Portal hypertension is a complex medical condition characterized by elevated blood pressure in the portal venous system. The conventional diagnosis of such disease often involves invasive procedures such as liver biopsy, endoscopy, or imaging techniques with contrast agents, which can be uncomfortable for patients and carry inherent risks. Deep neural networks can serve as useful auxiliary diagnostic tools, aiding healthcare professionals in making timely and accurate decisions for patients suspected of having portal hypertension.
1. Introduction
Portal hypertension (PHT) is a condition often related to the evolution of chronic liver disease, and is characterized by an excessive increase in portal venous pressure. This involves an increase in the hepatic venous pressure gradient (HVPG) between the portal vein and the inferior vena cava above the nominal value of 1–5 mmHg
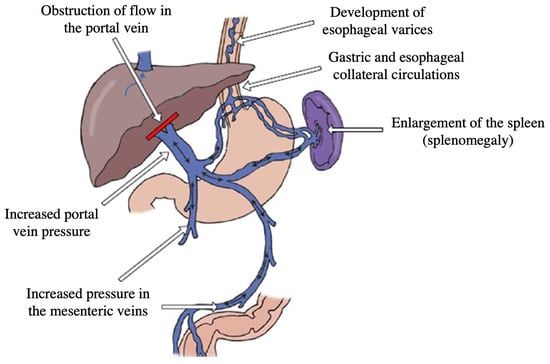
[1]. PHT involves the formation of collateral vessels that divert portal blood to the systemic circulation, bypassing the liver. This condition poses a significant clinical challenge and requires prompt diagnosis and management to prevent severe complications and improve patient outcomes.
There are numerous causes of portal hypertension, including cirrhosis, a chronic liver disease characterized by extensive fibrosis and nodular regeneration. Cirrhosis is the most common etiology, accounting for approximately 90%
of portal hypertension cases worldwide
[2]. Other causes include hepatic vein thrombosis, schistosomiasis, portal vein thrombosis, and congenital abnormalities
[3]. PHT gives rise to a multitude of complications that significantly impact patient health and quality of life. These complications include variceal bleeding, ascites, hepatic encephalopathy, hepatorenal syndrome, and spontaneous bacterial peritonitis
[4]. Variceal bleeding, resulting from the development of dilated and fragile veins in the esophagus or stomach, is one of the most severe complications and can be life-threatening if not promptly managed. The most common symptoms of PHT are shown in
Figure 1.
Figure 1.
Symptomatology of portal hypertension [5].
Given the critical nature of PHT and its associated complications, both prevention and early and accurate diagnosis are of the utmost importance. Traditionally, the diagnosis of PHT has relied on invasive procedures such as hepatic vein catheterization, which measures the HVPG, or imaging techniques like Doppler ultrasound and computed tomography (CT) scans
[6]. These methods provide valuable information about the extent and severity of portal hypertension, as well as associated liver abnormalities.
However, these traditional diagnostic approaches have limitations, including invasiveness, potential complications, and limited availability. Moreover, the interpretation of the obtained results requires specialized expertise. Hence, there is a need for alternative diagnostic methods that are non-invasive, readily accessible, and provide accurate and reliable results.
In recent years, there has been growing interest in the application of machine learning and artificial intelligence techniques, particularly deep neural networks, in the field of medical diagnostics. These techniques have shown promising results in various medical domains, including cancer detection, cardiovascular disease diagnosis, and neuroimaging analysis
[7][8][9][7,8,9]. In the context of PHT, the utilization of deep neural network classification models may offer a novel and valuable approach to improve diagnostic accuracy and aid in the timely management of this condition.
2. Artificial Intelligence in Hepatic Venous Pressure Gradient Diagnosis
In recent years, deep learning has emerged as a powerful paradigm within the field of artificial intelligence and machine learning
[10]. With its ability to automatically learn and extract intricate patterns from vast amounts of data, deep learning has revolutionized various domains, ranging from computer vision
[11] and natural language processing
[12] to speech recognition
[13] and robotics
[14]. This transformative approach has garnered significant attention and demonstrated remarkable success across diverse applications.
Deep learning, inspired by the structure and functioning of the human brain’s neural networks
[15], represents a subset of machine learning algorithms that learn multiple layers of representations or features from data
[16]. It leverages artificial neural networks composed of interconnected layers of artificial neurons, enabling the modeling of complex relationships and capturing intricate hierarchical patterns. This ability to automatically extract relevant features has led to breakthroughs in areas that were previously considered challenging or unsolvable.
One of the key strengths of deep learning lies in its ability to learn directly from raw data, eliminating the need for explicit feature engineering
[17]. This characteristic enables deep learning models to automatically discover relevant features and representations, effectively reducing the burden on human experts.
Artificial intelligence can be used to non-invasively diagnose HVPG through clinical tests such as abdominal ultrasound, computed tomography, magnetic resonance imaging, liver elastography, and the measurement of liver volume, increases in which correlate with disease severity. In particular, deep learning algorithms present the best performance in terms of quantifying HVPG non-invasively
[18]. In
[19], an auto-machine-learning model based on computed tomography achieves
80%accuracy in identifying severe PHT, implying useful support for early diagnosis and prophylaxis of the disease. In [20], a classification is performed that can discern between instances with HVPG values below 10 mmHg, and instances with HVPG values above 10 mmHg, using a set of deep learning methods on a dataset containing demographic, clinical, instrumental, and laboratory data. Specifically, the performance of four algorithms are compared: Naive Bayes, Regression, K-Nearest Neighbors, and Decision Trees. In [21], the segmentation of liver and spleen is performed to calculate their volume from the computed tomography of the volume of portal veins. Specifically, the deep learning algorithm automatically classifies the obtained segments as belonging to the liver, the spleen, or the background of the image, achieving 95% prediction accuracy. In [22] a machine learning approach was used to predict the HVPG, based on the histological features extracted from picrosirius-red-stained liver biopsies. The inclusion of the enhanced liver fibrosis score, platelet count, aspartate aminotransferase, and bilirubin significantly increased the diagnostic precision. However, this strategy was founded on information from an intrusive liver biopsy. In [23], neural networks were employed as a classification prediction model in a different prospective study on patients who underwent liver biopsy and HVPG measurement in order to identify those who had cirrhosis, CSPH, and esophageal varices. However, this method, which relied on a number of common blood indicators, did not surpass liver stiffness assessment as a stand-alone predictor.
A study (https://doi.org/10.3390/healthcare11182603) shows reasonable performance in distinguishing patients with PHT from healthy individuals. The model utilizes five clinical features (platelet count, total serum bilirubin, gamma-glutamyltransferase, activated partial thromboplastin time, and cholinesterase) to predict the hepatic venous pressure gradient (HVPG), which is used as a measure of PHT. The model’s performance suggests that deep neural networks can serve as useful auxiliary diagnostic tools in the non-invasive diagnosis of PHT, because of their ability to detect complex, multifaceted and non-linear relations within data by automatically learning hierarchical representations that capture intricate and abstract patterns.