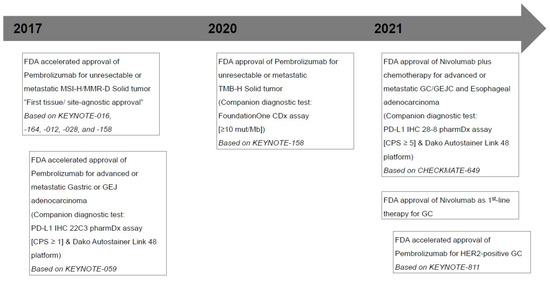
Despite advances in diagnostic imaging, surgical techniques, and systemic therapy, gastric cancer (GC) is the third leading cause of cancer-related death worldwide. Unfortunately, molecular heterogeneity and, consequently, acquired resistance in GC are the major causes of failure in the development of biomarker-guided targeted therapies. However, by showing promising survival benefits in some studies, the recent emergence of immunotherapy in GC has had a significant impact on treatment-selectable procedures. Immune checkpoint inhibitors (ICIs), widely indicated in the treatment of several malignancies, target inhibitory receptors on T lymphocytes, including the programmed cell death protein (PD-1)/programmed death-ligand 1 (PD-L1) axis and cytotoxic T-lymphocyte-associated protein 4 (CTLA4), and release effector T-cells from negative feedback signals.
- PD-L1
- gastric cancer
- immunotherapy
- biomarker
- IHC
- biopsy
1. Introduction
2. Rationale and Performance
3. Interpretation of PD-L1 IHC Assays in GC
To date, it has been typical to carry out IHC for evaluating PD-L1 expression [17]. When assessing PD-L1 expression, pathologists must pay attention to reproducibility and accuracy [17]. Criteria vary depending on the type of tumor. However, both the PD-L1 IHC 22C3 pharmDx and PD-L1 IHC 28-8 pharmDx assays share the CPS scoring system for assessing PD-L1 expression [2][18]. CPS is quantified as the number of PD-L1-stained cells (tumor cells, lymphocytes, and macrophages) and dividing the result by the total number of viable tumor cell subsequently multiplied by 100 [2][11][18]. For proper evaluation, at least 100 viable tumor cells must be present in the PD-L1-stained slide, and the maximum score is defined as 100 if the calculated results exceed 100 [2][11][18]. In CPS scoring system, partial linear or complete circumferential membrane staining (at any intensity) of invasive viable tumor cells is assessed, but not dysplasia or in situ carcinoma [2][11][18]. Conversely, membrane and/or cytoplasmic staining (at any intensity) of mononuclear inflammatory cells (including lymphocytes and macrophages) within tumor nests and adjacent supporting stroma is evaluated, but not eosinophils, neutrophils, and plasma cells. Additionally, normal cells, stromal cells (including fibroblasts), and cellular debris and/or necrotic cells are excluded from the numerator [18]. If the PD-L1 staining pattern shows heterogeneity, the final CPS should be determined by assessing the CPS results for each area within the entire tumor [18]. As previously mentioned, the interpretation of PD-L1 positivity should be according to the CPS cutoff point suitable for the assays used in the evaluation since two different PD-L1 assays have been approved as companion diagnostic assays on the basis of different CPS cutoff points [18]. CPS positivity is CPS ≥ 1 and CPS ≥ 5 in the PD-L1 IHC 22C3 pharmDx and PD-L1 and IHC 28-8 pharmDx assays, respectively [2][18]. In HER2-negative patients, the National Comprehensive Cancer Network Guidelines (NCCN) guidelines for GC version 2.2022 recommend fluoropyrimidine (fluorouracil or capecitabine), oxaliplatin, and nivolumab (CPS ≥ 5 when using the PD-L1 IHC 28-8 pharmDx assay) as preferred regimens of first-line therapy [14]. Another scoring method for PD-L1 IHC expression in other solid tumors, including metastatic non-small-cell lung cancer and melanoma, uses TPS for calculating the percentage of stained tumor cells out of the total tumor cells [2]. However, as TPS does not contain tumor-infiltrating immune cells when calculating the score, it may be inefficient in identifying responders [2][23]. Interestingly, a new tumor area positivity (TAP) score has recently been proposed for the evaluation of the VENTANA PD-L1 SP263 assay in G/GEJ adenocarcinoma and