Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 3 by Jessie Wu and Version 2 by Jessie Wu.
Alzheimer’s disease (AD) is a neurological disorder in humans caused by complex pathophysiological mechanisms that lead to loss of memory and cognition, death of neurons, loss of synapses, and damage of the brain, which culminates in death.
- Alzheimer’s disease
- medicinal plants
- ‘ginseng
- gotu kola
1. Treatment of Alzheimer’s Disease
There are already more than 55 million cases of Alzheimer’s disease (AD) documented globally, and by 2050, the overall number of AD patients is expected to more than triple [1][2]. Even though it is a serious health issue proper and complete treatment is not available, treatment strategies used today concentrate on assisting patients in managing behavioural symptoms, sustaining mental function, and delaying or preventing the signs of illness. Two treatment strategies can be adopted as discussed below.
1.1. Chemical-Based Treatment
Despite the fact that AD is a public health problem, there are currently only two classes of medications that have been approved by the FDA to treat AD: cholinesterase enzyme inhibitors (naturally occurring, synthetic, and hybrid analogues), and antagonists to N-methyl D-aspartate (NMDA).
1.1.1. Cholinesterase Inhibitors
According to the cholinergic theory, a reduction in the synthesis of acetylcholine (ACh) causes AD. A reduction in acetylcholinesterase along with an increase in cholinergic levels is one therapy that enhances neuronal cell and cognitive function [3]. Acetylcholine breakdown in synapses is prevented by acetylcholinesterase inhibitors (AChEIs), leading to continuous ACh build up and cholinergic receptor activation. Another approach to treating AD may involve raising choline reuptake and, consequently, the generation of acetylcholine at presynaptic terminals. This might be done by focusing on the choline transporter (CHT1), which is in charge of supplying the choline required for the synthesis of ACh [3][4]. Different AChEIs are donepezil, rivastigmine, and galantamine.
Donepezil
The most effective medication for treating AD is donepezil, which is a derivative of indanonebenzylpiperidine and a member of the second generation of acetylcholinesterase inhibitors (AChEIs). Due to donepezil’s reversible binding to acetylcholinesterase, there is more ACh present at the synapses and prevents it from being hydrolysed. With transient cholinergic side effects that affect the neurological, as well as gastrointestinal systems, the medicine may be tolerated by the patient. Notably, donepezil is used to treat AD symptoms, such as improving cognition and behaviour [5][6]. Due to an imbalance in acetylcholine, unusual adverse reactions such as extrapyramidal side effects are more likely to occur when AD medication is used along with psychiatric medicines. A case of an extrapyramidal adverse response brought on by the donepezil and risperidone combination was reported [7]. The patient experienced fatigue, nausea, panic, sweating, and vomiting.
Rivastigmine
It is a butyrylcholinesterase (BuChE) and acetylcholinesterase (AChE) pseudo-irreversible inhibitor. In order to function, it binds to the two active sites of AChE which are estearic and anionic sites, which stops acetylcholine (Ach) metabolism [8]. In the healthy brain, glial cells contain BuChE and have only a 10% activity level compared to the AD brain, where it has a 40–90% activity level, while simultaneously reducing ACh activity. This implies that BuChE activity can be a sign of mild to severe AD. Rivastigmine is metabolised by AChE and BuChE at the synapses and dissociates slower than AChE, which is why it is known as a pseudo-irreversible. The drug is used for the treatment of mild to moderate AD. It ameliorates daily activities and cognitive processes [9][10]. The most common adverse effects of rivastigmine are gastrointestinal problems such as bladder pain, painful urination, etc.
Galantamine (GAL)
For mild to severe AD cases, it is regarded as a conventional first-line medication. Galantamine is a dual-mode selective tertiary isoquinoline alkaloid, which not only acts as a competitive inhibitor of AChE but also has the ability to allosterically bind to and activate the nicotinic acetylcholine receptors subunit. Like other AChE inhibitors, GAL has good efficacy and tolerability and can reduce behavioural symptoms and improve daily activities, cognitive performance, and mood [11][12]. For transporting the medicine only to the areas of the brain that were injured, it is linked to hydroxyapatite particles that contain ceria. To transport GAL hydrobromide, some researchers have used solid-lipid nanoparticles and nano emulsification techniques [13]. The results of these tests are promising for the safe administration of the drug. Nasal delivery of a GAL hydrobromide–chitosan combination of nanoparticles has good pharmacological potential, while the controlled release dose of the drug has been transported via the patch technique by another group. The common problems associated with this drug are gastrointestinal problems, headache, dizziness, insomnia, weight loss, loss of appetite, etc. [13][14].
1.1.2. N-methyl D-aspartate Receptor (NMDAR) Antagonists
It is thought that NMDAR performs an important role in the pathophysiology of AD. Ca2+ influx brought on by NMDAR activation promotes signal transduction, and results in gene transcription that is required for the growth of long-term potentiation (LTP), which is essential for the establishment of synaptic neurotransmission, plasticity, and memory [15]. Excessive NMDAR activation overstimulates glutamate, the main excitatory amino acid in the CNS, which results in excitotoxicity, synaptic malfunction, neuronal cell death, and damage to cognitive abilities. Numerous NMDAR uncompetitive antagonists have been created and tested in clinical settings, though the majority of them were ineffective and had undesirable side effects [16]. The sole drug in this class that is approved for the treatment of moderate to severe AD is memantine.
Memantine
It is an uncompetitive, low-affinity antagonist of the glutamate receptor subtype. To treat mild to severe AD, memantine is administered alone or in combination with AChEI [12]. The drug has a low affinity and is quickly displaced from NMDAR by high quantities of glutamate. It blocks excitatory receptors without impairing regular synaptic communication, which makes it harmless, well tolerable, and avoids a long-lasting blockage. Possible adverse effects of memantine are dizziness, constipation, vomiting, hypertension, and headache [17].
