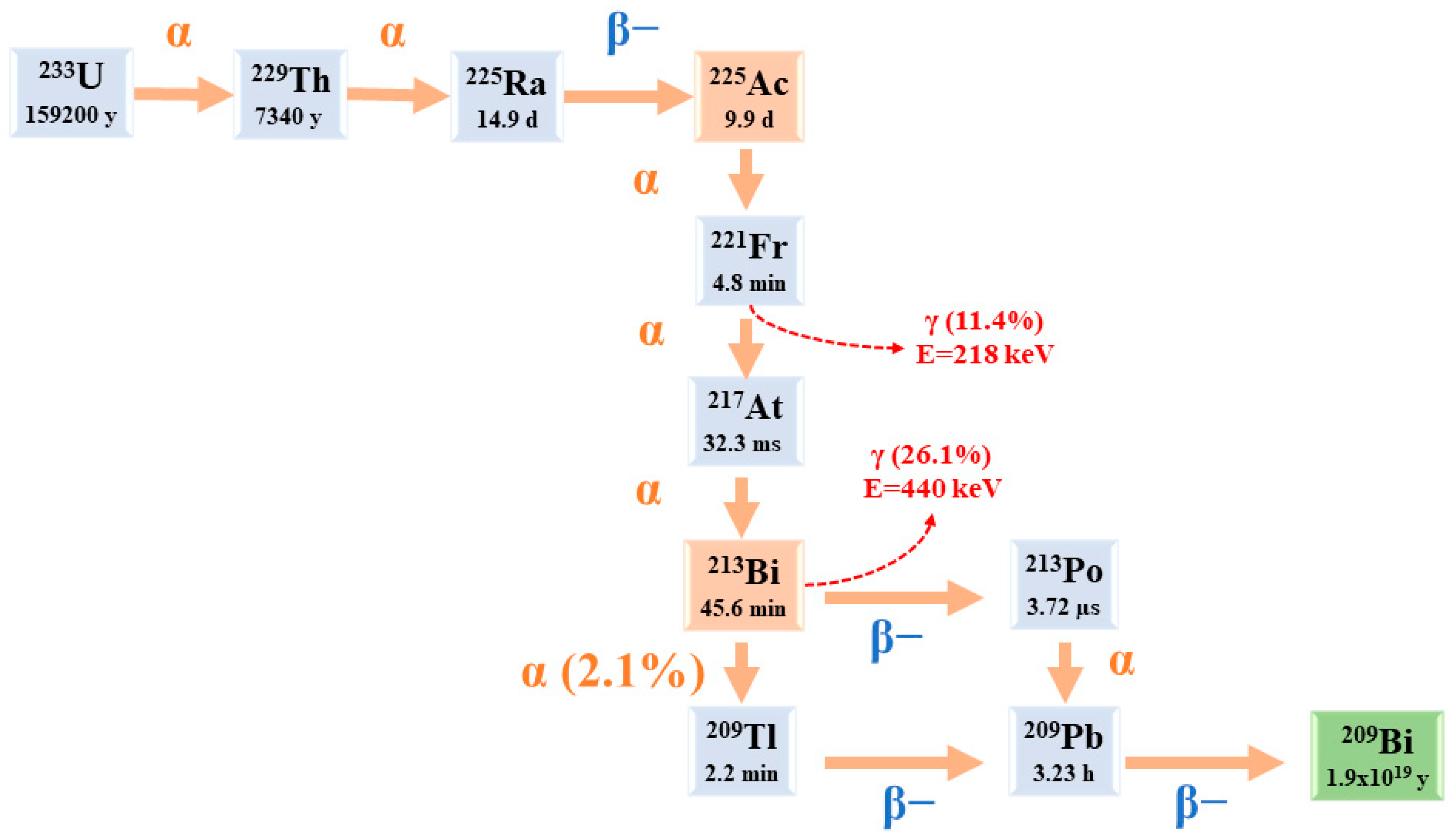
3. 225Ac and Its Potential Theranostic Use
225Ac is considered a “nanogenerator”, since one decay of this element produces a total of four α and three β particles, in addition to two γ emissions [24]. Taking into account its α particle emissions, along with the fact that the non-tumour binding activity can be eliminated before most of its dose is deposited in organs, 225Ac is considered an appealing choice for TAT [24,25][24][25]. However, it is important to give attention to the notable 225Ac cytotoxicity, including renal toxicity [26], due to its extended half-life and the various α particles produced throughout its decay chain [5]. A theranostic-based approach, characterised by the imaging–therapeutic duality, is the process of obtaining positron emission tomography (PET) and SPECT scans by exchanging the therapeutic α-emitting radionuclide with a positron or gamma diagnostic imaging radionuclide. Significant information on dosimetry and TAT reactions is obtained from these relevant nuclear medicine images. Chemical characteristics, half-life, radioactive emission type and intensity, related dosimetry, ease and scalability of production, radionuclidic purity, economics, and radionuclide progeny considerations are the factors that determine “the ideal” imaging surrogates for targeted alpha therapy [27,28][27][28]. Therapeutic use of 225Ac is often paired with imperfect PET imaging surrogates, such as 68Ga, 89Zr, or 111In, despite significant differences in their half-lives or chelation chemistry [29]. Studies are being conducted to address the limitations of imaging radionuclides by utilising lanthanum (La) as a potential alternative, especially 132La (T1/2 = 4.8 h, 42% β+) and 133La (T1/2 = 3.9 h, 7% β+) [30,31][30][31]. However, the half-lives of these isotopes are much shorter than that of 225Ac, limiting their applicability in PET imaging [29]. In this regard, the production of 134Ce (T1/2 = 3.2 d) has recently been started by the U.S. Department of Energy (DOE) Isotope Program [32]. The long 134Ce T1/2 and the similar chemical properties of 225Ac and 134Ce were considered potential benefits for monitoring in vivo pharmacokinetics. For PET imaging of the chelate and the antibody trastuzumab, 134Ce has been demonstrated to bind with diethylenetriamine pentaacetate (DTPA) [32] and dodecane tetraacetic acid (DOTA) [33]. On the other hand, greater molar ratios and higher temperatures are needed for isotope combinations with DOTA and DTPA [29]. In contrast, N, N′-bis[(6-carboxy-2-pyridyl)methyl]-4,13-diaza-18-crown-6 (macropa) has shown great stability for nonradioactive cerium and better chelate characteristics for 225Ac [34], indicating that it might be useful for the theranostic development of 134Ce/225Ac [35]. The