Thyroid storm (TS) is a rare and fatal endocrine emergency that occurs due to undiagnosed and inadequately treated hyperthyroidism after stressful conditions in patients with thyroid disorders. This review explores the myocardial involvement in terms of injury, dysrhythmia, cardiomyopathy, failure, and cardiogenic shock (CS) during TS and the modalities of treatment and their efficiency, including pharmacological, mechanical, and surgical options are explored.
- thyroid storm
- thyrotoxic crisis
- hyperthyroidism
- myocardial disease
- shock
- mechanical support
- thyroidectomy
1. Introduction
2. Thyroid Storm Complicated with Myocardial Involvement and Shock
Precipitating factors: TS can be triggered by various factors; some may spark underlying thyroid dysfunction, and others exacerbate existing thyroid diseases, particularly Graves’ disease [16]. These precipitating factors include noncompliance with ATD, surgery (thyroid and non-thyroid), trauma, acute illness with infection, childbirth, hydatidiform mole, acute stress, drugs, and excess iodine intake [2,16,99,107,136,144][2][16][19][20][21][22]. As 99% of thyroid hormones are in a bound form, stressors may decrease the hormone-binding capacity and thus abruptly increase the concentration of the free hormones, leading to TS (2191). Even microtrauma in stable thyroid disorders, such as fine-needle aspiration (FNA), can cause TS [243][23].
Noncompliance with medications: Galindo et al. [6] reported non-compliance in 15.4% of TS cases in comparison with 6% in thyrotoxicosis without storm. Moreover, insurance and side effects of ATDs interfere with the continuity of therapy [31,36,167][24][25][26].
Drug-induced TS: A few cases of amiodarone-induced TS that led to cardiomyopathy and CS [37,43,173][27][28][29] were found. Amiodarone is a class III antiarrhythmic drug with iodine content used to treat tachyarrhythmia, in around 14–18% of patients; it may result in amiodarone-induced thyrotoxicosis (AIT) [244][30]. AIT can occur in up to 10% of patients [244][30]. The risk of developing AIT can be seen after 18 months to 3 years; even so, it may occur after withdrawal, as the drug can remain in the tissues for a prolonged time. There are two types of AIT; type 1 generally occurs in patients with clinical thyroid disease [174][31].
Acute illness and infection: The presence of infection can aggravate thyrotoxicosis in patients with TS, especially if unresolved or missed. Acute illnesses such as myocardial infarction, stroke, diabetic ketoacidosis (DKA), or hypoglycemia can lead to TS [31,46,104,126,133,165,169][24][32][33][34][35][36][37]. Das et al. [32][38] reported a case of TS with acute decompensated heart failure, possibly triggered by SARS-CoV-2 infection, in a 16-year-old female. This patient had pre-existing Graves’ disease and dilated cardiomyopathy; however, it was stable prior to COVID-19 infection. The overaction of the T helper cell response and elevation in interleukin-6 due to COVID-19 infection resulted in a change in thyroid gland functionality [32][38]. Prasankati et al. [105][39] described TS and COVID-19 in a patient without a history of heart or thyroid disease who presented with SVT.
Cardiac manifestations of TS: Thyroid hormone receptors are distributed in the myocardium and vascular tissue and can cause endothelial dysfunction and myocardial systolic and diastolic dysfunction [245][40]. The heart mainly relies on T3 hormones to regulate its activity because of the lack of significant intracellular ideiodinase activity in cardiomyocytes. This effect occurs through positive or negative regulation of the expression of key genes [246][41]. T3 exerts its effect on the heart via both genomic and non-genomic mechanisms and regulates cardiac function and cardiovascular hemodynamics through three main processes affecting hemodynamics (peripheral circulation), myocardial contractility, and heart rate. The presence of increased T3 levels would cause upregulation of positive cardiac gene expression and suppression of negative cardiac gene expression; positive gene expression includes upregulation of alpha-myosin heavy chain activity, sarcoplasmic reticulum Ca2+ ATPase and beta1-adrenergic receptors [246][41]. Hemodynamically, thyroid hormones decrease peripheral resistance in the arterioles through a direct effect on vascular smooth muscle cells and decrease mean arterial pressure. Such changes cause an increase in the heart rate and a decrease in the diastolic pressure. Vasodilation activates the renin–angiotensin–aldosterone system and increases Na+ absorption. In addition, T3 caused an increase in the red cell mass. All these changes lead to an increase in blood volume and preload and eventually cause an increase in cardiac output (ranging from 50 to 300% in patients with hyperthyroidism) [246][41]. Moreover, hypertension may occur because of the inability of the vascular system to accommodate the increase in stroke volume owing to a dramatic decrease in systemic vascular resistance (up to 70%) [246][41]. Tachyarrhythmia: Arrhythmias are frequently observed [167][26]. Sinus tachycardia is the most evident rhythm as it is a cardinal feature of TS [241,246][41][42]. Heart rate ≥ 150 bpm is associated with increased mortality in patients with TS [247][43]. A heart rate above 130 bpm has been reported in three-quarters of patients with thyrotoxic crisis [2]. However, AF is the most common arrhythmia in thyrotoxicosis, with a prevalence of 15%, and is typically of the persistent type rather than paroxysmal [179,248][44][45]. This was due to the pathological acceleration of diastolic depolarization of the sinoatrial node caused by the shortened action potential. Generally, thyroid hormones affect the cardiac conduction system, shorten the action potential, and increase the refractory duration of atrioventricular cells, thereby causing AF [246][41]. Moreover, overt sympathetic activity and an increase in thyroid hormone levels lead to excessive chronotropic and inotropic effects that contribute to tachyarrhythmia and myocardial ischemia [59][46]. Thyroid hormones augment beta-adrenergic receptor sensitivity to catecholamines and myocardial excitability. ECG findings such as atrial flutter, atrial tachycardia, ventricular tachycardia, and multifocal tachycardia have also been reported in TS. Waqar et al. reported that the proportions of AF, atrial flutter, VT, and SVT were 46%, 7%, 5%, and 1.5%, respectively [241][42]. In TS, AF is the most prevalent arrhythmia by 30–40% [111][47]. In a Japanese study, almost half of the TS patients who died had AF [3]. Evidently, there is a link between increased T4 serum level and AF incidence [248][45]. The