1.2. Plant-Based Treatment
Currently available synthetic medicines are effective only for 1–4 years for mild to moderate AD. Synthetic medicine exhibits many negative side effects [18]. Scientific evidence related to the efficacy of phytochemicals in the prevention and treatment of AD has been accumulating which shows that they are safe and cost effective. Oxidative stress is one of the proven causes of AD. However, plants are reservoirs of antioxidants which can mitigate the effects of AD [19][20]. Several plants were examined for their ability to combat AD as listed in Table 1 and also shown in Figure 1. A diet high in plants has repeatedly been linked to a lower risk of AD. It is advised to consume fruits, vegetables, cereals, and nuts on a regular basis for overall health, to promote healthy ageing, and to reduce the risk of age-related disorders such as AD [21][22].
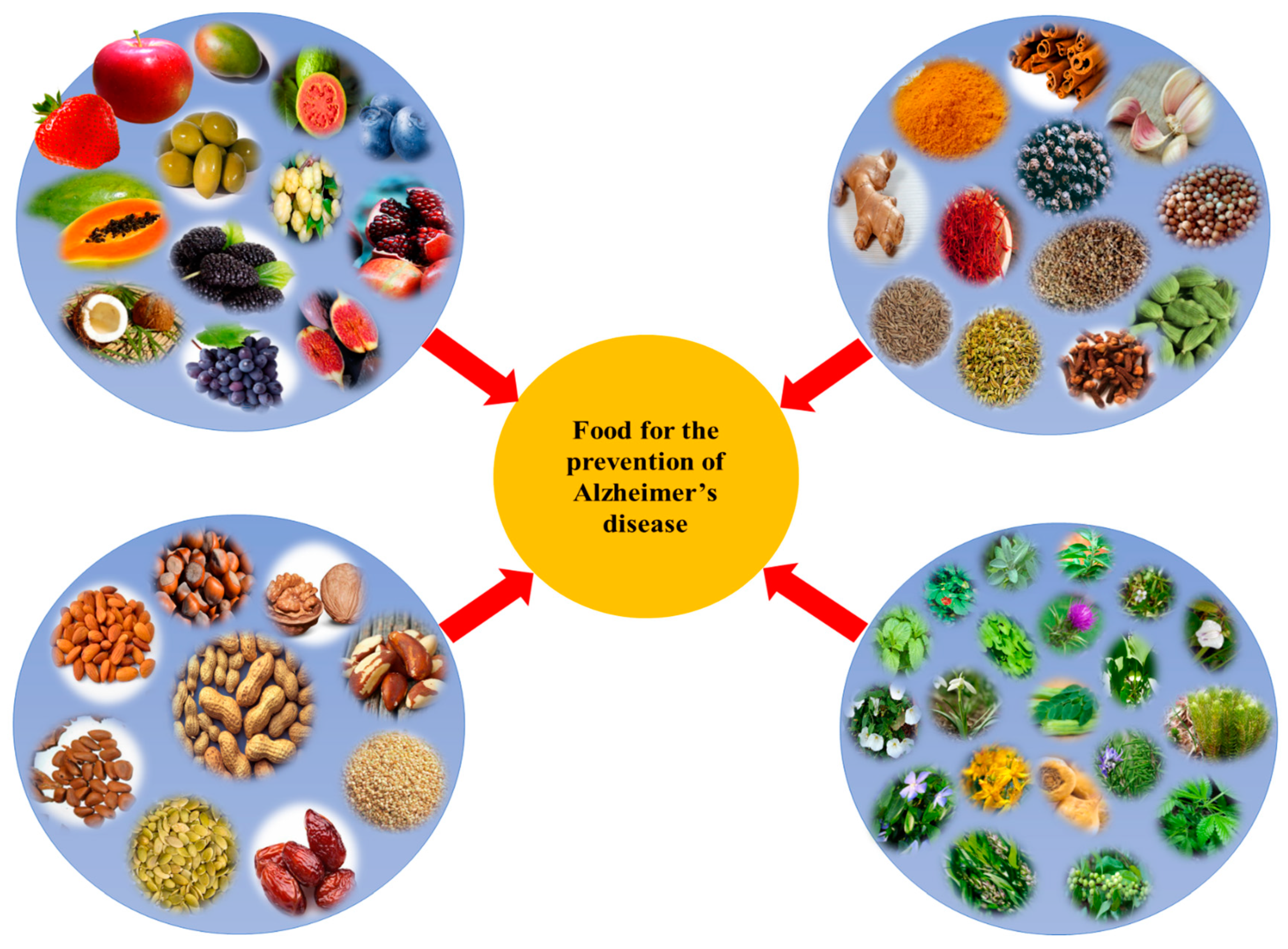
Figure 1. Different plant-based foods used for the prevention of Alzheimer’s disease (AD).
Table 1. Different plants possessing anti-Alzheimer properties.