potential use of γ disintegrations, obtained by the decay of the intermediate 221Fr (218 keV, 11.6% emission probability) and 213Bi (440 keV, 26.1% emission probability) [5], in SPECT in vivo imaging could lead the 225Ac radioactive cascade to a possible theranostic prospective in nuclear medicine applications. Nonetheless, planar SPECT imaging would be challenging because of the effectiveness of 225Ac, which results in modest administered doses (~50–200 kBq/kg [5]), along with low γ emissions [24,25][24][25]. As a possible solution to this limitation, we can notice the suitable use of 213Bi, which can be isolated from the 225Ac decay cascades [24]. Nevertheless, it is mandatory to consider the short half-life of 213Bi (45.6 min), which poses difficulties for processing, radiolabelling, and radiopharmaceutical delivery [24]. In addition, it is necessary to point out that these radiations make reaction monitoring complicated. Moreover, the secular equilibrium must be attained (for at least 6 h) before measuring a trustworthy radiochemical yield (RCY) [21]. Actinium’s chemistry lacks advancement because of its restricted availability; all Ac isotopes need specific management and facilities [20].4. Radiochemistry
During the production of radionuclides, it is mandatory to take into consideration a set of important aspects, such as safety, the co-generation of a few long-lived radionuclidic impurities, and adjustability, to enable delivery through clinical sites [27]. Once the target material has been irradiated, potent chemical purification methods are required to isolate the radioisotope [27,36,37,38][27][36][37][38]. Furthermore, the alpha particle may radiolytically damage the radiopharmaceutical itself, reducing in vivo targeting and producing more radioactive deposits in nontarget tissue. [27]. Since radiopharmaceuticals are considered typical pharmaceuticals, special manuals have been developed in the European Pharmacopoeia to deal with quality control issues [39]. Additionally, optimised protocols for preparing 225Ac agents in therapeutic doses have been established [40] (Table 1).|
Study |
Preparation Method |
Radiopharmaceutical |
RCY/RCP |
|---|---|---|---|
|
Abou. et al., 2022 [41] |
|
225Ac-DOTA-conjugated peptide |
>99%/>95% |
|
Dumond. et al., 2022 [42] |
|
225Ac-PSMA-617 |
>99%/98 ± 1% |
|
Thakral. et al., 2021 [43] |
|
225Ac-PSMA-617 |
85–87%/97–99% |
|
Kelly. et al., 2021 [44] |
|
225Ac-PSMA conjugated peptide/ 225Ac-DOTA conjugated peptide/ 225Ac-macropa conjugated peptide |
2.7 ± 0.55%–98.8 ± 0.09%/1.8–99.5% |
|
Hooijman. et al., 2021 [45] |
|
225Ac-PSMA-I&T |
>95%/>90% |
5. 225Ac Radiopharmaceuticals and Clinical Applications