incidence of AF has been linked to the increased sensitivity of myocytes to thyroid hormones as a result of high beta-adrenoreceptors on the surface of cardiac structures. This occurs because of the increased positive expression of beta-adrenoreceptor genes in response to increased T3 [245,246][40][41]. Rapid AF triggers hemodynamic collapse in the absence of an atrial kick, atrioventricular synchrony, and heart rate control [111][47]. Therefore, rapid AF is a precipitant of decompensated heart failure in TS [189][48]. Treatment of AF includes BBs, Class Ia and Ic antiarrhythmic agents, anticoagulation, digoxin, cardioversion (after exclusion of atrial thrombus), and amiodarone. TS-induced ventricular fibrillation (VF)/sudden cardiac death (SCD): A few cases of TS-induced SCD have been described in the literature [70,181,182,224][49][50][51][52]. The rate of death due to cardiac arrest increases significantly within a short timeframe in patients with TS, particularly in the presence of coexisting coronary artery disease [249][53]. Joa et al. [65][54] reported TS 6 months after discontinuation of antithyroid medication in a female patient. On arrival, the initial presentation was VT followed by VF. Circulatory collapse in TS is multifactorial and has been described after the administration of BBs, calcium channel blockers (CCBs), persistent arrhythmias (AF or VT), severe decompensated HF, CS, or severe coronary spasm. Moreover, severe respiratory distress may contribute to respiratory muscle asthenia, severe pulmonary hypertension, and respiratory failure [250][55]. Even in euthyroid patients, a study showed that higher levels of free T4 were associated with an increased risk of SCD, with a hazard ratio of 1.87 per 1 ng/dL increase in free T4 [250][55]. J-point elevation on ECG in TS: Although early repolarization (elevation of the QRS–ST junction (i.e., J-point elevation)) in at least two electrocardiographic leads is a common benign finding, it can be an arrhythmogenic substrate leading to VF [179][44]. J-point elevation represents a transmural voltage gradient between the endocardium and epicardium during ventricular electrical activation. In patients with TS, BBs may be an unsafe choice in the presence of early repolarization on ECG as it augments the elevation of the J-point and ST segment, increases the voltage gradient between the endocardium and epicardium, and enhances arrhythmogenicity. Ueno et al. [181][50] reported that a 69-year-old male presented with TS, and his ECG showed sinus rhythm with J-point elevation in the inferior and anterior leads. The patient was treated with landiolol (short-acting BB). During hospitalization, the patient developed AF followed by persistent VF, necessitating percutaneous cardiopulmonary support. Despite cardiac rhythm correction, the patient died a few days later due to multiorgan failure. Troponin release, Myocardial Injury, and Infarction (AMI): The actual incidence of AMI in patients with TS is not well known or is under-defined. Myocardial injury with or without ECG changes has been reported in most cases of TS and is defined as a cardiac troponin T concentration of 0.03 ng/mL or more or high-sensitivity troponin T concentration of 10 ng/L or more for women or 15 ng/L or more for men. AMI of either type I or II may occur in patients with thyrotoxicosis, with or without atherosclerosis, and most articles did not define the significance of elevated troponin levels in TS, especially when coronary angiography was not performed. Most patients with AMI are treated conservatively without thrombolytics or intervention because the majority has non-obstructive or non-atherosclerotic causes. In addition, multiorgan dysfunction and hemodynamic instability are limiting factors for aggressive treatment of AMI. Moreover, a slight increase in troponin levels in TS may be due to tachycardia, coronary artery spasm, or Takotsubo cardiomyopathy [241][42]. In a small sample size case series (n = 5), TS was initially misdiagnosed as AMI and CHF, which delayed on-time treatment of the storm [59][46]. TS-induced coronary spasm: Non-atherosclerotic causes of myocardial injury include an imbalance (mismatch) between oxygen supply and demand, which can occur with epicardial coronary artery spasm, tachyarrhythmias, or thyrotoxicosis. These factors can lead to type 2 acute MI [251][56]. Excess Thyroxine is associated with coronary spasms in young patients [252,253][57][58]. Omar et al. [96][59] described a 40-year-old male presented with an out-of-hospital cardiac arrest and AMI. Coronary angiography revealed spasm in the right coronary artery. The patient was successfully treated with intracoronary nitrate, BBs, CCBs, and intravenous fluids. Factors explaining excess thyroxine-induced coronary spasm include an increase in cellular calcium content, sympathetic activity, adrenergic receptor sensitivity, increased receptor numbers, hyper-reactivity of vascular smooth muscles, and coronary vasomotor tone abnormalities [181,251,253,254,255][50][56][58][60][61]. Acute Heart failure and cardiomyopathy: Heart failure may be the initial presentation of TS and the main cause of mortality [10]. High-output heart failure is often observed in patients with TS, owing to the overabundance of thyroid hormones. This type of heart failure includes cardiac output elevation compared with metabolic demand and a decrease in systemic vascular resistance mediated by the peripheral vasodilator adrenomedullin [10,162,177][10][62][63]. Consequently, it may progress to dilated cardiomyopathy and dysrhythmias [23][64]. Most patients have LVF or biventricular failure; however, isolated right-sided heart failure secondary to pulmonary artery hypertension can occur [256][65]. Dilated Cardiomyopathy (DCM): Dilated cardiomyopathy is characterized by progressive heart muscle disease and is the most common cardiomyopathy phenotype. Dilated thyrotoxic cardiomyopathy, an unusual TS phenotype, initially manifests in 6% of patients; however, severe LV dysfunction is observed in <1% of patients [1,30][1][66]. The presence of unregulated persistent tachycardia in patients with hyperthyroidism may precipitate DCM in 6–15% [53][67]. It is crucial to recognize DCM as a potentially reversible and unusual manifestation in patients with thyrotoxicosis patient [241][42]. Excess thyroxine centrally stimulates activity in the sympathetic nervous system by positively regulating β1-adrenergic receptors and upregulating sarcoplasmic reticulum Ca2+ ATPase, which is involved in excitation-contraction coupling and calcium-induced calcium release [257][68]. Calcium released from the ryanodine receptor in the sarcoplasmic reticulum activates