| Plant | Botanical Name | Family | Part Used | Active Compounds | Properties | References |
|---|---|---|---|---|---|---|
| Ashwangdha | Withania somnifera | Solanaceae | Roots | Glycowithanolides (Withaferin A, Withasomniferin A) | It has neuroprotective functions. | [23][24] |
| Brahmi | Bacopa monnieri | Plantaginaceae | Arial parts | Brahmine, bacosides A and B, apigenin, and quercetin | It works as a memory enhancer. | [25] |
| Calabar bean | Physostigma venenosum | Fabaceae | Seeds | physostigmine | It has acetylcholinesterase inhibitor activities. | [26] |
| Coffee | Coffea arabica | Rubiaceae | Seeds | Caffeic acid, chlorogenic acid | It is effective against Alzheimer’s disease. | [27] |
| Milk thistle | Silybum marianum | Asteraceae | Seeds | Silymarin | It acts as a scavenger of free radicals and protects the central nervous system against any injury and memory impairment. | [28] |
| Guggulu | Commiphora wightii | Burseraceae | Bark | Ferulic acid, commiphoric acid, eugenol, and commophorinic acid | It acts as a scavenger of superoxide radicals. | [29] |
| German chamomile | Matricaria recutita | Asteraceae | leaves | apigenin | It helps in stimulating the brain and calms the nerves. | [30] |
| Blueberry | Vaccinium corymbosum | Ericaceae | Fruit | Antioxidants, vitamins C, B, β-carotene, lutein, and zeaxanthin | It has anti-inflammatory and antidiabetic, properties, and also helps in preventing Alzheimer’s disease. | [31][32] |
| Rosemary | Rosmarinus officinalis | Lamiaceae | Leaves | Carnosic acid, carnosol, rosemanol, rosmarinic acid, and α-pinene | It has antioxidant properties and reduces the risk of AD. | [33] |
| Snowdrop | Galanthus nivalis | Amaryllidaceae | Bulbs | Galanthamine, nivalidine, narwedine, and lycorine | It has antioxidant and antiamyloid activities. | [34] |
| Turmeric | Curcuma longa | Zingiberaceae | Rhizome | Curcumin, bisdemethoxycurcumin, eugenol demethoxycurcumin, zingiberene dihydrocurcumin, azulene, D-camphene, caprylic acid, cineol, and turmerone | It has antioxidant properties so it helps in preventing Alzheimer’s disease. | [35][36] |
| St. John Wort | Hypericum perforatum | Hypericaceae | Entire plant | quercetin, Hypericin, rutin quercetin, and isorhamnetin, | It possesses antioxidant and antiamyloid activities. | [37][38] |
| Black pepper | Piper nigrum | Piperaceae | Seeds | piperine | It reduces acetylcholinesterase levels and shows better results in the treatment of Alzheimer’s disease. | [39] |
| Garlic | Allium sativum | Lilliaceae | Cloves | S-allyl-cysteine, S-allyl-mercaptocysteine Biophenols: caffeic acid, and ferulic acid | It shows antiamyloid and antitangle properties. | [40][41] |
| Ginkgo | Ginkgo biloba | Ginkgoaceae | Leaves | Ginkgolides A, B, C, J and M, bilobalide, quercetin, sesquiterpene kaempferol, and isorhamnetin | It has antioxidant properties. It increases the blood flow in the brain and acts as a scavenger of free radicals and shows neuroprotective properties. | [42][43] |
| Coriander | Coriandrum sativum | Apiaceae | Leaves | Camphor, limonene, alpha-pinene, geraniol, petroselinic acid, and linalool | It helps in improving memory and also helps in managing Alzheimer’s disease. | [44][45] |
| Sesame | Sesamum indicum | Pedaliaceae | seeds | Sesaminol, sesamine | It shows neuroprotective properties. | [46] |
| Apple | Malus pumila | Rosaceae | Fruit | Quercetin, catechin, and epicatechin | It improves cognitive functions. | [47] |
| Ginseng | Panax ginseng | Araliaceae | Roots | Ginsenosides, gintonin | It improves the functioning of the central nervous system, and it also shows anti-amyloid activity. | [48][49] |
| Mulberry | Morus alba | Moraceae | Fruit | resveratrol, oxyresveratrol, chlorogenic acid, mulberroside, moracin, and maclurin | It has antioxidant properties and helps in lowering the risk of AD. | [50] |
| Gotu kola | Centella asiatica | Apiaceae | Leaves | Quercetin, myricetin, kaempferol, rutin, and apigenin | It possesses anti-amyloid properties. | [51] |
| Seneca snakeroot | Polygala tenuifolia | Polygalaceae | Roots | Tenuigenin, tenuifolin, and xanthone glycosides | It acts as an acetylcholinesterase and beta-secretase 1 inhibitor. | [52][53] |
| Golden root | Rhodiola rosea | Crassulaceae | Roots | Rosavin, salidroside, rosin, cinnamoyl alcohol, and tyrosol | It has very good antioxidant activity and also acts as a cognitive enhancer. | [54][55] |
| Lemon balm | Melissa officinalis | Lamiaceae | Leaves | Citral, protocatechuic acid, caffeic acid, and rosmarinic acid | It acts as a memory enhancer. | [56] |
| Dwarf periwinkle | Vinca minor | Apocynaceae | Upper parts | Vinpocetine, apovincaminic acid, kaempferol glycosides, hydroxybenzoic acids, and chlorogenic acid | It acts as a memory enhancer and also shows antioxidant properties. | [57] |
| Green tea | Camellia sinensis | Theaceae | Leaves | Gallocatechin, Gallic acid, epigallocatechin, epicatechin, epigallocatechin gallate, and caffeine | It possesses antioxidant and antiamyloid activities. | [58][59] |
| Grapes | Vitis vinifera | Vitaceae | Fruit | Resveratrol, quercetin, and catechins | It has antioxidant and antiamyloid properties and is used in preventing neurodegeneration. | [60] |
| Marijuana | Cannabis sativa | Cannabaceae | Bud and leaves | Tetrahydrocannabinol, cannabidiol | It shows antiamyloid activity. | [61] |
| Olive | Olea europaea | Oleaceae | Fruit, oil, leaves | Oleuropein, tyrosol, hydroxytyrosol, caffeic acid, verbascoside, and rutin | It possesses antioxidant, anti-inflammatory, and antiamyloid properties. | [62] |
| Brazil nut | Bertholettia excelsa | Lecythidaceae | Nut | Lecithin | It increases the level of acetylcholine n AD patients. | [63] |
| firmoss | Huperzia serrata | Lycopodiaceae | Aerial parts | Huperzines | It possesses antiamyloid activity. | [64] |
| Pomegranate | Punica granatum | Punicaceae | Fruit | Ellagic acid, gallagic acid punicalagin, and punicic acid | It possesses antioxidant and antiamyloid activities. | [65][66] |
| Marapuama | Ptychopetalum olacoides | Olacaceae | Roots | Ptychonal, muirapuamine, and theobromine | It possesses antiamnesic, anticholinesterase, and neuroprotective properties. | [67][68] |
| Fennel | Foeniculum vulgare | Apiaceae | Seed | Estragole, limonene, fenchone, and β-myrcene | It shows an inhibitory effect against acetylcholinesterase and butyrlcholinesterase. | [69] |