The delivery of the radiopharmaceutical via the circulatory system enables the targeting of both the main tumour and its metastases. Whether a radiopharmaceutical is intended for therapeutic or diagnostic purposes depends on the decay properties of the linked radioisotope. For the purpose of curing, controlling, or palliating symptoms, TAT aims to provide an adequate amount of ionising radiation to intended malignities areas [27]. This means that any TAT agent must have a thorough understanding of its stability, pharmacokinetics, and dosimetry. Investigations on 225Ac have shown potential in treating neuroendocrine tumours, acute myeloid leukaemia, and metastatic prostate cancer, and more radiopharmaceuticals are being developed for other cancer types [46,47,48,49,50,51,52][46][47][48][49][50][51][52] (Table 2).|
Disease |
Study |
Radiopharmaceutical |
|---|---|---|
|
Prostate cancer |
Parida et al., 2023 [53] |
225Ac-PSMA RLT |
|
Ma et al., 2022 [54] |
225Ac-PSMA-617 |
|
|
Sanli et al., 2021 [55] |
225Ac-PSMA-617 |
|
|
Sen et al., 2021 [56] |
225Ac-PSMA-617 |
|
|
Zacherl et al., 2021 [50] |
225Ac-PSMA-I&T |
|
|
Feuerecker et al., 2021 [57] |
225Ac-PSMA-617 |
|
|
Van Der Doelen et al., 2021 [58] |
225Ac-PSMA-617 |
|
|
Sathekge et al., 2020 [51] |
225Ac-PSMA-617 |
|
|
Yadav et al., 2020 [59] |
225Ac-PSMA-617 |
|
|
Satapathy et al., 2020 [60] |
225Ac-PSMA-617 |
|
|
Sathekge et al., 2019 [61] |
225Ac-PSMA-617 |
|
|
Kratochwil et al., 2018 [62] |
225Ac-PSMA-617 |
|
|
Neuroendocrine tumours |
Ballal et al., 2022 [63] |
225Ac-DOTATATE |
|
Yadav et al., 2022 [48] |
225Ac-DOTATATE |
|
|
Kratochwil et al., 2021 [64] |
225Ac-DOTATATE |
|
|
Ballal et al., 2020 [65] |
225Ac-DOTATATE |
|
|
Kratochwil et al., 2015 [66] |
225Ac-DOTATOC |
|
|
Acute myeloid leukaemia |
Rosenblat et al., 2022 [67] |
225Ac-lintuzumab |
|
Jurcic, 2018 [68] |
225Ac-lintuzumab |
|
|
Jurcic et al., 2016 [69] |
225Ac-lintuzumab |
|
|
Jurcic et al., 2011 [70] |
225Ac-lintuzumab |
6. The Production Routes of 225Ac
As already mentioned, 225Ac is part of the 237Np disintegration family that has vanished in nature. This radioactive element could be artificially reproduced [21]. In addition to direct production paths, 225Ac is conveniently reachable at numerous points along the decay chain, in particular via 233U (T1/2 =159200 y, 100% α), 229Th (T1/2 = 7340 y, 100% α), and 225Ra (T1/2 = 14.9 d, 100% β−) [19]. 225Ac possesses many fewer nucleons than other actinide nuclei that are more stable to be employed as production targets, such as 232Th and 226Ra [19]. Thus, production methods should, with rare exceptions, rely on radioactive decay or greater energy bombardments. The available production routes of 225Ac and its parents are listed below (Figure 3) [14]: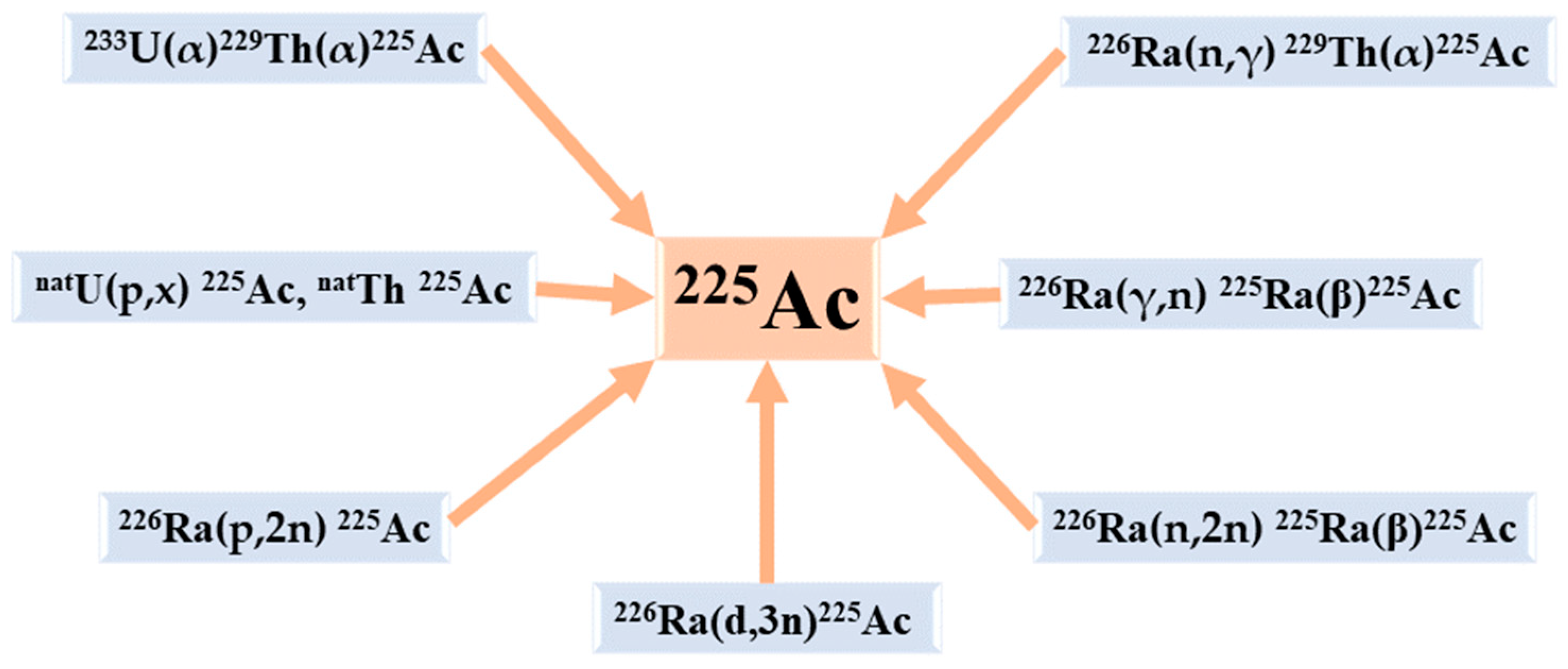
References
- McDevitt, M.R.; Sgouros, G.; Sofou, S. Targeted and Nontargeted α-Particle Therapies. Annu. Rev. Biomed. Eng. 2018, 20, 73–93.