the myocardial myofilaments, leading to positive inotropy [257][68]. Free T3 and T4 increase the expression of the more rapid contractile isoforms of the alpha-myosin heavy chain. In addition, these hormones stimulate erythropoietin secretion, contributing to increased blood volume, leading to high-output CHF. T3 leads to an increase in stroke volume and pulse rate and promotes peripheral vasodilation, causing a decrease in systemic vascular resistance, which in turn activates the renin–angiotensin system, leading to fluid and salt retention [30][66]. Notably, persistent tachycardia impairs myocardial contraction as the activity of the Na/K-ATPase pump declines, in addition to the downregulation of beta-adrenergic receptors [1]. These factors eventually lead to DCM during thyrotoxicosis. Pericardial effusion: There were seven cases of pericardial effusion and TS [33,41,106,163,193,205][69][70][71][72][73][74]. Pericardial effusion and pericarditis are rare in thyrotoxic diseases and may resolve without intervention after improvement of hyperthyroid status. Bui et al. reported pericardial effusions in 7 out of 12 patients with thyrotoxicosis due to Graves’ disease [259][75]. Circulatory collapse and Cardiogenic shock: CS is an infrequent complication of TS, with a high fatality rate [19][18]. In patients with impaired systolic function, CS has a mortality rate of up to 30% [167][26]. A Japanese study showed that the presence of shock increases the likelihood of mortality four-fold [3]. However, information regarding CS in TS is limited. Some factors are associated with the occurrence of thyrotoxic-induced CS, such as pre-existing CHF, valvular heart disease, AF, coagulopathy, and hepatic, renal, and pulmonary dysfunction [41][70]. Risk factor identification is crucial because these patients would require more intensive care and caution [41][70]. Additionally, drugs that may precipitate CS as BBs and CCBs must be discontinued to avoid further deterioration. Modalities of treatment of TS with myocardial involvement A multidisciplinary approach must be applied to patients with TS, because multiple organs are affected. It is crucial to adequately evaluate and avoid misdiagnosis of TS as early management plays a crucial role in the outcome. Pharmacological treatment Initial Management: 90% of patients were administered ATDs once diagnosed with TS. This classic regimen includes thioamides such as carbimazole (CBZ), methimazole (MMI) and propylthiouracil (PTU). They act by inhibiting thyroid peroxidase (TPO), thereby blocking the synthesis of T3 and T4 from thyroglobulin [17][76]. MMI and CBZ have higher potency than PTU. CBZ/MMI has a longer half-life and prolonged time of action; therefore, it may be administered as one dose daily rather than several times daily. However, PTU tends to be more effective in the treatment of TS as it also blocks the conversion of peripheral deiodinase-mediated T4 to T3 [17][76]. Table 1 shows the strength of the recommendation and quality of evidence for the measures of TS treatment [247][43]. In Graves’ disease, ATDs should be initiated as soon as possible, and adherence to treatment is vital. Large doses of inorganic iodide, simultaneously with ATDs, should be administered to treat Graves’ disease complicated with TS.| Measures of Treatment | Strength of Recommendation | Quality of Evidence |
|---|---|---|
| Antithyroid drugs (ATDs) | High | Low |
| Inorganic iodide | High | Moderate |
| Corticosteroids | High | Moderate |
| Cooling with acetaminophen and mechanical cooling | High | Low |
| Therapeutic plasmapheresis | Weak | Low |
| Central nervous system manifestations treatment | Strong | Low |
| Tachycardia treatment | High | Low |
| Atrial fibrillation treatment | High | Low |
| Acute congestive heart failure | High | Low |
| Treatment Modalities | N of Cases | Doses | Mechanism of Action/Indications | Side Effects and Contraindications |
|---|---|---|---|---|
| Anti-thyroid drugs (ATD) Carbimazole (CBZ) Methimazole (MMI) Propylthiouracil (PTU) |
228 | - MMI and CBZ oral 20–30 mg/day every 6–4 h. - PTU: 200 mg every 4 h. |
First line of treatment to control TS.
|
Agranulocytosis.
Rash. Thrombocytopenia (CBZ may be switched to PTU). Antineutrophilic cytoplasmic antibody vasculitis (PTU). Antithyroid arthritis syndrome (CBZ/MMI). |
| Inorganic iodide Saturated solution of Potassium iodide (SSKI) Lugol iodine |
111 | SKKI: 200 mg/day. Lugol Iodine: 5–10 drops orally once in 6–8 h. |
Wolff–Chaikoff effect
- Decreases blood flow to thyroid gland and so can be given prior to thyroidectomy. |
Hyperkalemia (potassium iodide). Due to the transient action:
|
| Cholestyramine | 33 | A total of 4 g oral intake 2–4 times a day. | - Elimination of thyroid hormone in enterohepatic circulation by binding to iodothyronines. - Indications:
|
|
| Corticosteroids Hydrocortisone/Dexamethasone prednisone |
172 | -IV/IM hydrocortisone: 150. mg/day every 6 h. -IV dexamethasone; 2 mg every 6 h. |
- When given in high doses, it inhibits thyroid hormone release, T4 and T3 conversion inhibition, and prevents adrenal insufficiency related to the hypermetabolic state of TS. - Increases vasomotor stability. - Given until TS resolves. |
|
| Beta Blockers Propranolol (NCBB) Metoprolol Esmolol (SC) Bisoprolol Landiolol (USC) Sotalol |
191 | -Propranolol: 1. oral or NGT 60–80 mg, 2. IV: 0.5–1 mg over 10 min followed by 1–2 mg over 10 every few hours. -Short-acting (Esmolol): a loading dose of 250–500 mcg/kg, followed by 50–100 mcg/kg infusion. |
|
Cardiogenic shock
Circulatory collapse. Hypotension. Refractory hypotension - Bronchoconstriction with bisoprolol. |
| Calcium channel blockers Verapamil Diltiazem |
30 | IV diltiazem push: 20 mg. | - Inhibit Ca2+ into excitable cells, resulting in smooth muscle dilation. - Negative inotropes in cardiac cells. - Indications:
- Was given for AF prior to TS diagnosis then discontinued when diagnosis made. |
- Cardiogenic shock. - Asystole. |
| Digoxin | 25 | IV: 0.125–0.25 mg. | Increases cardiac contractility as it binds and inhibits the Na/K-ATPase pump within cardiac myocytes. Positive inotropic effect:
|
Avoid in case of renal dysfunction as it increases renal clearance. - Worsening hypotension. |
| Inotropes (Vasopressors) Dopamine Dobutamine Epinephrine Levosimendan Noraderanline Milrinone |
81 | Dobutamine: infusion 2 (ug/kg/min) Noradrenaline. |
Dobutamine/dopamine: Inotrope with high affinity to B1 adrenergic receptors.
Milrinone:
|
|
| Amiodarone | 19 | IV: 125 mg over 10 min followed by a 0.8 mg infusion for 6 h. | - An iodine-rich class III antiarrhythmic - Blocks 5′mono-deiodination of t4 in peripheral tissues as the liver and pituitary gland.