| Papaya | Carica papaya | Caricaceae | Fruit | Quercetin, β-sitosterol | It possesses radical scavenging activity. | [70] |
| Saffron | Crocus sativus | Iridaceae | Stigma | Crocin, crocetin, picrocrocin, safranin, and safranal, | It possesses antioxidant and antiamyloid activities. | [71] |
| Ginger | Zingiber officinale | Zingiberaceae | Rhizome | Shagol, gingerol, zingerone | It shows antioxidant properties. | [72] |
| Sage | Salvia officinalis | Lamiaceae | Leaves | Rosmarinic acid, thujone, cineol, and camphor | It shows antioxidant properties. It has cognitive-enhancing properties and helps in preventing age-related problems. | [73] |
| Camb | Caryocar brasiliense | Caryocaracea | Leaf | Gallic acid, quinic acid, quercetin, and quercetin 3-o arabinose | It has neuroprotective effects. | [74] |
| Coconut | Cocos nucifera | Arecaceae | Seed | Caproic acid, Caprylic acid, Capric acid, Lauric acid, and Myristic acid | It helps in preventing Alzheimer’s disease. | [75] |
| Gouteng | Uncaria rhynchophylla | Rubiaceae | Stem | Rhynchophylline, isorhynchophylline, and hirsuteine | It shows free radical scavenging activity and also exhibits protection against kainic acid-induced neuronal damage. | [76] |
| Aloe vera | Aloe barbadensis miller | Aloaceae | Juice | Aloin, β-secretase, aloe-emodin | It improves brain functioning. | [77] |
| Wuzhuyu | Tetradium ruticarpum | Rutaceae | Fruit | Evodiamine, rutaecarpine, evocarpine, and quinoline | It increases the blood flow in the brain and also inhibits the effect of acetylcholinesterase. | [78] |
| Moringa | Moring oleifera | Moringaceae | Leaves | Glycoside niazirin, niaziminim A and B, | It maintains the monoamine level in the brain and helps in treating Alzheimer’s disease. | [79] |
| Walnut | Juglans regia | Juglandaceae | Kernel | α-tocopherol, ellagic acid, and juglone | It reduces the risk of Alzheimer’s disease by reducing oxidative stress and it also shows amyloidogenic activity. | [80][81] |
| Cinnamon | Cinnamomum verum | Lauraceae | Extract of bark | Cinnamaldehyde, eugenol, and trans cinnamaldehyde | It promotes the disassembly of tau filaments and also shows anti-inflammatory activity. | [82] |
| Tahitian gooseberry | Phyllanthus acidus | Phyllanthaceae | Fruit | Terpine | It lowers oxidative stress, decreases lipid peroxidation, and helps in increasing the level of antioxidant enzymes in the brain. | [83] |
| Fig | Ficus carica | Moraceae | Fruit | Quercetin, C-Sitosterol | It has antioxidant activity, exhibits memory-enhancing effects and better learning abilities. | [84] |
| Pumpkin | Cucurbita maxima | Cucurbitaceae | seeds | Ferulic acid, caffeic acid, and coumaric acid | It has antioxidant properties and helps in relieving stress. | [85] |
| Shankhpushpi | Convolvulus pluricaulis | Convolvulaceae | Whole plant | Flavonol glycosides, anthocyanins, and triterpenoids | It is consumed as a tonic for enhancing memory and it calms the nerves. | [86][87] |
| Strawberry | Fragaria ananassa | Rosaceae | Fruit | Pelargonidin | It has antioxidant properties. | [88] |
| Butterfly pea | Clitoria ternatea | Fabaceae | Root and leaf extract | Myricetin, quercetin | It shows antioxidant properties and AChE inhibitor activities. | [89] |
| Broccoli | Brassica oleracea var. italica | Brassicaceae | Floret | Kaempferol, sulforaphane | It possesses antioxidant activities and reduces cerebral oedema. | [90] |
| Spinach | Spinacia oleracea | Amaranthaceae | Leaves | Ferulic acid, coumaric acid, quercetin, spinacetin, and myricetin, | It reduces the neuronal death and production of ROS. | [91] |
| Date palm | Phoenix dactylifera L. | Arecaceae | Fruit | Cinnamic acid, caffeic acid, protocatechuic, gallic acid, dactylifiric acid, and epicatechin | It has antioxidant properties and helps in enhancing memory | [92] |
2. Different Plants with Anti-Alzheimer Properties
Different plants belonging to the families Solanaceae, Plantaginaceae, Fabaceae, Rubiaceae, Asteraceae, Ericaceae, Amaryllidaceae, Zingiberaceae, Pedaliaceae, Hypericaceae, Piperaceae, Lilliaceae, Ginkgoaceae, Apiaceae, Araliaceae, Polygalaceae, Crassulaceae, Lamiaceae, Apocynaceae, Theaceae, Vitaceae, Cannabaceae, Oleaceae, Lycopodiaceae, Punicaceae, Iridaceae, Lamiaceae, Caryocaracea, Arecaceae, Aloaceae, Rutaceae, Moringaceae, Juglandaceae, Lauraceae, Phyllanthaceae, Moraceae, Convolvulaceae, Halymeniaceae, Rosaceae, etc., have anti-Alzheimer properties and have been used for the treatment of AD.
2.1. Ginseng
Panax ginseng (family: Araliaceae), commonly known as ‘ginseng’ is one of the well-known herbs in China, Japan, and Korea used to treat AD. It consists of phytochemicals such as ginsenosides (saponins), a derivative of the triterpenoid dammarane, and 20(S)-protopanaxadiol, which prevents β-amyloid from aggregating and clears it from neurons, relieves mitochondrial dysfunction, and boosts the secretion of the neurotrophic factor [44][45]. According to a molecular enzyme study, ginsenosides have substantial AChE inhibitory activities, which is an efficient strategy for lowering the symptoms of AD [93][94]. Through the stimulation of phosphatidic acid receptors involved in hemolysis, the bioactive glycoprotein gintonin lowers the production of Aβ and enhances learning and memory. Additionally, it reduces AD symptoms by promoting autophagy, anti-inflammatory mechanisms, antiapoptosis, and management of oxidative stress, as proven by comprehensive in vivo and in vitro investigations [95]. Gintonin modulates the G protein-coupled lysophosphatidic acid receptors which affect the cholinergic system and neurotrophic factors, reducing the level of plaque formation. In a clinical experiment with a limited sample size of 10 people who had mild cognitive impairment or early dementia, gintonin intake (300 mg/day, 12 weeks) significantly enhanced Korean mini mental state test scores at 4 and 8 weeks compared to baseline scores. In contrast, gintonin consumption (300 mg/day, 4 weeks) significantly raised the ADAS-Cog-K and ADAS-non-Cog-K scores on the Korean cognitive subscale of the Alzheimer’s disease assessment scale after 4 weeks compared to the baseline scores. When it comes to gintonin toxicity in humans, none of the patients reported any negative side effects during the 12-week dose of gintonin. Hence, gintonin administration to older subjects with cognitive impairment was safe and well tolerated [96].
