Smart healthcare is altering the delivery of healthcare by combining the benefits of IoT, mobile, and cloud computing. Cloud computing has tremendously helped the health industry connect healthcare facilities, caregivers, and patients for information sharing. The main drivers for implementing effective healthcare systems are low latency and faster response times. Thus, quick responses among healthcare organizations are important in general, but in an emergency, significant latency at different stakeholders might result in disastrous situations. Thus, cutting-edge approaches like edge computing and artificial intelligence (AI) can deal with such problems. A packet cannot be sent from one location to another unless the “quality of service” (QoS) specifications are met.
- :quality of service
- smart healthcare
- Internet of Things (IoT)
1. Introduction
-
A patient in a remote area with few medical facilities can receive the care they need if the streaming videos between the doctor and patient work without any glitches. The doctor will be better able to evaluate the patient’s symptoms and make an accurate diagnosis.
-
Low latency is advantageous for X-rays, MRIs, and other medical imaging since it allows for speedy loading for the doctor and several viewing angles for quick interpretation of the delivered reports.
-
When a patient needs emergency care, it might be possible to save their life and guarantee that they receive the right care if a clinician has quick access to their medical records with no noticeable delays.
2. Smart Healthcare
Traditional healthcare cannot address all the needs of the population due to rapid population expansion. Hospital visits are challenging given the state of the planet, the most recent pandemic (COVID-19), the high expenditures, and the distances. To satisfy the demand for long-term care and remote medical monitoring, as well as to reduce the financial burden on patients by creating a digital healthcare system, it is essential to rely on technology that connects easily accessible medical resources and healthcare services. Smart healthcare is an IoT application that monitors, gathers, and analyzes medical data to provide online healthcare services. Smart healthcare could result in the development of a system of interconnected medical devices with sensors for the observation and treatment of patient health, as shown in Figure 1 [14][7]. Medical sensors are compact, sophisticated, reasonably priced, and light wearable sensor nodes used for health monitoring. They can be attached or connected to devices inside or outside the body. By effectively integrating these tiny devices with wireless technology, smart healthcare monitoring can be carried out using the Internet of Things [15][8]. By automatically interacting with them, these technologies alert users, physicians, and other healthcare providers, enabling them to deliver services effectively [16][9]. Given the growing trend towards smart cities, an effective smart healthcare system assures a healthy lifestyle for its citizens. Connectivity technologies are essential for developing smart healthcare applications. Smart healthcare apps are powered by cloud computing, machine learning protocols, and IoT. A patient record system that functions properly with the right sensing mechanisms and gathers structured and unstructured data for ML analysis is the technology and architecture of smart healthcare. Cloud computing makes it simple to access medical data from numerous sources, including test results and electronic medical records. Additionally, this framework offers analyses that allow medical professionals to compare how they perform to norms for high-quality treatment [17][10]. Smart healthcare integrates medical technology (sensors), the cloud, and humans (ML) to track, handle, and maintain patient records for continuing treatment and machine learning analysis.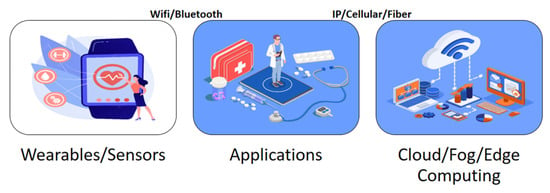
3. Internet of Things
In a presentation describing how RFID may be used for supply chain management, Ashton, K. [21][14] introduced the phrase “Internet of Things”. The phrase “Internet of Things” today is used to refer to a network of devices and gadgets—including various kinds of sensors and actuators, mobile phones, and wearable technologies—that communicate with one another over the Internet [22][15]. These devices establish connections with servers so that information can be retrieved and transmitted between them, successfully providing essential services. This ground-breaking technology can be seen as a paradigm change in patient health-focused low-cost healthcare applications. The Internet of Things connects patients and clinicians in a setting that incorporates sensors, sophisticated algorithms, cloud interfaces, and communication interfaces. Technology advancements in sensor, RFID, and WSN networks support data collection infrastructure as shown in Figure 2. Advanced algorithms are then used to analyze the data [23][16]. Cloud services can be utilized to upload medical data and lessen the complexity of the scenario due to the resource limitations of IoT devices. Healthcare applications cannot effectively use the delays provided by cloud computing due to low latency, great dependability, and other criteria for healthcare. With real-time analysis and efficient decision-making tools, healthcare applications are run anywhere near users to overcome these limitations. To overcome these restrictions, fog, and edge computing run healthcare apps close to IoT devices with real-time analysis and efficient decision-making tools [24][17]. Despite all its advancements, the IoT continues to be in its infancy. Numerous issues—such as the heterogeneity of various devices, scalability, security, and privacy—are still being researched.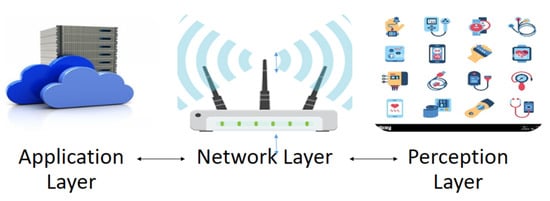