- Parker, C.; Nilsson, S.; Heinrich, D.; Helle, S.I.; O’Sullivan, J.M.; Fosså, S.D.; Chodacki, A.; Wiechno, P.; Logue, J.; Seke, M.; et al. Alpha Emitter Radium-223 and Survival in Metastatic Prostate Cancer. N. Engl. J. Med. 2013, 369, 213–223.
- Jurcic, J.G.; Ravandi, F.; Pagel, J.M.; Park, J.H.; Smith, B.D.; Douer, D.; Estey, E.H.; Kantarjian, H.M.; Wahl, R.L.; Earle, D.; et al. Phase I Trial of Targeted Alpha-Particle Therapy Using Actinium-225 (225Ac)-Lintuzumab (Anti-CD33) in Combination with Low-Dose Cytarabine (LDAC) for Older Patients with Untreated Acute Myeloid Leukemia (AML). Blood 2014, 124, 5293.
- Johnson, J.D.; Heines, M.; Bruchertseifer, F.; Chevallay, E.; Cocolios, T.E.; Dockx, K.; Duchemin, C.; Heinitz, S.; Heinke, R.; Hurier, S.; et al. Resonant Laser Ionization and Mass Separation of 225Ac. Sci. Rep. 2023, 13, 1347.
- Morgenstern, A.; Apostolidis, C.; Kratochwil, C.; Sathekge, M.; Krolicki, L.; Bruchertseifer, F. An Overview of Targeted Alpha Therapy with 225Actinium and 213Bismuth. Curr. Radiopharm. 2018, 11, 200–208.
- Sgouros, G.; Roeske, J.C.; McDevitt, M.R.; Palm, S.; Allen, B.J.; Fisher, D.R.; Brill, A.B.; Song, H.; Howell, R.W.; Akabani, G.; et al. MIRD Pamphlet No. 22 (Abridged): Radiobiology and Dosimetry of Alpha-Particle Emitters for Targeted Radionuclide Therapy. J. Nucl. Med. 2010, 51, 311–328.
- Wulbrand, C.; Seidl, C.; Gaertner, F.C.; Bruchertseifer, F.; Morgenstern, A.; Essler, M.; Senekowitsch-Schmidtke, R. Alpha-Particle Emitting 213Bi-Anti-EGFR Immunoconjugates Eradicate Tumor Cells Independent of Oxygenation. PLoS ONE 2013, 8, e64730.
- Elgqvist, J.; Frost, S.; Pouget, J.-P.; Albertsson, P. The Potential and Hurdles of Targeted Alpha Therapy—Clinical Trials and Beyond. Front. Oncol. 2014, 3, 324.
- Friesen, C.; Glatting, G.; Koop, B.; Schwarz, K.; Morgenstern, A.; Apostolidis, C.; Debatin, K.-M.; Reske, S.N. Breaking Chemoresistance and Radioresistance with Anti-CD45 Antibodies in Leukemia Cells. Cancer Res. 2007, 67, 1950–1958.
- Kratochwil, C.; Giesel, F.L.; Bruchertseifer, F.; Mier, W.; Apostolidis, C.; Boll, R.; Murphy, K.; Haberkorn, U.; Morgenstern, A. 213Bi-DOTATOC Receptor-Targeted Alpha-Radionuclide Therapy Induces Remission in Neuroendocrine Tumours Refractory to Beta Radiation: A First-in-Human Experience. Eur. J. Nucl. Med. Mol. Imaging 2014, 41, 2106–2119.
- Kratochwil, C.; Bruchertseifer, F.; Giesel, F.L.; Weis, M.; Verburg, F.A.; Mottaghy, F.; Kopka, K.; Apostolidis, C.; Haberkorn, U.; Morgenstern, A. 225Ac-PSMA-617 for PSMA-Targeted α-Radiation Therapy of Metastatic Castration-Resistant Prostate Cancer. J. Nucl. Med. 2016, 57, 1941–1944.
- Humm, J.L.; Cobb, L.M. Nonuniformity of Tumor Dose in Radioimmunotherapy. J. Nucl. Med. 1990, 31, 75–83.
- Guerra Liberal, F.D.C.; O’Sullivan, J.M.; McMahon, S.J.; Prise, K.M. Targeted Alpha Therapy: Current Clinical Applications. Cancer Biother. Radiopharm. 2020, 35, 404–417.
- Ahenkorah, S.; Cassells, I.; Deroose, C.M.; Cardinaels, T.; Burgoyne, A.R.; Bormans, G.; Ooms, M.; Cleeren, F. Bismuth-213 for Targeted Radionuclide Therapy: From Atom to Bedside. Pharmaceutics 2021, 13, 599.