2.2. Gotu Kola
Centella asiatica (family: Apiaceae) is commonly called ‘gotu kola’. It is a widespread persistent herbaceous climber in Asia. It is used in traditional medicines for the purpose of regenerating brain cells and enhancing memory, lifespan, and intellect [51]. Animal studies have shown that Centella asiatica has an impact on neuronal structure, learning ability, and memory-retaining ability. It has been shown to improve cognitive performance by reducing phospholipase A2 (PLA2) activity, suppressing acetylcholinesterase activity, preventing the formation of amyloid, and preventing brain damage [97][98]. In preclinical studies, Centella asiatica was also discovered to have antidepressant, anxiolytic, antistress, and seizure-prevention properties [99][100]. It has been shown to affect metabolic pathways connected to AD when administered to 5xFAD mice [101]. In rats overexpressed with β-amyloid, Centella asiatica extract has been demonstrated to enhance memory and decision-making, while it lowers hippocampus mitochondrial dysfunctioning. In a clinical investigation, a 70% water-ethanol extract of C. asiatica demonstrated promising anxiolytic properties by reducing anxiety and stress in patients [101].
2.3. Ginkgo
Ginkgo biloba (family: Ginkgoaceae) is commonly known as ‘ginkgo’. It is the most well-known herb for treating Alzheimer’s and its symptoms. Terpene lactones and flavone glycosides are both present in plant extracts. The terpene lactones include bilobalide A, B, and C, and ginkgolides, while the flavone glycosides include kaempferol, quercetin, and isorhamnetin [38]. Through the control of glutathione peroxidase, catalase, and superoxide dismutase (SOD) activity, this herbal extract shields against Aβ generated neurotoxicity by preventing apoptosis of neurons, reactive oxygen species (ROS) collection, glucose assimilation, mitochondrial dysfunctioning, and activation of the extracellular signal-regulated kinase (ERK) pathway [42][43]. Numerous studies have connected astrocytosis, microgliosis, and the presence of proinflammatory substances to the deposition of Aβ peptides [102]. G. biloba extracts demonstrated therapeutic advantage in AD, compared to donepezil, with few unfavourable side effects. It is most recognized for its capacity to improve circulation (vasorelaxing effect) throughout the body. G. biloba can thus reduce blood pressure and prevent platelet aggregation [103]. In an experiment involving 18 randomized clinical trials (RCTs) with 1642 individuals, 842 of them were in the experimental group (donepezil hydrochloride plus G. biloba formulations) and 800 were in the control group (donepezil), it was observed that donepezil with G. biloba can enhance clinical efficacy rates and verbal memory. However, to validate this, more stringent trials will be required in the future [104].
2.4. Turmeric
Curcuma longa (family: Zingiberaceae) is commonly known as ‘turmeric’. Curcuminoids, such as curcumin, demethoxycurcumin, and bis-demethoxycurcumin, are the phytochemicals present in turmeric. The primary curcuminoid is curcumin, which gives turmeric roots their characteristically yellow colour. According to research, curcumin may be a potential drug for treating AD [105]. The level of oxidative damage in the brain can be reduced by curcumin. It has been shown that curcumin can reverse β-amyloid pathology in a mouse model with AD [106]. The antioxidant and anti-inflammatory properties of curcumin also facilitated in alleviating of some AD symptoms [35][36]. The capacity of the Early Growth Response-1 (Egr1) protein to bind DNA is inhibited by curcumin, which reduces inflammation. Activated microglia and astrocytes produce chemokines which are known to cause monocyte chemotaxis and are also inhibited by curcumin at the CNS. Effective ways to stop proinflammatory cytokine activation include decreasing the production of ROS by stimulating neutrophils and suppressing the tumor necrosis factor α (TNF-α) and interleukin-1 (IL-1) inflammatory cytokine expression [107][108]. Curcumin inhibits the activity of the activator protein (AP-1), a transcription factor involved in the synthesis of amyloid. The capacity of curcuminoids to prevent the generation and spread of free radicals is proof that they possess potent antioxidant effects. It also prevents the oxidation of free radicals and low-density lipoproteins which causes the destruction of neurons in AD and other neurodegenerative diseases.
2.5. Brahmi
Bacopa monnieri (family: Plantaginaceae) commonly known as ‘brahmi’ is a persistent creeper that is indigenous to the swamps of eastern and southern India, together with Australia, Europe, Africa, Asia, North and South America, and the Middle East. In traditional medicine, it is frequently used as a cardiotonic, diuretic, and nerve tonic [109][110]. The main phytochemicals of Brahmi are Brahmine, bacosides A and B, apigenin, quercetin, bacosaponins A, and bacosaponins B. Protein kinase activity is increased by B. monnieri extracts, which has a nootropic effect. Rats administered Brahmi extract displayed reduced cholinergic degradation and an improvement in cognition. Additionally, it also shields neural cells from the harm done by β-amyloids [110]. B. monnieri extract treatment resulted in decreased ROS levels in neural cells, indicating that it reduces intracellular oxidative stress. Cognitive abilities significantly increase with regular use of Brahmi, which also reduced their levels of inflammation and oxidative stress [111]. In addition, a team of researchers found that an extract of standardised B. monnieri corrected the cognitive abnormalities brought on by the intracerebroventricular administration of colchicines and ibotenic acid into the nucleus basalis magnocellularis. In the same study, Bacopa monnieri also restored acetylcholine depletion, choline acetyltransferase activity reduction, and reduction of muscarinic cholinergic receptor binding in the frontal cortex and hippocampal regions [112]. By suppressing cellular acetylcholinesterase activity, Brahmi extracts prevent beta-amyloid-induced cell death in neurons. In a study (randomized, double-blinded trial) involving 81 persons of the age group 55 and above, a 12-week cycle of Bacopa considerably improved memory acquisition and retention [113].