4. Cloud Computing
In cloud computing (CC) the provision of virtualized, on-demand computing, data storage, and networking capabilities via internet access via cloud services is completely customizable. The complexity and cost of CC resources vary depending on the desired capabilities and degree of application complexity for which they are used [26][19]. Compared to local computing resources, the cost, manageability, and flexibility of cloud computing resources have recently improved. Each data center in which cloud services are normally housed uses thousands of computers regularly. These systems must be able to scale up to extraordinarily high service demand levels while preserving reasonable processing times and low hardware and energy costs. This can enable interface simplicity that helps in processing widely accessible cloud data and offers a variety of services by linking multiple platforms. Infrastructure as a service (IaaS), platform as a service (PaaS), and software as a service are the three main services that make up CC services (SaaS). Companies may either buy or use CC services from cloud service providers, like Amazon, or they can build their own private clouds for their employees to use. Participatory community clouds are frequently used by research organizations and other pertinent organizations. In hybrid clouds, both private and public strategies are employed [27][20]. To assist better decision-making across a variety of application domains, including healthcare, applications enabled by CC solutions can extract highly important data. CC is one of the key enabling technologies for smart healthcare, which is made up of a variety of sensors, actuators, apps, and communication technologies, as shown in Figure 3.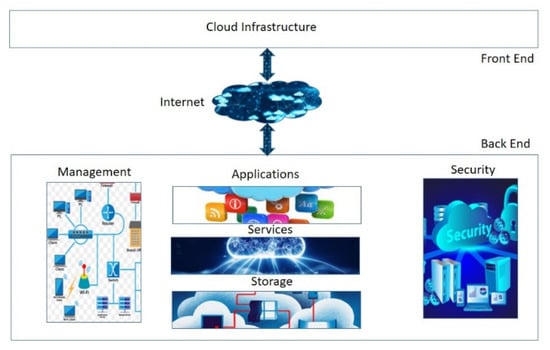
5. Fog/Edge Computing
Due to the numerous drawbacks of conventional centralized computing—such as single point failure, excessive latency, energy consumption, etc.—a more distributed and decentralized paradigm for cloud computing has emerged. Although CC does address several problems, such as single points of failure, it is still responsible for concerns with latency and energy use brought on by big uploads to the cloud servers. It became apparent that it would be best to upload only the data that required more processing to the cloud rather than the entire acquisition of data. It would be preferable to carry out operations that require lighter processing locally or very near to the user. Fog and edge computing are concepts that were inspired by this particular idea. This processing idea is shared by fog computing and edge computing. However, they differ technically as indicated by the Venn diagram in Figure 4.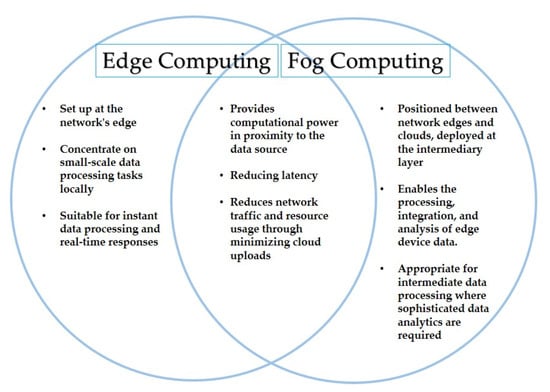
6. Machine Learning
Artificial intelligence, a new assistant for doctors, can help them with diagnostics and even prognoses. The ability to learn from experience can also make it easier to fully understand the conditions of the patients. The use of AI algorithms in SHAs allows for the creation of computer programs that acquire knowledge and grow as a result of experience rather than being explicitly programmed to make predictions or suggestions. Over the past few decades, technological advancements in computer power have made it possible for resource-intensive AI methods, like machine learning solutions, to be created. Machine learning programs use information for training, or data samples, to statistically develop a predictive model, as shown in Figure 5 [29][22]. Applications that are needed for sound decision-making employ this training to categorize things or make predictions. Smart healthcare applications use machine learning logic to process health data gathered from sensors and send it to the cloud for processing using machine learning algorithms. The received data are referred to as the testing data, and the outcomes are adequately emulated. After being emulated, the results will also be used for the training portion of the forthcoming testing data. The data obtained by the sensors are therefore viewed as testing data and, following processing, as training data for further medical assessments. Computational efficiency, detection precision, and robust implementation are the most important factors to consider when choosing machine learning algorithms for healthcare applications [30][23].