- Vermeulen, K.; Vandamme, M.; Bormans, G.; Cleeren, F. Design and Challenges of Radiopharmaceuticals. Semin. Nucl. Med. 2019, 49, 339–356.
- Beyls, C.; Haustermans, K.; Deroose, C.M.; Pans, S.; Vanbeckevoort, D.; Verslype, C.; Dekervel, J. Could Autoimmune Disease Contribute to the Abscopal Effect in Metastatic Hepatocellular Carcinoma? Hepatology 2020, 72, 1152–1154.
- Seidl, C. Radioimmunotherapy with α-Particle-Emitting Radionuclides. Immunotherapy 2014, 6, 431–458.
- Zimmermann, R. Is Actinium Really Happening? J. Nucl. Med. 2023, 64, 1516–1518.
- Engle, J.W. The Production of Ac-225. Curr. Radiopharm. 2018, 11, 173–179.
- Hatcher-Lamarre, J.L.; Sanders, V.A.; Rahman, M.; Cutler, C.S.; Francesconi, L.C. Alpha Emitting Nuclides for Targeted Therapy. Nucl. Med. Biol. 2021, 92, 228–240.
- Eychenne, R.; Chérel, M.; Haddad, F.; Guérard, F.; Gestin, J.-F. Overview of the Most Promising Radionuclides for Targeted Alpha Therapy: The “Hopeful Eight”. Pharmaceutics 2021, 13, 906.
- Pommé, S.; Marouli, M.; Suliman, G.; Dikmen, H.; Van Ammel, R.; Jobbágy, V.; Dirican, A.; Stroh, H.; Paepen, J.; Bruchertseifer, F.; et al. Measurement of the 225Ac Half-Life. Appl. Radiat. Isot. 2012, 70, 2608–2614.
- Suliman, G.; Pommé, S.; Marouli, M.; Van Ammel, R.; Stroh, H.; Jobbágy, V.; Paepen, J.; Dirican, A.; Bruchertseifer, F.; Apostolidis, C.; et al. Half-Lives of 221Fr, 217At, 213Bi, 213Po and 209Pb from the 225Ac Decay Series. Appl. Radiat. Isot. 2013, 77, 32–37.
- Nelson, B.J.B.; Andersson, J.D.; Wuest, F. Targeted Alpha Therapy: Progress in Radionuclide Production, Radiochemistry, and Applications. Pharmaceutics 2020, 13, 49.
- Scheinberg, D.A.; McDevitt, M.R. Actinium-225 in Targeted Alpha-Particle Therapeutic Applications. Curr. Radiopharm. 2011, 4, 306–320.
- Muslimov, A.R.; Antuganov, D.; Tarakanchikova, Y.V.; Karpov, T.E.; Zhukov, M.V.; Zyuzin, M.V.; Timin, A.S. An Investigation of Calcium Carbonate Core-Shell Particles for Incorporation of 225Ac and Sequester of Daughter Radionuclides: In Vitro and in Vivo Studies. J. Control Release 2021, 330, 726–737.
- Nelson, B.J.B.; Wilson, J.; Andersson, J.D.; Wuest, F. Theranostic Imaging Surrogates for Targeted Alpha Therapy: Progress in Production, Purification, and Applications. Pharmaceuticals 2023, 16, 1622.
- Saini, S.; Bartels, J.L.; Appiah, J.-P.K.; Rider, J.H.; Baumhover, N.; Schultz, M.K.; Lapi, S.E. Optimized Methods for the Production of High-Purity 203Pb Using Electroplated Thallium Targets. J. Nucl. Med. 2023, 64, 1791–1797.
- Bobba, K.N.; Bidkar, A.P.; Meher, N.; Fong, C.; Wadhwa, A.; Dhrona, S.; Sorlin, A.; Bidlingmaier, S.; Shuere, B.; He, J.; et al. Evaluation of 134Ce/134La as a PET Imaging Theranostic Pair for 225Ac α-Radiotherapeutics. J. Nucl. Med. 2023, 64, 1076–1082.
- Aluicio-Sarduy, E.; Barnhart, T.E.; Weichert, J.; Hernandez, R.; Engle, J.W. Cyclotron-Produced 132La as a PET Imaging Surrogate for Therapeutic 225Ac. J. Nucl. Med. 2021, 62, 1012–1015.
- Nelson, B.J.B.; Ferguson, S.; Wuest, M.; Wilson, J.; Duke, M.J.M.; Richter, S.; Soenke-Jans, H.; Andersson, J.D.; Juengling, F.; Wuest, F. First In Vivo and Phantom Imaging of Cyclotron-Produced 133La as a Theranostic Radionuclide for 225Ac and 135La. J. Nucl. Med. 2022, 63, 584–590.
- Bailey, T.A.; Mocko, V.; Shield, K.M.; An, D.D.; Akin, A.C.; Birnbaum, E.R.; Brugh, M.; Cooley, J.C.; Engle, J.W.; Fassbender, M.E.; et al. Developing the 134Ce and 134La Pair as Companion Positron Emission Tomography Diagnostic Isotopes for 225Ac and 227Th Radiotherapeutics. Nat. Chem. 2021, 13, 284–289.