esophageal squamous cell carcinoma [24]. The TAP scoring system is measured as the percentages of the PD-L1-positive tumor cells plus immune cells are divided by the tumor area, which is occupied by all viable tumor cells and the tumor-associated stroma containing tumor-associated immune cells [24]. Partial linear or circumferential membrane staining (at any intensity) of tumor cells is evaluated, and cytoplasmic, membranous, and punctate staining of tumor-associated immune cells (at any intensity) is considered PD-L1-positive staining [24]. Liu et al. reported that the degree of agreement between the TAP (cutoff of 1%) and CPS (cutoff of 1%) was 100% positive percent agreement, 84.6% negative percent agreement, and 96.2% overall percent agreement [24]. Furthermore, they also suggested that the TAP scoring system is a simple, visual-based method as the average time spent on scoring is 5 min, and it can address the limitations of a cell-counting approach [24]. However, accumulating evidence based on clinical trials is required for the standardization of this scoring system.4. Interchangeability of PD-L1 Assays in GC
The interchangeability between the PD-L1 IHC 22C3 pharmDx and the PD-L1 IHC 28-8 pharmDx assays is very high [25][26]. Ahn et al. compared two PD-L1 assays in the same formalin-fixed, paraffin-embedded (FFPE) tissue blocks from 55 cases with GC and demonstrated that all PD-L1-positive cases using the PD-L1 IHC 22C3 pharmDx assay were also positive using the PD-L1 IHC 28-8 pharmDx assay, regardless of which CPS cutoff was used (≥1, ≥10, and ≥50) [25]. Moreover, they provided a high correlation between them in a comparison of the quantitative CPS of the two assays (Spearman correlation value = 0.978, p < 0.001) [25]. However, nonspecific background staining can be observed in the PD-L1 IHC 28-8 pharmDx assay. When the PD-L1 IHC 28-8 pharmDx assay was used in comparison with the PD-L1 IHC 22C3 pharmDx assay, nonspecific cytoplasmic staining, but not membranous staining, was observed in the muscular tissues and tumor cells [25]. Moreover, Narita et al. evaluated a pairwise comparison of two assays in the same FFPE tissue microarray (TMA) from 226 cases with GC. They reported that 87% of the pairs were concordant, and 11% had a higher expression using the PD-L1 IHC 22C3 pharmDx assay [26]. With a CPS of ≥ 5, the concordance between them was strong (kappa score = 0.881), specifically, 25 and 22 cases were positive using the PD-L1 IHC 22C3 pharmDx and PD-L1 IHC 28-8 pharmDx assays, respectively [26]. Conversely, Yeong et al. suggested that CPSs using the PD-L1 IHC 28-8 pharmDx assay were consistently observed at higher rates than that using the PD-L1 IHC 22C3 pharmDx assay in 362 cases with GC (344 cores of TMA, 18 whole slides) (70.3% versus 49.4%, p < 0.001 at CPS ≥ 1; 29.1% versus 13.4%, p < 0.001 at CPS ≥ 5; 13.7% versus 7.0%, p = 0.004 at CPS ≥ 10) [27]. However, in their study, PD-L1 expression was determined by multiplex IHC/immunofluorescence using the Opal Multiplex fIHC kit (Akoya Biosciences, CA, USA) [27]. Moreover, Kim et al. demonstrated that the concordance for the different IHC assays (VENTANA PD-L1 SP263, PD-L1 IHC 22C3 pharmDx on the Dako automated staining platform, and PD-L1 IHC 22C3 pharmDx on the Ventana platform) was very low across all cutoffs in the biopsy or resection specimens (biopsy, kappa coefficient [κ] = 0.17–0.453; resection, κ = 0.02–0.311) [28]. Therefore, based on the results of several studies, even when using the same sample, PD-L1 expression can be observed differently depending on the antibody, staining method, and platform/machine [25][26][27][28][29].5. Discordance between Biopsy and Resection Specimens and Inter-Observer Variation