- Most common antiarrhythmic in ICU due to stable properties.
|
- Hyperthyroid activity and thyrotoxic precipitant (Jod- Basedow phenomenon). - Amiodarone-induced thyrotoxicosis. - Hepatotoxicity; worsened ischemic hepatic failure. - Worsening hypotension |
Beta-blocker associated with circulatory collapse: BBs therapy has been described as a double-edged sword in TS [161][77]. Patients with prior clinical thyrotoxic cardiomyopathy or subclinical disease, especially in a setting of low-output heart failure, are prone to circulatory collapse when administered propranolol [175,177][63][78]. This may be attributed to NCBBs averting the compensatory hyperadrenergic state caused by thyrotoxicosis, and thus, a sharp decrease in the cardiac output in events as a TS leads to circulatory collapse [175][78]. Approximately 25.8% of cases reported hemodynamic instability and circulatory collapse, possibly due to BBs. In these cases, some were administered concomitantly with BBs and CCBs. Both agents are known to have negative inotropic effects [40][79]. Propranolol was the BB used in 46% of cases. Patients administered propranolol or atenolol tend to require extensive resuscitation [52][80]. Evidently, in conditions with signs of heart failure and low ejection fraction during thyrotoxic crisis, other agents are recommended [10,20,46,47][10][32][81][82]. Such agents are cardioselective BBs with shorting-acting properties, such as landiolol and esmolol, because titration and cessation are attainable [10,26,51,52][10][80][83][84]. Moreover, Voll et al. highlighted that even when dobutamine was administered during circulatory collapse alongside a high dose of propranolol, it was deemed less effective [36][25].
Calcium channel blockers (CCBs): Few authors have reported the use of CCB for the treatment of TS. However, Saakan et al. attributed diltiazem to the reversible CS in the setting of TS, as CCBs are atrioventricular blocker agents, leading to worsening of cardiac output and hemodynamic instability in a few cases [15]. Ivabradine: Hyperpolarization-activated cyclic nucleotide-gated (HCN) channel blockers, such as Ivabradine, act by selectively and specifically inhibiting the cardiac pacemaker current (If) of the sinoatrial node and do not affect contractility. Frenkel et al. described a 37-year-old patient with thyrotoxicosis and CHF [62][85]. In attempts to regulate the heart rate using propranolol at high doses, it was deemed ineffective. The patient was prescribed Ivabradine, a, and within 48 h, the heart rate was well controlled [62][85]. Amiodarone: It can be used in patients with TS for the treatment of tachyarrhythmia such as AF, flutter, and paroxysmal tachycardias [244][30]. Owing to its iodine content, it leads to thyroid dysfunction, as it Although amiodarone can cause AIT, Yamamoto et al. reported a patient with an initial diagnosis of multifocal atrial tachycardia complicated by CS [1]. Owing to unresolved refractory tachyarrhythmia, the decision was made to insert an IABP and continuous amiodarone infusion [1]. As the patient’s condition improved, it was later found in blood samples taken from the first (pre-amiodarone) to the seventh day that the patient had TS [1]. Non-pharmacological therapy Mechanical treatment of TS: The three main extracorporeal support systems (ECMO, TPE, and CRRT) can be useful as bridges for stability and definitive surgery in TS. Both ECMO and TPE were used concurrently in multiple cases, and only a few cases utilized all three. Evidence for the use of these systems arises from case reports or a few case series, as there are no prospective clinical trials. The use of these systems is costly and does not have side effects. Therefore, they require an expert team and appropriate patient selection and timing.- (a)
-
Extracorporeal Membrane Oxygenation (VA-ECMO): In 2021, Lim et al. [161][77] reported that there were 27 cases in the literature at the time of thyrotoxic crisis requiring ECMO, and 85% of these patients survived. In severe cases, first-line pharmacotherapy may not be sufficient to restore cardiovascular function to normal levels after TS development. When faced with this, extracorporeal modalities are implemented. Among the 256 cases, the use of ECMO was reported in 16.3% of cases; hence, it was the most used mechanical support. ECMO bypasses the heart and lungs and provides gas exchange through the external membrane [161][77]. This process supports the heart by temporarily relieving the heart of its functions to allow it to heal, while thyroid hormones normalize, and the euthyroid state is restored [263][86].
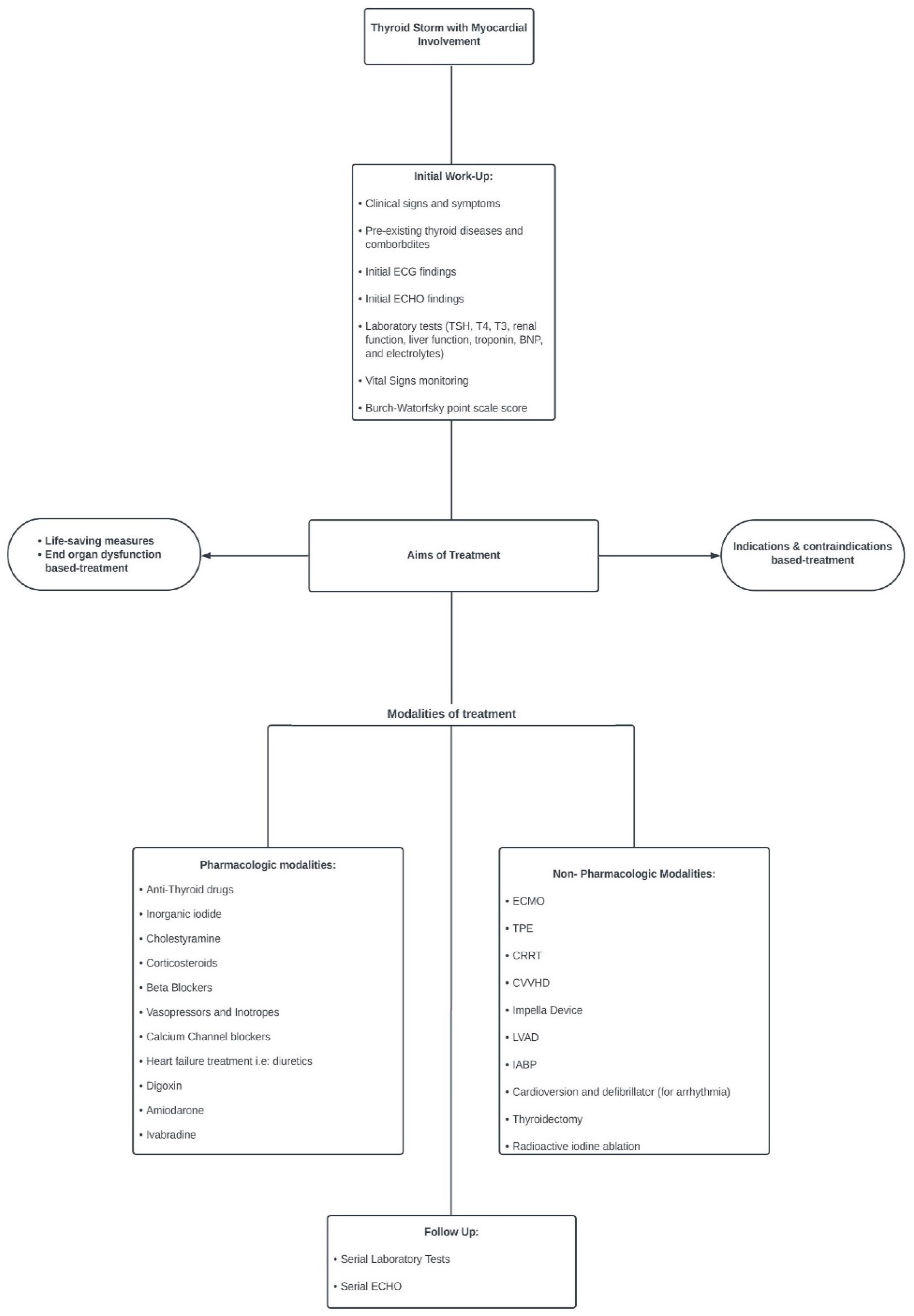 Figure 1.Algorithm for management of thyroid storm with cardiac involvement.