7. Quality of Service
Given how delicate the subject of health is, accuracy and perfection are paramount. Because health facilities cannot accept network performance difficulties or downtime caused by QoS solutions that were earlier suitable, providing QoS is a crucial obligation for smart healthcare apps. Since the information is so important to the patient’s health, the system needs to quickly gather reliable data. The QoS requirements must be met when a packet is sent from one place to another as shown in Figure 6. The throughput, bandwidth, transmission delay, availability, jitter, latency, and packet loss metrics are among them, as pointed out by Sodhro in [34][27]. They are defined as: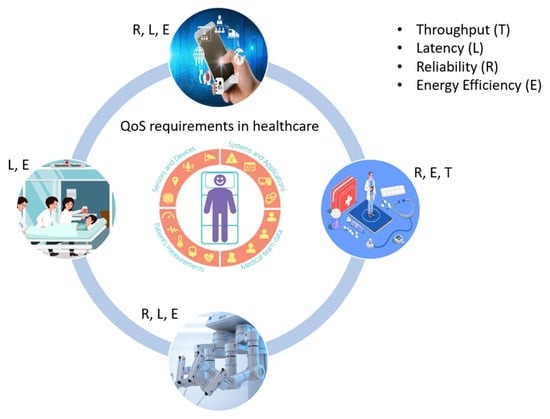
-
Throughput: within the time frame specified, data transmission traveled between two points.
-
Bandwidth: the optimum rate at which data can move through a network.
-
Delay: elapsed time for data traffic to reach its destination.
-
Availability: ratio of network’s accessibility to inaccessibility by its users.
-
Jitter: rate of change in data packets’ delays.
-
Latency: the sum of the time it takes a data packet to travel from its source to its destination plus any computational delays.
-
Packet loss: network issues preventing data packets from reaching their destinations.
References
- Abdellatif, A.A.; Mohamed, A.; Chiasserini, C.F.; Tlili, M.; Erbad, A. Edge computing for smart health: Context-aware approaches, opportunities, and challenges. IEEE Netw. 2019, 33, 196–203.
- Akmandor, A.O.; Jha, N.K. Smart Health Care: An Edge-Side Computing Perspective. IEEE Consum. Electron. Mag. 2018, 7, 29–37.
- Hayyolalam, V.; Aloqaily, M.; Özkasap, Ö.; Guizani, M. Edge Intelligence for Empowering IoT-Based Healthcare Systems. IEEE Wirel. Commun. 2021, 28, 6–14.
- Sodhro, A.H.; Luo, Z.; Sangaiah, A.K.; Baik, S.W. Mobile edge computing-based QoS optimization in medical healthcare applications. Int. J. Inf. Manag. 2019, 45, 308–318.
- Al-Rakhami, M.; Gumaei, A.; Alsahli, M.; Hassan, M.M.; Alamri, A.; Guerrieri, A.; Fortino, G. A lightweight and cost effective edge intelligence architecture based on containerization technology. World Wide Web 2020, 23, 1341–1360.
- Rahman, M.S.; Khalil, I.; Atiquzzaman, M.; Yi, X. Towards privacy preserving ai based composition framework in edge networks using fully homomorphic encryption. Eng. Appl. Artif. Intell. 2020, 94, 103737.
- Al-kahtani, M.S.; Khan, F.; Taekeun, W. Application of Internet of Things and Sensors in Healthcare. Sensors 2022, 22, 5738.
- Mohanty, S.P.; Choppali, U.; Kougianos, E. Everything you wanted to know about smart cities: The Internet of things is the backbone. IEEE Consum. Electron. Mag. 2016, 5, 60–70.