As previously mentioned, as PD-L1 staining patterns may exhibit intratumoral heterogeneity, there may be discrepancies in PD-L1 CPS results between paired biopsy and resection specimens [28][29]. Kim et al. reported that the overall positive agreement for PD-L1 results, when the CPS cutoff was 1, in paired biopsy and resection samples from 99 cases with GC was 100% (VENTANA PD-L1 SP263; κ = 1.000), 86% (PD-L1 IHC 22C3 pharmDx on the Dako automated staining platform; κ = 0.693) and 93% (PD-L1 IHC 22C3 pharmDx on the Ventana platform; κ = 0.820), respectively [28]. Additionally, Heo et al. presented that cases with PD-L1 CPS ≥1 were observed in 32.1% (36 of 112) paired biopsy and 47.3% (53 of 112) resection samples as measured by digital image analysis using the PD-L1 IHC 22C3 pharmDx assay [29]. Interestingly, in their study, 41 (36.6%) discrepant cases between biopsy and resection were determined by digital image analyses (κ = 0.254, p = 0.0048), while 31 (27.7%) discrepant cases were determined by pathologists (κ = 0.432, p < 0.0001) [29]. Furthermore, Yamashita et al. showed that cases with PD-L1 CPS ≥ 1 observed in 46.6% (89 of 191) paired biopsy and 70.1% (135 of 191) resection samples using the E1L3N antibody for PD-L1 [30]. In their study, the accordance of cases with only a single biopsy tissue was significantly lower (48.8%) than that of cases with multiple biopsied tissues (68.9%) (p < 0.05) [30]. Therefore, owing to the high levels of intraumoral and intertumoral heterogeneity in GC, PD-L1 expression in paired biopsy and resection specimens of GC may show relatively low concordance. Considering the difference in interpretation between digital image analyses and pathologists, inter-observer variation may also exist. Multiple biopsies can be more helpful than a single biopsy for reducing discrepancies in PD-1 CPS results between biopsy and resection [30]. Notably, Schoemig-Markiefka et al. suggested that sampling and analysis of four or more biopsies with a total area of approximately 4.5 mm2 may obtain similar results to resection specimens [31]. To evaluate inter-observer variation, Park et al. compared the CPS results of 55 cores of TMA obtained from five pathologists [32]. The PD-L1 IHC 22C3 pahrmDx assay had a higher concordance among pathologists than the VENTANA PD-L1 SP263 assay (CPS ≥ 1, κ = 0.389 versus κ = 0.224; CPS ≥ 10, κ = 0.256 versus κ = 0.140) [32]. They suggested that continuous training for PD-L1 interpretation is significant as trained pathologists showed higher agreement between the two assays than untrained pathologists [32].References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249.
- Kim, M.; Na Seo, A. Molecular Pathology of Gastric Cancer. J. Gastric Cancer 2022, 22, 273–305.
- Gullo, I.; Carneiro, F.; Oliveira, C.; Almeida, G.M. Heterogeneity in Gastric Cancer: From Pure Morphology to Molecular Classifications. Pathobiology 2018, 85, 50–63.
- Fuchs, C.S.; Doi, T.; Jang, R.W.; Muro, K.; Satoh, T.; Machado, M.; Sun, W.; Jalal, S.I.; Shah, M.A.; Metges, J.-P.; et al. Safety and Efficacy of Pembrolizumab Monotherapy in Patients with Previously Treated Advanced Gastric and Gastroesophageal Junction Cancer: Phase 2 Clinical KEYNOTE-059 Trial. JAMA Oncol. 2018, 4, e180013.
- Shitara, K.; Özgüroğlu, M.; Bang, Y.-J.; Di Bartolomeo, M.; Mandalà, M.; Ryu, M.-H.; Fornaro, L.; Olesiński, T.; Caglevic, C.; Muro, K.; et al. Pembrolizumab versus paclitaxel for previously treated, advanced gastric or gastro-oesophageal junction cancer (KEYNOTE-061): A randomised, open-label, controlled, phase 3 trial. Lancet 2018, 392, 123–133.
- Shitara, K.; Van Cutsem, E.; Bang, Y.-J.; Fuchs, C.; Wyrwicz, L.; Lee, K.-W.; Kudaba, I.; Garrido, M.; Chung, H.C.; Lee, J.; et al. Efficacy and Safety of Pembrolizumab or Pembrolizumab Plus Chemotherapy vs Chemotherapy Alone for Patients with First-line, Advanced Gastric Cancer: The KEYNOTE-062 Phase 3 Randomized Clinical Trial. JAMA Oncol. 2020, 6, 1571–1580.