Figure 1.Algorithm for management of thyroid storm with cardiac involvement.3. Conclusions
The exact mechanism underlying the development of TS in uncomplicated thyrotoxicosis is not yet well defined; however, most manifestations of the latter occur in an exaggerated and wider manner during the storm. This could be due to the abrupt increase and availability of free thyroid hormones in the circulation, in addition to the enhanced response of the tissue receptors (which increase in number) to the hormone and catecholamine surge. Therefore, early and appropriate treatment of severe thyrotoxicosis is crucial to prevent the progression to TS and its higher fatalities. Frontline physicians should be aware of “TS” and not only “thyrotoxicosis” and the on-time appropriate treatment. The index of suspicion should be high, especially in the absence of a prior history of hyperthyroidism or clear triggers, as it may be missed in 30% of cases. Management should be guided by the affected end organ, indication versus contraindication (safety) of certain therapies, and the prevention of recurrence. The early diagnosis and management of TS in cardiac settings, including pharmacological, mechanical, and surgical modalities, may save high-risk patients. Mechanical support is required to bridge the gap between stability and definitive treatment. Sex matters in the presentation, treatment, and mortality of these populations, to a certain extent. However, further large-scale and well-designed studies are required.
References
- Yamamoto, H.; Monno, S.; Ohta-Ogo, K.; Ishibashi-Ueda, H.; Hashimoto, T. Delayed diagnosis of dilated thyrotoxic cardiomyopathy with coexistent multifocal atrial tachycardia: A case report. BMC Cardiovasc. Disord. 2021, 21, 124.
- Chiha, M.; Samarasinghe, S.; Kabaker, A.S. Thyroid storm: An updated review. J. Intensive Care Med. 2015, 30, 131–140.
- Akamizu, T.; Satoh, T.; Isozaki, O.; Suzuki, A.; Wakino, S.; Iburi, T.; Tsuboi, K.; Monden, T.; Kouki, T.; Otani, H.; et al. Diagnostic criteria, clinical features, and incidence of thyroid storm based on nationwide surveys. Thyroid 2012, 22, 661–679.
- Nayak, B.; Burman, K. Thyrotoxicosis and thyroid storm. Endocrinol. Metab. Clin. N. Am. 2005, 35, 661–679.
- Kornelius, E.; Chang, K.L.; Yang, Y.S.; Huang, J.Y.; Ku, M.S.; Lee, K.Y.; Ho, S.W. Epidemiology and factors associated with mortality of thyroid storm in Taiwan: A nationwide population-based study. Intern. Emerg. Med. 2021, 16, 601–607.
- Galindo, R.J.; Hurtado, C.R.; Pasquel, F.J.; García Tome, R.; Peng, L.; Umpierrez, G.E. National Trends in Incidence, Mortality, and Clinical Outcomes of Patients Hospitalized for Thyrotoxicosis with and without Thyroid Storm in the United States, 2004–2013. Thyroid 2019, 29, 36–43.
- Sarlis, N.J.; Gourgiotis, L. Thyroid emergencies. Rev. Endocr. Metab. Disord. 2003, 4, 129–136.
- Silva, J.E.; Bianco, S.D. Thyroid-adrenergic interactions: Physiological and clinical implications. Thyroid 2008, 18, 157–165.
- Lorlowhakarn, K.; Kitphati, S.; Songngerndee, V.; Tanathaipakdee, C.; Sinphurmsukskul, S.; Siwamogsatham, S.; Puwanant, S.; Ariyachaipanich, A. Thyrotoxicosis-Induced Cardiomyopathy Complicated by Refractory Cardiogenic Shock Rescued by Extracorporeal Membrane Oxygenation. Am. J. Case Rep. 2022, 23, e935029.
- Sourial, K.; Borgan, S.M.; Mosquera, J.E.; Abdelghani, L.; Javaid, A. Thyroid Storm-induced Severe Dilated Cardiomyopathy and Ventricular Tachycardia. Cureus 2019, 11, e5079.
- Abera, B.T.; Abera, M.A.; Berhe, G.; Abreha, G.; Gebru, H.T.; Abraha, H.E.; Ebrahim, M.M. Thyrotoxicosis and dilated cardiomyopathy in developing countries. BMC Endocr. Disord. 2021, 21, 132.
- Soomro, R.; Campbell, N.; Campbell, S.; Lesniak, C.; Sullivan, M.; Ong, R.; Cheng, J.; Hossain, M.A. Thyroid storm complicated by multisystem organ failure requiring plasmapheresis to bridge to thyroidectomy: A case report and literature review. Clin. Case Rep. Rev. 2019, 5, 1–4.
- Burch, H.B.; Wartofsky, L. Life-threatening thyrotoxicosis. Thyroid Storm. Endocrinol. Metab. Clin. N. Am. 1993, 22, 263–277.
- Clark, O.H.; Duh, Q.; Kebebew, E. Textbook of Endocrine Surgery, 2nd ed.; Elsevier Saunders: Philadelphia, PA, USA, 2005; pp. 216–219.
- Sakaan, R.A.; Poole, M.A.; Long, B. Diltiazem-Induced Reversible Cardiogenic Shock in Thyroid Storm. Cureus 2021, 13, e19261.
- Arai, M.; Asaumi, Y.; Murata, S.; Matama, H.; Honda, S.; Otsuka, F.; Tahara, Y.; Kataoka, Y.; Nishimura, K.; Noguchi, T. Thyroid Storm Patients with Elevated Brain Natriuretic Peptide Levels and Associated Left Ventricular Dilatation May Require Percutaneous Mechanical Support. Crit. Care Explor. 2021, 3, e0599.
- Pandey, R.; Kumar, S.; Kotwal, N. Thyroid Storm: Clinical Manifestation, Pathophysiology, and Treatment; IntechOpen: London, UK, 2020.