2.6. Ashwagandha
Withania somnifera (family: Solanaceae) is commonly known as ‘ashwagandha’ and is regarded as a Rasayana (rejuvenating). It possesses antioxidant properties, characteristic of free radical scavengers. The chemical composition of ashwagandha root includes alkaloids, anolides, many sitoindosides, and flavonoids [114][115]. According to a molecular study, ashwagandha root helps in treating AD by preventing nuclear factor B activation, promoting nuclear factor erythroid 2-related factor 2 (Nrf2) migration to the nucleus, where it enhances the expression of antioxidant enzymes, to reduce the formation of amyloid, decrease apoptotic cell death, restore synaptic function, and boosts the immune system [116]. In certain research, ashwagandha root methanolic preparations were used to treat human neuroblastoma SK-N-SH cells, which led to an increase in dendritic extension, neurite outgrowth, and synapse formation. Researchers have hypothesised that the ashwagandha root extracts are effective in treating neurodegenerative illnesses and also promote neurite growth, and have anti-inflammatory, antiapoptotic, and anxiolytic effects. Moreover, they have the capacity to minimise mitochondrial dysfunctioning, boost antioxidant defence levels, reduce glutathione levels, and can cross the blood–brain barrier and reduce inflammation in the brain [117]. In a double-blind, randomized, placebo-controlled study, 50 participants with moderate cognitive impairment (MCI) were treated with a 300 mg dose of W. somnifera root extract twice daily for an eight-week period. After eight weeks, the W. somnifera-treated group displayed considerable improvements in their ability to process information, concentrate, and use executive functions [118].
2.7. Saffron
Crocus sativus (family: Iridaceae) commonly known as ‘saffron’, possesses antioxidant, anticancer, and aphrodisiac properties and also improves memory in adults. Numerous studies have shown that saffron possesses antioxidative, anti-inflammatory and antiamyloidogenic properties. Additionally, saffron is said to be helpful in reducing acetylcholinesterase and protecting against toxins (AChE). AChE is connected to the neurofibrillary tangles and beta-amyloid plaques that are characteristic of AD [119].
To analyse the effect of saffron on learning abilities, and the prevention of oxidative stress, each rat was administered five and ten grams of saffron extract, twice a week. Oxidative stress markers were assessed seven days later. The group that received saffron treatment was found to have a reduced memory deficit along with enhanced spatial learning and antioxidant activity of enzymes [120]. The main bioactive compound of saffron is crocin. It has the ability to bind to the hydrophobic region of Aβ and thus inhibits its aggregation [121]. A double-blinded/phase II study using the AD assessment scale, cognitive subscale, clinical dementia rating scale, and sums of boxes scores was conducted on a total of 54 patients who were 55 years of age or older with AD. These patients received saffron extractive (30 mg) or donepezil (10 mg) as a positive control once daily for 22 weeks. As a result, donepezil and saffron extractives had similar effects on patients with mild to moderate AD, suggesting that saffron extractives have a therapeutic effect [71].
2.8. Ginger
Zingiber officinale (family: Zingiberaceae) commonly called ‘ginger’ is a spice having both culinary and therapeutic uses. It is frequently used as a nutritional supplement, in ginger tea preparation, or as an extract. The primary bioactive components in ginger include gingerols, shagols, volatile oils such as bisabolene and zingiberene, and monoterpenes. In vitro research has been done on the AChE inhibitory activity of red and white ginger [122]. Inhibition of AChE causes acetylcholine to accumulate in synapses, which is followed by an increase in the cholinergic pathway activity and results in better cognitive performance in AD patients.
Ginger’s ability to decrease lipid peroxidation is vital for the prevention of AD. Pro-oxidants such as quinolinic acid (QUIN) and sodium nitroprusside (SNP) are utilised to cause lipid peroxidation in the rat-brain homogenate. Due to the overstimulation of NMDA receptors and the significant rise in malondialdehyde level brought on by the incorporation of SNP and QUIN, free radicals are produced [72]. Ginger extract was demonstrated to boost brain SOD and CAT expression, decrease NF-ĸB, interleukin-1 beta (IL-1β), and malondialdehyde (MDA) levels and improve behavioural impairment in a rat model of AD caused by oral AlCl3 and injection of intracerebroventricular β-amyloid protein [123]. In a similar study, the fermented ginger extract had more bioavailability and has been shown to greatly reduce synaptic dysfunction and neuron cell loss, compared to the fresh extract, in a mouse model of AD produced by injection of β-amyloid plaques [124].
2.9. Rosemary
Rosmarinus officinalis (family: Lamiaceae) is commonly called ‘rosemary’. Other than its native Mediterranean region, several other countries are known to use the plant in traditional medicine.
It possesses antioxidant and anti-inflammatory properties. To learn how drinking rosemary tea affects the working of the brain, an investigation on adult male mice was done. The testing revealed that rosemary tea consumption for four weeks had a favourable effect (anxiolytic- and antidepressant) without changing the memory or learning [29]. Other researchers have shown that it possesses antidepressant properties and is able to reverse ACHE changes despite spatial learning impairment [125]. Carnosic acid has also been found to have neuroprotective effects on cyanide-induced brain damage in cultured rodent and human-induced pluripotent stem cell-derived neurons in vitro and in vivo in several brain locations in a non-Swiss albino mouse model [126]. In vitro, the intercellular adhesion molecule (ICAM-1) expression is suppressed and tumour necrosis factor (TNF)-induced monocyte adherence to endothelial cells is inhibited by carnosol and rosemary essential oils [127]. Carnosol decreases the activity of the nuclear factor kappa-B inhibitor and increases the production of heme oxygenase-1 (HO-1), both of which block the signalling pathways triggered by TNF-α [128]. According to a study conducted on 68 students in Kerman, Iran, using 500 mg of rosemary twice daily for a month improved students’ prospective and retrospective memory [129].