- Janjigian, Y.Y.; Shitara, K.; Moehler, M.; Garrido, M.; Salman, P.; Shen, L.; Wyrwicz, L.; Yamaguchi, K.; Skoczylas, T.; Bragagnoli, A.C.; et al. First-line nivolumab plus chemotherapy versus chemotherapy alone for advanced gastric, gastro-oesophageal junction, and oesophageal adenocarcinoma (CheckMate 649): A randomised, open-label, phase 3 trial. Lancet 2021, 398, 27–40.
- Janjigian, Y.Y.; Kawazoe, A.; Yañez, P.; Li, N.; Lonardi, S.; Kolesnik, O.; Barajas, O.; Bai, Y.; Shen, L.; Tang, Y.; et al. The KEYNOTE-811 trial of dual PD-1 and HER2 blockade in HER2-positive gastric cancer. Nature 2021, 600, 727–730.
- Dunn, G.P.; Bruce, A.T.; Ikeda, H.; Old, L.J.; Schreiber, R.D. Cancer immunoediting: From immunosurveillance to tumor escape. Nat. Immunol. 2002, 3, 991–998.
- Kim, H.; Chung, J.-H. PD-L1 Testing in Non-small Cell Lung Cancer: Past, Present, and Future. J. Pathol. Transl. Med. 2019, 53, 199–206.
- Kwak, Y.; Na Seo, A.; Lee, H.E.; Lee, H.S. Tumor immune response and immunotherapy in gastric cancer. J. Pathol. Transl. Med. 2020, 54, 20–33.
- Cho, Y.A.; Lee, H.; Kim, D.G.; Kim, H.; Ha, S.Y.; Choi, Y.-L.; Jang, K.-T.; Kim, K.-M. PD-L1 Expression Is Significantly Associated with Tumor Mutation Burden and Microsatellite Instability Score. Cancers 2021, 13, 4659.
- Kroeze, L.I.; de Voer, R.M.; Kamping, E.J.; von Rhein, D.; Jansen, E.A.; Hermsen, M.J.; Barberis, M.C.; Botling, J.; Garrido-Martin, E.M.; Haller, F.; et al. Evaluation of a Hybrid Capture–Based Pan-Cancer Panel for Analysis of Treatment Stratifying Oncogenic Aberrations and Processes. J. Mol. Diagn. 2020, 22, 757–769.
- Ajani, J.A.; D’amico, T.A.; Bentrem, D.J.; Chao, J.; Cooke, D.; Corvera, C.; Das, P.; Enzinger, P.C.; Enzler, T.; Fanta, P.; et al. Gastric Cancer, Version 2.2022, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2022, 20, 167–192.
- Ishida, Y.; Agata, Y.; Shibahara, K.; Honjo, T. Induced expression of PD-1, a novel member of the immunoglobulin gene superfamily, upon programmed cell death. EMBO J. 1992, 11, 3887–3895.
- Ribas, A. Tumor Immunotherapy Directed at PD-1. N. Engl. J. Med. 2012, 366, 2517–2519.
- Kim, B.; Kang, S.Y.; Kim, K.-M. DNA-protein biomarkers for immunotherapy in the era of precision oncology. J. Pathol. Transl. Med. 2021, 55, 26–32.
- Park, Y.S.; Kook, M.-C.; Kim, B.-H.; Lee, H.S.; Kang, D.-W.; Gu, M.-J.; Shin, O.R.; Choi, Y.; Lee, W.; Kim, H.; et al. A Standardized Pathology Report for Gastric Cancer: 2nd Edition. J. Gastric Cancer 2023, 23, 107–145.
- Garcia-Diaz, A.; Shin, D.S.; Moreno, B.H.; Saco, J.; Escuin-Ordinas, H.; Rodriguez, G.A.; Zaretsky, J.M.; Sun, L.; Hugo, W.; Wang, X.; et al. Interferon Receptor Signaling Pathways Regulating PD-L1 and PD-L2 Expression. Cell Rep. 2017, 19, 1189–1201.
- Zou, W.; Wolchok, J.D.; Chen, L. PD-L1 (B7-H1) and PD-1 pathway blockade for cancer therapy: Mechanisms, response biomarkers, and combinations. Sci. Transl. Med. 2016, 8, 328rv4.