- Carroll, R.; Matfin, G. Endocrine and Metabolic Emergencies: Thyroid Storm. Ther. Adv. Endocrinol. Metab. 2010, 1, 139–145.
- Jiménez-Labaig, P.; Mañe, J.M.; Rivero, M.P.; Lombardero, L.; Sancho, A.; López-Vivanco, G. Just an Acute Pulmonary Edema? Paraneoplastic Thyroid Storm Due to Invasive Mole. Case Rep. Oncol. 2022, 15, 566–572.
- Jayasuriya, A.; Muthukuda, D.; Dissanayake, P.; Subasinghe, S. Recurrent Thyroid Storm Caused by a Complete Hydatidiform Mole in a Perimenopausal Woman. Case Rep. Endocrinol. 2020, 2020, 8842987.
- Samra, T.; Kaur, R.; Sharma, N.; Chaudhary, L. Peri-operative concerns in a patient with thyroid storm secondary to molar pregnancy. Indian J. Anaesth. 2015, 59, 739–742.
- Kofinas, J.D.; Kruczek, A.; Sample, J.; Eglinton, G.S. Thyroid storm-induced multi-organ failure in the setting of gestational trophoblastic disease. J. Emerg. Med. 2015, 48, 35–38.
- Idowu, A.O.; Adesegun, O.A.; Osibowale, B.; Ajiro, T.; Ezuduemoih, D.; Osonuga, A. A case of thyroxine (T4) toxicosis complicated by thyroid storm with an unusual precipitant. Casp. J. Intern. Med. 2020, 11, 231–234.
- Kinoshita, H.; Sugino, H.; Oka, T.; Ichikawa, O.; Shimonaga, T.; Sumimoto, Y.; Kashiwabara, A.; Sakai, T. A case in which SGLT2 inhibitor is a contributing factor to takotsubo cardiomyopathy and heart failure. J. Cardiol. Cases 2020, 22, 177–180.
- Voll, M.; Øystese, K.A.; Høiskar, E.; Johansen, O.; Nyvold, C.; Norheim, I.; von Lueder, T.G.; Andersen, G. Case report: A patient with thyroid storm, refractory cardiogenic shock, and cardiac arrest treated with Lugol’s iodine solution and veno-arterial extracorporeal membrane oxygenation support. Eur. Heart J. 2021, 5, ytab017.
- Matsubara, M.; Tanaka, T.; Wakamiya, A.; Tamanaha, T.; Makino, H.; Tanei, T.; Aiba, T.; Kusano, K.; Hosoda, K. First Case Report of Arrhythmogenic Right Ventricular Cardiomyopathy Showing Refractory Ventricular Tachycardia Induced by Thyroid Storm due to Graves’ Disease. Case Rep. Endocrinol. 2022, 2022, 6078148.
- Pong, V.; Yeung, C.-Y.; Ko, R.L.-Y.; Tse, H.-F.; Siu, C.-W. Extracorporeal Membrane Oxygenation in Hyperthyroidism-Related Cardiomyopathy: Two Case Reports. J. Endocrinol. Metab. 2013, 3, 24–28.
- Bou Chaaya, R.G.; Saint, L.M.; Ilonze, O.J. Thyroidectomy in Mechanical Circulatory Support—A Salvage Treatment for Thyrotoxicosis-Induced Cardiogenic Shock: Case Series. VAD J. 2021, 7, e2021710.
- Nakashima, Y.; Kenzaka, T.; Okayama, M.; Kajii, E. A Case of Thyroid Storm with Cardiac Arrest. Int. Med. Case Rep. J. 2019, 12, 413–416.
- Martino, E.; Bartalena, L.; BogazziI, F.; Braveman, L.E. The Effects of Amiodarone on the Thyroid. Endocr. Soc. 2001, 22, 240–254.
- Ozcan, E.E.; Dogdus, M.; Yilancioglu, R.Y.; Adiyman, S.C.; Turan, O.E. Invasive Heart Rate Control as a Salvage Therapy in Amiodarone-induced Thyroid Storm. Medeniyet Med. J. 2022, 37, 119–122.
- Wu, W.-T.; Hsu, P.-C.; Huang, H.-L.; Chen, Y.-C.; Chien, S.-C. A Case of Takotsubo Cardiomyopathy Precipitated by Thyroid Storm and Diabetic Ketoacidosis with Poor Prognosis. Acta Cardiol. Sin. 2014, 30, 574–577.
- Chang, C.H.; Lian, H.W.; Sung, Y.F. Cystic Encephalomalacia in a Young Woman After Cardiac Arrest Due to Diabetic Ketoacidosis and Thyroid Storm. Cureus 2022, 14, e23707.
- Ikeoka, T.; Otsuka, H.; Fujita, N.; Masuda, Y.; Maeda, S.; Horie, I.; Ando, T.; Abiru, N.; Kawakami, A. Thyroid Storm Precipitated by Diabetic Ketoacidosis and Influenza A: A Case Report and Literature Review. Intern. Med. 2017, 56, 181–185.
- Lin, C.H.; Chen, S.C.; Lee, C.C.; Ko, P.C.; Chen, W.J. Thyroid storm concealing diabetic ketoacidosis leading to cardiac arrest. Resuscitation 2004, 63, 345–347.
- Brown, J.; Cham, M.D.; Huang, G.S. Storm and STEMI: A case report of unexpected cardiac complications of thyrotoxicosis. Eur. Heart J. Case Rep. 2020, 4, 1–5.
- Abbasi, A.A.; Chandar, P.; Shankar, S.; Gupta, S.S.; Kupfer, Y. Thyrotoxic Periodic Paralysis and Cardiomyopathy in a Patient with Graves’ Disease. Cureus 2018, 10, e2837.
- Das, B.B.; Shakti, D.; Akam-Venkata, J.; Obi, O.; Weiland, M.D.; Moskowitz, W. SARS-CoV-2 infection induced thyroid storm and heart failure in an adolescent girl. Cardiol. Young 2022, 32, 988–992.
- Pranasakti, M.E.; Talirasa, N.; Rasena, H.A.; Purwanto, R.Y.; Anwar, S.L. Thyrotoxicosis occurrence in SARS-CoV-2 infection: A case report. Ann. Med. Surg. 2022, 78, 103700.
- Razvi, S.; Jabbar, A.; Pingitore, A.; Danzi, S.; Biondi, B.; Klein, I.; Peeters, R.P.; Zaman, A.; Iervasi, G. Thyroid Hormones and Cardiovascular Function and Diseases. J. Am. Coll. Cardiol. 2018, 71, 1781–1796.