- Bailey, T.A.; Wacker, J.N.; An, D.D.; Carter, K.P.; Davis, R.C.; Mocko, V.; Larrabee, J.; Shield, K.M.; Lam, M.N.; Booth, C.H.; et al. Evaluation of 134Ce as a PET Imaging Surrogate for Antibody Drug Conjugates Incorporating 225Ac. Nucl. Med. Biol. 2022, 110–111, 28–36.
- Hu, A.; Aluicio-Sarduy, E.; Brown, V.; MacMillan, S.N.; Becker, K.V.; Barnhart, T.E.; Radchenko, V.; Ramogida, C.F.; Engle, J.W.; Wilson, J.J. Py-Macrodipa: A Janus Chelator Capable of Binding Medicinally Relevant Rare-Earth Radiometals of Disparate Sizes. J. Am. Chem. Soc. 2021, 143, 10429–10440.
- Thiele, N.A.; Brown, V.; Kelly, J.M.; Amor-Coarasa, A.; Jermilova, U.; MacMillan, S.N.; Nikolopoulou, A.; Ponnala, S.; Ramogida, C.F.; Robertson, A.K.H.; et al. An Eighteen-Membered Macrocyclic Ligand for Actinium-225 Targeted Alpha Therapy. Angew. Chem. Int. Ed. Engl. 2017, 56, 14712–14717.
- Rizk, H.E.; Breky, M.M.E.; Attallah, M.F. Development of Purification of No-Carrier-Added 47Sc of Theranostic Interest: Selective Separation Study from the natTi(n,p) Process. Radiochim. Acta 2023, 111, 273–282.
- Mousa, A.M.; Abdel Aziz, O.A.; Al-Hagar, O.E.A.; Gizawy, M.A.; Allan, K.F.; Attallah, M.F. Biosynthetic New Composite Material Containing CuO Nanoparticles Produced by Aspergillus Terreus for 47Sc Separation of Cancer Theranostics Application from Irradiated Ca Target. Appl. Radiat. Isot. 2020, 166, 109389.
- Attallah, M.F.; Rizk, S.E.; Shady, S.A. Separation of 152+154Eu, 90Sr from Radioactive Waste Effluent Using Liquid–Liquid Extraction by Polyglycerol Phthalate. Nucl. Sci. Tech. 2018, 29, 84.
- Hooijman, E.L.; Ntihabose, C.M.; Reuvers, T.G.A.; Nonnekens, J.; Aalbersberg, E.A.; van de Merbel, J.R.J.P.; Huijmans, J.E.; Koolen, S.L.W.; Hendrikx, J.J.M.A.; de Blois, E. Radiolabeling and Quality Control of Therapeutic Radiopharmaceuticals: Optimization, Clinical Implementation and Comparison of Radio-TLC/HPLC Analysis, Demonstrated by Lu-PSMA. EJNMMI Radiopharm. Chem. 2022, 7, 29.
- Mdanda, S.; Ngema, L.M.; Mdlophane, A.; Sathekge, M.M.; Zeevaart, J.R. Recent Innovations and Nano-Delivery of Actinium-225: A Narrative Review. Pharmaceutics 2023, 15, 1719.
- Abou, D.S.; Zerkel, P.; Robben, J.; McLaughlin, M.; Hazlehurst, T.; Morse, D.; Wadas, T.J.; Pandya, D.N.; Oyama, R.; Gaehle, G.; et al. Radiopharmaceutical Quality Control Considerations for Accelerator-Produced Actinium Therapies. Cancer Biother. Radiopharm. 2022, 37, 355–363.
- Dumond, A.R.S.; Rodnick, M.E.; Piert, M.R.; Scott, P.J.H. Synthesis of 225Ac-PSMA-617 for Preclinical Use. Curr. Radiopharm. 2022, 15, 96–103.
- Thakral, P.; Simecek, J.; Marx, S.; Kumari, J.; Pant, V.; Sen, I.B. In-House Preparation and Quality Control of Ac-225 Prostate-Specific Membrane Antigen-617 for the Targeted Alpha Therapy of Castration-Resistant Prostate Carcinoma. Indian. J. Nucl. Med. 2021, 36, 114–119.
- Kelly, J.M.; Amor-Coarasa, A.; Sweeney, E.; Wilson, J.J.; Causey, P.W.; Babich, J.W. A Suitable Time Point for Quantifying the Radiochemical Purity of 225Ac-Labeled Radiopharmaceuticals. EJNMMI Radiopharm. Chem. 2021, 6, 38.
- Hooijman, E.L.; Chalashkan, Y.; Ling, S.W.; Kahyargil, F.F.; Segbers, M.; Bruchertseifer, F.; Morgenstern, A.; Seimbille, Y.; Koolen, S.L.W.; Brabander, T.; et al. Development of Ac-PSMA-I&T for Targeted Alpha Therapy According to GMP Guidelines for Treatment of mCRPC. Pharmaceutics 2021, 13, 715.
- Busslinger, S.D.; Tschan, V.J.; Richard, O.K.; Talip, Z.; Schibli, R.; Müller, C. Ac-SibuDAB for Targeted Alpha Therapy of Prostate Cancer: Preclinical Evaluation and Comparison with Ac-PSMA-617. Cancers 2022, 14, 5651.