- Nayyar, A.; Puri, V.; Nguyen, N.G. BioSenHealth 1.0: A Novel Internet of Medical Things (IoMT)-Based Patient Health Monitoring System. In International Conference on Innovative Computing and Communications. Lecture Notes in Networks and Systems; Bhattacharyya, S., Hassanien, A., Gupta, D., Khanna, A., Pan, I., Eds.; Springer: Singapore, 2019; Volume 55.
- Darwish, A.; Hassanien, A.E.; Elhoseny, M.; Sangaiah, A.K.; Muhammad, K. The impact of the hybrid platform of internet of things and cloud computing on healthcare systems: Opportunities, challenges, and open problems. J. Ambient. Intell. Hum. Comput. 2019, 10, 4151–4166.
- Bhatti, D.S.; Saleem, S.; Imran, A.; Iqbal, Z.; Alzahrani, A.; Kim, H.; Kim, K.-I. A Survey on Wireless Wearable Body Area Networks: A Perspective of Technology and Economy. Sensors 2022, 22, 7722.
- Lins, S.; Pandl, K.D.; Teigeler, H. Artificial Intelligence as a Service. Bus. Inf. Syst. Eng. 2021, 63, 441–456.
- Huang, A. WE-CARE: An Intelligent Mobile Telecardiology System to Enable mHealth Applications. IEEE J. Biomed. Health Inform. 2014, 18, 693–702.
- Ashton, K. Internet of Things. RFiD J. 2009, 22, 97–114.
- Nikravan, M. An intelligent energy efficient QoS- routing scheme for WSN. Int. J. Adv. Eng. Sci. Technol. 2011, 8, 121–124.
- Wamba, S.F.; Anand, A.; Carter, L.D. A literature review of rfid-enabled healthcare applications and issues. Int. J. Inf. Manag. 2013, 33, 875–891.
- Al Masarweh, M.; Alwada’n, T.; Afandi, W. Fog Computing, Cloud Computing and IoT Environment: Advanced Broker Management System. J. Sens. Actuator Netw. 2022, 11, 84.
- Ray, P.P.; Dash, D.; De, D. Internet of things-based real-time model study on e-healthcare: Device, message service and dew computing. Comput. Netw. 2019, 149, 226–239.
- Sharma, H.K.; Kumar, A.; Pant, S.; Ram, M. 10 Cloud Commuting Platform for Smart Healthcare and Telemedicine. In Artificial Intelligence, Blockchain and IoT for Smart Healthcare; River Publishers: Gistrup, Denmark, 2022; pp. 95–104.
- Sarker, I.H. Machine Learning: Algorithms, Real-World Applications and Research Directions. SN Comput. Sci. 2021, 2, 160.
- Zhang, Y.; Qiu, M.; Tsai, C.-W.; Hassan, M.M.; Alamri, A. Health-CPS: Healthcare Cyber-Physical System Assisted by Cloud and Big Data. IEEE Syst. J. 2017, 11, 88–95.
- He, C.; Fan, X.; Li, Y. Toward Ubiquitous Healthcare Services with a Novel Efficient Cloud Platform. IEEE Trans. Biomed. Eng. 2013, 60, 230–234.
- Zahid, N.; Alkhayyat, A.; Ismail, M.; Sodhro, A.H. An Effective Traffic Management Approach for Decentralized BSNs. In Proceedings of the 2022 IEEE 96th Vehicular Technology Conference (VTC2022-Fall), London, UK, 26–29 September 2022; pp. 1–5.
- Jayatilak, S.M.D.A.C.; Ganegoda, G.U. Involvement of Machine Learning Tools in Healthcare Decision Making. J. Healthc. Eng. 2021, 2021, 6679512.
- Hutsebaut-Buysse, M.; Mets, K.; Latré, S. Hierarchical Reinforcement Learning: A Survey and Open Research Challenges. Mach. Learn. Knowl. Extr. 2022, 4, 172–221.
- Li, Y.; Huang, C.; Ding, L. Deep learning in bioinformatics: Introduction, application, and perspective in the big data era. Methods 2019, 166, 4–21.
- Thirunavukarasu, R.; Gnanasambandan, R.; Gopikrishnan, M.; Palanisamy, V. Towards computational solutions for precision medicine based big data healthcare system using deep learning models: A review. Comput. Biol. Med. 2022, 149, 106020.