- Albakri, A. Thyrotoxic heart failure: A review of clinical status and meta-analysis of electrocardiogram diagnosis and medical clinical management methods. Integr. Mol. Med. 2018, 5, 2–11.
- Waqar, Z.; Avula, S.; Shah, J.; Ali, S.S. Cardiovascular Events in Patients with Thyroid Storm. J. Endocr. Soc. 2021, 5, bvab040.
- Satoh, T.; Isozaki, O.; Suzuki, A.; Wakino, S.; Iburi, T.; Tsuboi, K.; Kanamoto, N.; Otani, H.; Furukawa, Y.; Teramukai, S.; et al. 2016 Guidelines for the management of thyroid storm from The Japan Thyroid Association and Japan Endocrine Society (First edition). Endocr. J. 2016, 63, 1025–1064.
- Zayour, M.; Yasmin, F.A.; Baydoun, A.; Tawk, M.; Sleiman, D.; Shatila, W.; Chamoun, C. Cardiac Arrest as First Presentation of Thyroid Storm. Cureus 2023, 15, e37057.
- Osuna, P.M.; Udovcic, M.; Sharma, M. DHyperthyroidism and the Heart. Methodist DeBakey Cardiovasc. J. 2017, 13, 60–63.
- Chao, A.; Wang, C.H.; You, H.C.; Chou, N.K.; Yu, H.Y.; Chi, N.H.; Huang, S.C.; Wu, I.H.; Tseng, L.J.; Lin, M.H.; et al. Highlighting Indication of extracorporeal membrane oxygenation in endocrine emergencies. Sci. Rep. 2015, 5, 13361.
- Ali, H.; Sarfraz, S.; Hassan, L.; Ali, H. Atrial Fibrillation as an Initial Presentation of Apathetic Thyroid Storm. Cureus 2021, 13, e17786.
- Naik, S.K.; Hallak, N.; Patel, R.; Esan, A.; Saleh, A.; Sung, A.; Raoof, S. Reversible thyrotoxic cardiomyopathy: Prompt. Chest 2009, 136, 37S.
- Sugiyama, Y.; Tanaka, R.; Yoshiyama, Y.; Ichino, T.; Hishinuma, N.; Shimizu, S.; Imai, N.; Mitsuzawa, K.; Kawamata, M. A case of sudden onset of thyroid storm just before cesarean section manifesting congestive heart failure and pulmonary edema. JA Clin. Rep. 2017, 3, 20.
- Ueno, A.; Yamamoto, T.; Sato, N.; Tanaka, K. Ventricular fibrillation associated with early repolarization in a patient with thyroid storm. J. Interv. Card. Electrophysiol. 2010, 29, 93–96.
- Omar, A.M.A.; Knott, K.; Saba, M.M.; Lim, P.O. Cardiac arrest in myocardial infarction with non-obstructive coronary artery (MINOCA) secondary to thyroid dysfunction. BMJ Case Rep. 2023, 16, e253500.
- Korte, A.K.; Derde, L.; van Wijk, J.; Tjan, D.H. Sudden cardiac arrest as a presentation of Brugada syndrome unmasked by thyroid storm. BMJ Case Rep. 2015, 2015, bcr2015212351.
- Chaker, L.; van den Berg, M.E.; Niemeijer, M.N.; Franco, O.H.; Dehghan, A.; Hofman, A.; Rijnbeek, P.R.; Deckers, J.W.; Eijgelsheim, M.; Stricker, B.H.; et al. Thyroid Function and Sudden Cardiac Death: A Prospective Population-Based Cohort Study. Circulation 2016, 134, 713–722.
- Jao, Y.T.F.N.; Chen, Y.; Lee, W.-H.; Tai, F.-T. Thyroid storm and ventricular tachycardia. South. Med. J. 2004, 97, 604–607.
- Lencu, C.; Alexescu, T.; Petrulea, M.; Lencu, M. Respiratory manifestations in endocrine diseases. Clujul Med. 2016, 89, 459–463.
- Klomp, M.; Siegelaar, S.E.; van de Hoef, T.P.; Beijk, M.A.M. A case report of myocardial infarction with non-obstructive coronary artery disease: Graves’ disease-induced coronary artery vasospasm. Eur. Heart J. Case Rep. 2020, 4, 1–5.
- El-Menyar, A.A. Drug-induced myocardial infarction secondary to coronary artery spasm in teenagers and young adults. J. Postgrad. Med. 2006, 52, 51–56.
- Zheng, W.; Zhang, Y.J.; Li, S.Y.; Liu, L.-L.; Sun, J. Painless thyroiditis-induced acute myocardial infarction with normal coronary arteries. Am. J. Emerg. Med. 2015, 33, 983.
- Kataoka, S.; Matsuno, K.; Sugano, K.; Takahashi, K. Thyroid storm induced by combined nivolumab and ipilimumab immunotherapy in advanced non-small cell lung cancer. BMJ Case Rep. 2022, 15, e250696.
- Hammond, H.K.; White, F.C.; Buxton, I.L.; Saltzstein, P.; Brunton, L.L.; Longhurst, J.C. Increased myocardial beta-receptors and adrenergic responses in hyperthyroid pigs. Am. J. Physiol. 1987, 252, H283–H290.
- Lassnig, E.; Berent, R.; Auer, J.; Eber, B. Cardiogenic shock due to myocardial infarction caused by coronary vasospasm associated with hyperthyroidism. Int. J. Cardiol. 2003, 90, 333–335.
- Allencherril, J.; Birnbaum, I. Heart Failure in Thyrotoxic Cardiomyopathy: Extracorporeal Membrane Oxygenation Treatment for Graves’ Disease. JECT 2015, 47, 231–232.
- Tolu-Akinnawo, O.Z.; Abiade, J.; Awosanya, T.; Okafor, H.E. Thyrotoxicosis-Induced Cardiogenic Shock: Acute Management Using a Multidisciplinary Approach. Cureus 2022, 14, e32841.
- Taylor, G.M.; Pop, A.M.C.; McDowell, E.L. A case report of thyroid storm presenting as hemodynamic instability and acute kidney injury. Oxford Med. Case Rep. 2019, 2019, 252–255.
- Dahl, P.; Danzi, S.; Klein, I. Thyrotoxic cardiac disease. Curr. Heart Fail. Rep. 2008, 5, 170–176.
- Alam, S.; Zaman, J. Case study of thyrotoxic cardiomyopathy. BMJ Case Rep. 2019, 12, e228896.
- Subahi, A.; Ibrahim, W.; Abugroun, A. Diltiazem-Associated Cardiogenic Shock in Thyrotoxic Crisis. Am. J. Ther. 2018, 25, 1075–1078.