- King, A.P.; Gutsche, N.T.; Raju, N.; Fayn, S.; Baidoo, K.E.; Bell, M.M.; Olkowski, C.S.; Swenson, R.E.; Lin, F.I.; Sadowski, S.M.; et al. 225Ac-MACROPATATE: A Novel α-Particle Peptide Receptor Radionuclide Therapy for Neuroendocrine Tumors. J. Nucl. Med. 2023, 64, 549–554.
- Yadav, M.P.; Ballal, S.; Sahoo, R.K.; Bal, C. Efficacy and Safety of 225Ac-DOTATATE Targeted Alpha Therapy in Metastatic Paragangliomas: A Pilot Study. Eur. J. Nucl. Med. Mol. Imaging 2022, 49, 1595–1606.
- Rathke, H.; Bruchertseifer, F.; Kratochwil, C.; Keller, H.; Giesel, F.L.; Apostolidis, C.; Haberkorn, U.; Morgenstern, A. First Patient Exceeding 5-Year Complete Remission after 225Ac-PSMA-TAT. Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 311–312.
- Zacherl, M.J.; Gildehaus, F.J.; Mittlmeier, L.; Böning, G.; Gosewisch, A.; Wenter, V.; Unterrainer, M.; Schmidt-Hegemann, N.; Belka, C.; Kretschmer, A.; et al. First Clinical Results for PSMA-Targeted α-Therapy Using 225Ac-PSMA-I&T in Advanced-mCRPC Patients. J. Nucl. Med. 2021, 62, 669–674.
- Sathekge, M.; Bruchertseifer, F.; Vorster, M.; Lawal, I.O.; Knoesen, O.; Mahapane, J.; Davis, C.; Reyneke, F.; Maes, A.; Kratochwil, C.; et al. Predictors of Overall and Disease-Free Survival in Metastatic Castration-Resistant Prostate Cancer Patients Receiving 225Ac-PSMA-617 Radioligand Therapy. J. Nucl. Med. 2020, 61, 62–69.
- Camacaro, J.F.; Dunckley, C.P.; Harman, S.E.; Fitzgerald, H.A.; Lakes, A.L.; Liao, Z.; Ludwig, R.C.; McBride, K.M.; Yalcintas Bethune, E.; Younes, A.; et al. Development of 225Ac Production from Low Isotopic Dilution 229Th. ACS Omega 2023, 8, 38822–38827.
- Parida, G.K.; Panda, R.A.; Bishnoi, K.; Agrawal, K. Efficacy and Safety of Actinium-225 Prostate-Specific Membrane Antigen Radioligand Therapy in Metastatic Prostate Cancer: A Systematic Review and Metanalysis. Med. Princ. Pract. 2023, 32, 178–191.
- Ma, J.; Li, L.; Liao, T.; Gong, W.; Zhang, C. Efficacy and Safety of 225Ac-PSMA-617-Targeted Alpha Therapy in Metastatic Castration-Resistant Prostate Cancer: A Systematic Review and Meta-Analysis. Front. Oncol. 2022, 12, 796657.
- Sanli, Y.; Kuyumcu, S.; Simsek, D.H.; Büyükkaya, F.; Civan, C.; Isik, E.G.; Ozkan, Z.G.; Basaran, M.; Sanli, O. 225Ac-Prostate-Specific Membrane Antigen Therapy for Castration-Resistant Prostate Cancer: A Single-Center Experience. Clin. Nucl. Med. 2021, 46, 943–951.
- Sen, I.; Thakral, P.; Tiwari, P.; Pant, V.; Das, S.S.; Manda, D.; Raina, V. Therapeutic Efficacy of 225Ac-PSMA-617 Targeted Alpha Therapy in Patients of Metastatic Castrate Resistant Prostate Cancer after Taxane-Based Chemotherapy. Ann. Nucl. Med. 2021, 35, 794–810.
- Feuerecker, B.; Tauber, R.; Knorr, K.; Heck, M.; Beheshti, A.; Seidl, C.; Bruchertseifer, F.; Pickhard, A.; Gafita, A.; Kratochwil, C.; et al. Activity and Adverse Events of Actinium-225-PSMA-617 in Advanced Metastatic Castration-Resistant Prostate Cancer After Failure of Lutetium-177-PSMA. Eur. Urol. 2021, 79, 343–350.
- Van der Doelen, M.J.; Mehra, N.; van Oort, I.M.; Looijen-Salamon, M.G.; Janssen, M.J.R.; Custers, J.A.E.; Slootbeek, P.H.J.; Kroeze, L.I.; Bruchertseifer, F.; Morgenstern, A.; et al. Clinical Outcomes and Molecular Profiling of Advanced Metastatic Castration-Resistant Prostate Cancer Patients Treated with 225Ac-PSMA-617 Targeted Alpha-Radiation Therapy. Urol. Oncol. 2021, 39, 729.e7–729.e16.
- Yadav, M.P.; Ballal, S.; Sahoo, R.K.; Tripathi, M.; Seth, A.; Bal, C. Efficacy and Safety of 225Ac-PSMA-617 Targeted Alpha Therapy in Metastatic Castration-Resistant Prostate Cancer Patients. Theranostics 2020, 10, 9364–9377.