- Brahmer, J.R.; Tykodi, S.S.; Chow, L.Q.M.; Hwu, W.-J.; Topalian, S.L.; Hwu, P.; Drake, C.G.; Camacho, L.H.; Kauh, J.; Odunsi, K.; et al. Safety and Activity of Anti-PD-L1 Antibody in Patients with Advanced Cancer. N. Engl. J. Med. 2012, 366, 2455–2465.
- Kang, Y.-K.; Chen, L.-T.; Ryu, M.-H.; Oh, D.-Y.; Oh, S.C.; Chung, H.C.; Lee, K.-W.; Omori, T.; Shitara, K.; Sakuramoto, S.; et al. Nivolumab plus chemotherapy versus placebo plus chemotherapy in patients with HER2-negative, untreated, unresectable advanced or recurrent gastric or gastro-oesophageal junction cancer (ATTRACTION-4): A randomised, multicentre, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2022, 23, 234–247.
- Akhtar, M.; Rashid, S.; Al-Bozom, I.A. PD–L1 immunostaining: What pathologists need to know. Diagn. Pathol. 2021, 16, 94.
- Liu, C.; Fang, F.; Kong, Y.; ElGabry, E.A. Tumor Area Positivity (TAP) score of programmed death-ligand 1 (PD-L1): A novel visual estimation method for combined tumor cell and immune cell scoring. Diagn. Pathol. 2023, 18, 48.
- Ahn, S.; Kim, K.-M. PD-L1 expression in gastric cancer: Interchangeability of 22C3 and 28-8 pharmDx assays for responses to immunotherapy. Mod. Pathol. 2021, 34, 1719–1727.
- Narita, Y.; Sasaki, E.; Masuishi, T.; Taniguchi, H.; Kadowaki, S.; Ito, S.; Yatabe, Y.; Muro, K. PD-L1 immunohistochemistry comparison of 22C3 and 28-8 assays for gastric cancer. J. Gastrointest. Oncol. 2021, 12, 2696–2705.
- Yeong, J.; Lum, H.Y.J.; Teo, C.B.; Tan, B.K.J.; Chan, Y.H.; Tay, R.Y.K.; Choo, J.R.-E.; Jeyasekharan, A.D.; Miow, Q.H.; Loo, L.-H.; et al. Choice of PD-L1 immunohistochemistry assay influences clinical eligibility for gastric cancer immunotherapy. Gastric Cancer 2022, 25, 741–750.
- Kim, S.-W.; Jeong, G.; Ryu, M.-H.; Park, Y.S. Comparison of PD-L1 immunohistochemical assays in advanced gastric adenocarcinomas using endoscopic biopsy and paired resected specimens. Pathology 2021, 53, 586–594.
- Heo, Y.J.; Kim, B.; Kim, H.; Kim, S.; Jang, M.S.; Kim, K.-M. PD-L1 expression in paired biopsies and surgical specimens in gastric adenocarcinoma: A digital image analysis study. Pathol. Res. Pract. 2021, 218, 153338.
- Yamashita, K.; Iwatsuki, M.; Harada, K.; Koga, Y.; Kiyozumi, Y.; Eto, K.; Hiyoshi, Y.; Ishimoto, T.; Iwagami, S.; Baba, Y.; et al. Can PD-L1 expression evaluated by biopsy sample accurately reflect its expression in the whole tumour in gastric cancer? Br. J. Cancer 2019, 121, 278–280.
- Schoemig-Markiefka, B.; Eschbach, J.; Scheel, A.H.; Pamuk, A.; Rueschoff, J.; Zander, T.; Buettner, R.; Schroeder, W.; Bruns, C.J.; Loeser, H.; et al. Optimized PD-L1 scoring of gastric cancer. Gastric Cancer 2021, 24, 1115–1122.
- Park, Y.; Koh, J.; Na, H.Y.; Kwak, Y.; Lee, K.-W.; Ahn, S.-H.; Park, D.J.; Kim, H.-H.; Lee, H.S. PD-L1 Testing in Gastric Cancer by the Combined Positive Score of the 22C3 PharmDx and SP263 Assay with Clinically Relevant Cut-offs. Cancer Res. Treat. 2020, 52, 661–670.