2.10. Date Palm
Phoenix dactylifera (family: Arecaceae) is commonly called ‘date palm’. They have been used since Mesopotamian civilization, and their historical, theological, and medicinal significance is well known [130][131]. Three to four date fruits per day were recommended for improving memory in Palestine [131]. Turkish people drink “Hurma coffee,” an herbal brew made from date fruit seeds, to improve their memory. It reduces glutathione, glutathione reductase, and glutathione peroxidase levels [132]. In addition, mice with AD were fed diets supplemented with 2 and 4% acetone-extracted date fruit, for 14 months, and the results were compared to mice receiving a control diet. When mice were fed dates at 2 and 4% levels, oxidative stress markers such as protein carbonyl levels, lipid peroxidation, and the restoration of anti-oxidative stress enzymes were all considerably reduced [133].
2.11. Pumpkin Seeds
Cucurbita maxima (family: Cucurbitaceae) is commonly known as ‘pumpkin’. Pumpkin seeds are included in the category of nuts. Despite their significant nutritional content and therapeutic qualities, pumpkin seeds are typically seen as agricultural waste and are thrown away. In addition to being added to food preparations, they can be eaten in their fresh or roasted form. Pumpkin seeds are rich in choline (63 mg/100 g) and L-tryptophan (576 mg/100 g) [11]. L-tryptophan is frequently used to treat a variety of medical disorders, including anxiety, sleeplessness, and depression [134][135]. The body can convert tryptophan to serotonin, which in turn may control a number of cognitive functions. It is known that choline serves as a precursor for the synthesis of the neurotransmitter acetylcholine in cholinergic synapses, which deliver stimulatory signals to nerve cells. Moreover, choline promotes brain growth [136]. In adult male Wistar rats, oral treatment of pumpkin-seed oil (100 mg/kg and 200 mg/kg for 5 days) is reported to have antiamnesic benefits against scopolamine-induced amnesia. It suppresses acetylcholine esterase, reduces TNF expression in the hippocampus, and raises glutathione levels in the brain [136].
2.12. Garlic
Allium sativum (family Liliaceae) is commonly known as ‘garlic’. It is widely used in traditional medicines for the treatment of numerous diseases, including AD. The most popular garlic preparation used is called AGE, and it is often made by keeping slices of garlic in a solution of water and ethanol for more than 10 months at ambient temperature. Aggregation of unusually folded Aβ and tau proteins in amyloid plaques and neuronal tangles are the main pathologies of AD. The two primary types of Aβ are Aβ40 and Aβ42. AGE at dosages of 250 and 500 mg/kg BW can improve short-term memory deficits in humans [40][41]
It has been discovered that raw garlic has strong antineuroinflammatory capabilities, and this is due to organosulfur compounds (OSCs) that are produced from alliin (such as allicin, diallyl trisulfide, and diallyl disulfide). In lipopolysaccharides (LPS)-activated microglial cells, these substances, particularly diallyl trisulfide and diallyl disulfide, reduce the generation of TNF-α, lipopolysaccharide (LPS) induced nitric oxide, monocyte chemoattractant protein-1, and interleukin-1 (IL-1) [137]. Similar to this, glial cell activation caused by LPS and inflammatory mediators that are implicated in amyloidogenesis is reduced by the sulphur-containing substance thiacremonone [138].
References
- World Health Organization: Dementia. 2019. Available online: https://www.who.int/en/news–room/factsheets/detail/dementia (accessed on 20 December 2021).
- Prince, M.; Guerchet, M.; Prina, M. Policy Briefs for Heads of Governments. D. Ph.D. Thesis, Alzheimer’s Disease International, London, UK, 2013.
- Anand, P.; Singh, B. A review on cholinesterase inhibitors for Alzheimer’s disease. Arch. Pharm. Res. 2013, 36, 375–399.
- Sharma, K. Cholinesterase inhibitors as Alzheimer’s therapeutics. Mol. Med. Rep. 2019, 20, 1479–1487.
- Kumar, A.; Sidhu, J.; Goyal, A.S.P. Alzheimer Disease; StatPearls Publishing: Treasure Island, FL, USA, 2020.
- Dooley, M.; Lamb, H.M. Donepezil: A review of its use in Alzheimer’s disease. Drugs Aging 2000, 16, 199–226.
- Magnuson, T.M.; Keller, B.K.; Burke, W.J. Extrapyramidal side effects in a patient treated with risperidone plus donepezil. Am. J. Psychiatry 1998, 155, 1458–1459.
- Wilcock, G.; Howe, I.; Coles, H.; Lilienfeld, S.; Truyen, L.; Zhu, Y.; Bullock, R.; Kershaw, P. A long–term comparison of galantamine and donepezil in the treatment of Alzheimer’s disease. Drugs Aging 2003, 20, 777–789.
- Hansen, R.A.; Gartlehner, G.; Webb, A.P.; Morgan, L.C.; Moore, C.G.; Jonas, D.E. Efficacy and safety of donepezil, galantamine, and rivastigmine for the treatment of Alzheimer’s disease: A systematic review and meta-analysis. Clin. Interv. Aging 2008, 3, 211–225.
- Annicchiarico, R.; Federici, A.; Pettenati, C.; Caltagirone, C. Rivastigmine in Alzheimer’s disease: Cognitive function and quality of life. Ther. Clin. Risk Manag. 2007, 3, 1113–1123.
- Khoury, R.; Rajamanickam, J.; Grossberg, G.T. An update on the safety of current therapies for Alzheimer’s disease: Focus on rivastigmine. Ther. Adv. Drug Saf. 2018, 9, 171–178.
- Danysz, W.; Parsons, C.G. The NMDA receptor antagonist memantine as a symptomatological and neuroprotective treatment for Alzheimer’s disease: Preclinical evidence. Int. J. Geriatr. Psychiatry 2003, 18, S23–S32.
- Malinow, R. New developments on the role of NMDA receptors in Alzheimer’s disease. Curr. Opin. Neurobiol. 2012, 22, 559–563.
- Scott, L.J.; Goa, K.L. Galantamine: A review of its use in Alzheimer’s disease. Drugs 2000, 60, 1095–1122.
- Prvulovic, D.; Hampel, H.; Pantel, J. Galantamine for Alzheimer’s disease. Expert. Opin. Drug Metab. Toxicol. 2010, 6, 345–354.