- Satapathy, S.; Mittal, B.R.; Sood, A.; Das, C.K.; Singh, S.K.; Mavuduru, R.S.; Bora, G.S. Health-Related Quality-of-Life Outcomes with Actinium-225-Prostate-Specific Membrane Antigen-617 Therapy in Patients with Heavily Pretreated Metastatic Castration-Resistant Prostate Cancer. Indian. J. Nucl. Med. 2020, 35, 299–304.
- Sathekge, M.; Bruchertseifer, F.; Knoesen, O.; Reyneke, F.; Lawal, I.; Lengana, T.; Davis, C.; Mahapane, J.; Corbett, C.; Vorster, M.; et al. 225Ac-PSMA-617 in Chemotherapy-Naive Patients with Advanced Prostate Cancer: A Pilot Study. Eur. J. Nucl. Med. Mol. Imaging 2019, 46, 129–138.
- Kratochwil, C.; Bruchertseifer, F.; Rathke, H.; Hohenfellner, M.; Giesel, F.L.; Haberkorn, U.; Morgenstern, A. Targeted α-Therapy of Metastatic Castration-Resistant Prostate Cancer with 225Ac-PSMA-617: Swimmer-Plot Analysis Suggests Efficacy Regarding Duration of Tumor Control. J. Nucl. Med. 2018, 59, 795–802.
- Ballal, S.; Yadav, M.P.; Tripathi, M.; Sahoo, R.K.; Bal, C. Survival Outcomes in Metastatic Gastroenteropancreatic Neuroendocrine Tumor Patients Receiving Concomitant 225Ac-DOTATATE Targeted Alpha Therapy and Capecitabine: A Real-World Scenario Management Based Long-Term Outcome Study. J. Nucl. Med. 2022, 64, 211–218.
- Kratochwil, C.; Apostolidis, L.; Rathke, H.; Apostolidis, C.; Bicu, F.; Bruchertseifer, F.; Choyke, P.L.; Haberkorn, U.; Giesel, F.L.; Morgenstern, A. Dosing 225Ac-DOTATOC in Patients with Somatostatin-Receptor-Positive Solid Tumors: 5-Year Follow-up of Hematological and Renal Toxicity. Eur. J. Nucl. Med. Mol. Imaging 2021, 49, 54–63.
- Ballal, S.; Yadav, M.P.; Bal, C.; Sahoo, R.K.; Tripathi, M. Broadening Horizons with 225Ac-DOTATATE Targeted Alpha Therapy for Gastroenteropancreatic Neuroendocrine Tumour Patients Stable or Refractory to 177Lu-DOTATATE PRRT: First Clinical Experience on the Efficacy and Safety. Eur. J. Nucl. Med. Mol. Imaging 2020, 47, 934–946.
- Kratochwil, C.; Bruchertseifer, F.; Giesel, F.; Apostolidis, C.; Haberkorn, U.; Morgenstern, A. Ac-225-DOTATOC—An Empiric Dose Finding for Alpha Particle Emitter Based Radionuclide Therapy of Neuroendocrine Tumors. J. Nucl. Med. 2015, 56, 1232.
- Rosenblat, T.L.; McDevitt, M.R.; Carrasquillo, J.A.; Pandit-Taskar, N.; Frattini, M.G.; Maslak, P.G.; Park, J.H.; Douer, D.; Cicic, D.; Larson, S.M.; et al. Treatment of Patients with Acute Myeloid Leukemia with the Targeted Alpha-Particle Nanogenerator Actinium-225-Lintuzumab. Clin. Cancer Res. 2022, 28, 2030–2037.
- Jurcic, J.G. Clinical Studies with Bismuth-213 and Actinium-225 for Hematologic Malignancies. Curr. Radiopharm. 2018, 11, 192–199.
- Jurcic, J.G.; Levy, M.Y.; Park, J.H.; Ravandi, F.; Perl, A.E.; Pagel, J.M.; Smith, B.D.; Estey, E.H.; Kantarjian, H.; Cicic, D.; et al. Phase I Trial of Targeted Alpha-Particle Therapy with Actinium-225 (225Ac)-Lintuzumab and Low-Dose Cytarabine (LDAC) in Patients Age 60 or Older with Untreated Acute Myeloid Leukemia (AML). Blood 2016, 128, 4050.
- Jurcic, J.G.; Rosenblat, T.L.; McDevitt, M.R.; Pandit-Taskar, N.; Carrasquillo, J.A.; Chanel, S.M.; Zikaras, K.; Frattini, M.G.; Maslak, P.G.; Cicic, D.; et al. Phase I Trial of the Targeted Alpha-Particle Nano-Generator Actinium-225 (225Ac)-Lintuzumab (Anti-CD33; HuM195) in Acute Myeloid Leukemia (AML). Blood 2011, 118, 768.
- Pretze, M.; Kunkel, F.; Runge, R.; Freudenberg, R.; Braune, A.; Hartmann, H.; Schwarz, U.; Brogsitter, C.; Kotzerke, J. Ac-EAZY! Towards GMP-Compliant Module Syntheses of 225Ac-Labeled Peptides for Clinical Application. Pharmaceuticals 2021, 14, 652.
- Eryilmaz, K.; Kilbas, B. Fully-Automated Synthesis of 177Lu Labelled FAPI Derivatives on the Module Modular Lab-Eazy. EJNMMI Radiopharm. Chem. 2021, 6, 16.