- Chariyawong, P.; Rao, A.; Panikkath, D.; Panikkath, R. Hyperthyroidism-induced dilated cardiomyopathy. Southwest Respir. Crit. Care Chron. 2019, 7, 64–66.
- Witczak, J.K.; Ubaysekara, N.; Ravindran, R.; Rice, S.; Yousef, Z.; Premawardhana, L.D. Significant cardiac disease complicating Graves’ disease in previously healthy young adults. Endocrinol. Diabetes Metab. Case Rep. 2019, 2020, 19-0132.
- Rana, A.; Assad, S.; Abuzaid, M.; Farooqi, A.; Nolte, J. Thyrotoxicosis-Induced Cardiogenic Shock with Encephalopathy and Acute Respiratory Distress: A Case Report and Literature Review. Cureus 2020, 12, e8213.
- Rushing, M.W.; Rebolledo, M.A.; Lahoti, A.; Alemzadeh, R. Acute febrile illness in a teenage female with history of Graves’ disease. Oxf. Med. Case Rep. 2023, 2023, omad050.
- Manuel, L.; Fong, L.; Lahanas, A.; Grant, P. How to do it: Plasmapheresis via venoarterial extracorporeal membrane oxygenation circuit for thyroid storm. Ann. Med. Surg. 2021, 67, 102485.
- Carhill, A.; Gutierrez, A.; Lakhia, R.; Nalini, R. Surviving the storm: Two cases of thyroid storm successfully treated with plasmapheresis. BMJ Case Rep. 2012, 2012, bcr2012006696.
- Amin, T.; Austin, C.P.; Udongwo, N.; Wiseman, K.; Parhar, A.S.; Chaughtai, S. Iodinated Contrast-Induced Thyroid Storm with Concomitant Cardiac Tamponade: A Case Report. Cureus 2022, 14, e28001.
- Bui, P.V.; Zaveri, S.N.; Pierce, J.R. Sanguinous pericardial effusion and cardiac tamponade in the setting of Graves’ disease: Report of a case and review of previously reported cases. Case Rep. Med. 2016, 2016, 9653412.
- Pokhrel, B.; Aiman, W.; Bhusal, K. Thyroid Storm. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023.
- Lim, S.L.; Wang, K.; Lui, P.L.; Ramanathan, K.; Yang, S.P. Crash Landing of Thyroid Storm: A Case Report and Review of the Role of Extra-Corporeal Systems. Front. Endocrinol. 2021, 12, 725559.
- Çiçek, V.; Çınar, T.; Selçuk, M.; Orhan, A.L. Acute Thyrotoxicosis Induced Reversible Cardiomyopathy in an Adult Patient. Hamidiye Med. J. 2021, 2, 138–140.
- Chao, J.; Cook, R.; Dhingra, V. Escaping a storm alive: A case report of a young woman’s acute presentation of thyroid storm leading to cardiac arrest salvaged by VA-ECMO. J. Clin. Anesth. Intensive Care 2021, 2, 26–30.
- Dalan, R.; Leow, M. Cardiovascular Collapse Associated with Beta Blockade in Thyroid Storm. Exp. Clin. Endocrinol. Diabetes 2007, 115, 392–396.
- Du, F.; Liu, S.W.; Yang, H.; Duan, R.X.; Ren, W.X. Thyrotoxicosis after a massive levothyroxine ingestion: A case report. World J. Clin. Cases 2022, 10, 3624–3629.
- Noh, K.W.; Seon, C.S.; Choi, J.W.; Cho, Y.B.; Park, J.Y.; Kim, H.J. Thyroid Storm and Reversible Thyrotoxic Cardiomyopathy After Ingestion of Seafood Stew Thought to Contain Marine Neurotoxin. Thyroid 2011, 21, 679–682.
- Yamashita, Y.; Iguchi, M.; Nakatani, R.; Usui, T.; Takagi, D.; Hamatani, Y.; Unoki, T.; Ishii, M.; Ogawa, H.; Masunaga, N.; et al. Thyroid Storm with Heart Failure Treated with a Short-acting Beta-adrenoreceptor Blocker, Landiolol Hydrochloride. Intern. Med. 2015, 54, 1633–1637.
- Misumi, K.; Kodera, S.; Nagura, F.; Kushida, S.; Shiojiri, T.; Kanda, J. Cardiac arrest caused by landiolol in a patient in thyroid crisis. J. Cardiol. Cases 2016, 14, 62–64.
- Frenkel, A.; Bichovsky, Y.; Arotsker, N.; Besser, L.; Joshua, B.Z.; Fraenkel, M.; Zahger, D.; Klein, M. Ivabradine for Uncontrolled Sinus Tachycardia in Thyrotoxic Cardiomyopathy–Case Report. Endocr. Metab. Immune Disord. Drug Targets 2023, 23, 992–995.
- Dyer, M.; Neal, M.D.; Rollins-Raval, M.A.; Raval, J.S. Simultaneous Extracorporeal membrane oxygenation and therapeutic plasma exchange procedures are tolerable in both pediatric and adult patients. Transfusion 2014, 54, 1158–1165.
- Cheah, J.M.; Ng, D.; Low, M.Y.; Foo, S.H. Weathering the Crisis: A Case of Thyroid Crisis with Propranolol-Induced Circulatory Collapse Successfully Treated with Therapeutic Plasma Exchange. ASEAN Fed. Endocr. Soc. 2019, 34, 206–209.
- Park, H.S.; Kwon, S.K.; Kim, Y.N. Successful Treatment of Thyroid Storm Presenting as Recurrent Cardiac Arrest and Subsequent Multiorgan Failure by Continuous Renal Replacement Therapy. Endocrinol. Diabetes Metab. 2017, 16, 0115.
- Tandukar, S.; Palevsky, P.M. Continuous Renal Replacement Therapy: Who, When, Why, and How. Chest 2019, 155, 626–638.
- Khan, T.M.; Siddiqui, A.H. Intra-Aortic Balloon Pump. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023.
- Glazier, J.J.; Kaki, A. The Impella Device: Historical Background, Clinical Applications and Future Directions. Int. J. Angiol. 2019, 28, 118–123.
- Fu, Y.; Ge, H.; Zhang, Y.; Li, Y.; Mu, B.; Shang, W.; Li, S.; Ma, Q. Targeted Temperature Management for In-hospital Cardiac Arrest Caused by Thyroid Storm: A Case Report. Front. Cardiovasc. Med. 2021, 8, 634987.
- Biello, A.; Kinberg, E.C.; Wirtz, E.D. Thyroidectomy. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022.
- Klubo-Gwiezdzinska, J.; Wartofsky, L. Thyroid emergencies. Med. Clin. N. Am. 2012, 96, 385–403.