- Folch, J.; Busquets, O.; Ettcheto, M.; Sánchez-López, E.; Castro-Torres, R.D.; Verdaguer, E.; Garcia, M.L.; Olloquequi, J.; Casadesús, G.; Beas-Zarate, C.; et al. Memantine for the treatment of dementia: A review on its current and future applications. J. Alzheimer’s D 2018, 62, 1223–1240.
- Rogawski, M.A.; Wenk, G.L. The neuropharmacological basis for the use of memantine in the treatment of Alzheimer’s disease. CNS Drug Rev. 2003, 9, 275–308.
- Filho, J.M.B.; Medeiros, K.C.P.; de Fátima, F.M.; Batista, L.M.; Athayde-Filho, P.F.; Silva, M.S.; da Cunha, E.V.L.; Almeida, J.R.G.S.; Quintans-Júnior, L.J. Natural products inhibitors of the enzyme acetylcholinesterase. Rev. Bras. Farmacogn. 2006, 16, 258–285.
- Rahman, K. Studies on free radicals, antioxidants, and co–factors. Clin. Interv. Aging 2007, 2, 219–236.
- Gauthier, S.; Leuzy, A.; Racine, E.; Rosa-Neto, P. Diagnosis and management of Alzheimer’s disease: Past, present and future ethical issues. Prog. Neurobiol. 2013, 110, 102–113.
- Dai, Q.; Borenstein, A.R.; Wu, Y.; Jackson, J.C.; Larson, E.B. Fruit and vegetable juices and Alzheimer’s disease: The Kame Project. Am. J. Med. 2006, 119, 751–759.
- Upaganlawar, A.B.; Wankhede, N.L.; Kale, M.B.; Umare, M.D.; Sehgal, A.; Singh, S.; Bhatia, S.; Al-Harrasi, A.; Najda, A.; Nurzyńska-Wierdak, R.; et al. Interweaving epilepsy and neurodegeneration: Vitamin E as a treatment approach. Biomed. Pharmacother. 2021, 143, 112146.
- Sehgal, N.; Gupta, A.; Valli, R.K.; Joshi, S.D.; Mills, J.T.; Hamel, E.; Khanna, P.; Jain, S.C.; Thakur, S.S.; Ravindranath, V. Withania somnifera reverses Alzheimer’s disease pathology by enhancing low–density lipoprotein receptor-related protein in liver. Proc. Natl. Acad. Sci. USA 2012, 109, 3510–3515.
- Choudhary, M.I.; Nawaz, S.A.; Lodhi, M.A.; Ghayur, M.N.; Jalil, S.; Riaz, N.; Yousuf, S.; Malik, A.; Gilani, A.H. Withanolides, a new class of natural cholinesterase inhibitors with calcium antagonistic properties. Biochem. Biophys. Res. Commun. 2005, 334, 276–287.
- Pase, M.P.; Kean, J.; Sarris, J.; Neale, C.; Scholey, A.B. Con Stough. The cognitive–enhancing effects of Bacopa monnieri: A systematic review of randomized, controlled human clinical trials. J. Altern. Complement. Med. 2012, 18, 647–652.
- Mahalanobish, S.; Ghosh, N.; Sil, P.C. Panax quinquefolium (American Ginseng) and Physostigma venenosum (Calabar Bean). In Herbs, Shrubs, and Trees of Potential Medicinal Benefits; CRC Press: Boca Raton, FL, USA, 2022.
- Gulkari, V.D.; Maske, D.K. Role of herbal drugs in the prevention and treatment of alzheimer’s disease. World J. Pharm. Res. 2020, 9, 1042–1047.
- Pereira, P.; De Oliveira, P.A.; Ardenghi, P.; Rotta, L.; Henriques, J.A.P.; Picada, J.N. Neuropharmacological analysis of caffeic acid in rats. Basic Clin. Pharmacol. Toxicol. 2006, 99, 374–378.
- Baluchnejadmojarad, T.; Roghani, M.; Mafakheri, M. Neuroprotective effect of silymarin in 6–hydroxydopamine hemi–parkinsonian rat: Involvement of estrogen receptors and oxidative stress. Neurosci. Lett. 2010, 480, 206–210.
- Rao, R.V.; Descamps, O.; John, V.; Bredesen, D.E. Ayurvedic medicinal plants for Alzheimer’s disease: A review. Alzheimer’s Res. Ther. 2012, 4, 1–9.
- Fernandez-Panchon, M.S.; Villano, D.; Villano Troncoso, A.M.; Garcia-Parrilla, M.C. Antioxidant activity of phenolic compounds: From in vitro results to in vivo evidence. Crit. Rev. Food Sci. Nutr. 2008, 48, 649–671.
- Zheng, Y.; Wang, C.Y.; Wang, S.Y.; Zheng, W. Effect of high-oxygen atmospheres on blueberry phenolics, anthocyanins, and antioxidant capacity. J. Agric. Food Chem. 2003, 51, 7162–7169.
- Ferlemi, A.V.; Katsikoudi, A.; Kontogianni, V.G.; Kellici, T.F.; Iatrou, G.; Lamari, F.N.; Tzakos, A.G.; Margarity, M. Rosemary tea consumption results to anxiolytic–and anti–depressant–like behavior of adult male mice and inhibits all cerebral area and liver cholinesterase activity; phytochemical investigation and in silico studies. Chem. Biol. Interact. 2015, 237, 47–57.
- Heinrich, M.; Teoh, H.L. Galanthamine from snowdrop-the development of a modern drug against Alzheimer’s disease from local Caucasian knowledge. J. Ethnopharmacol. 2004, 92, 147–162.
- Mishra, S.; Palanivelu, K. The effect of curcumin (turmeric) on Alzheimer’s disease: An overview. Ann. Indian Acad. Neurol. 2008, 11, 13.
- Ahmed, T.; Gilani, A.H. Therapeutic potential of turmeric in Alzheimer’s disease: Curcumin or curcuminoids? Phytother Res. 2014, 28, 517–525.
- Brenn, A.; Grube, M.; Jedlitschky, G.; Fischer, A.; Strohmeier, B.; Eiden, M.; Keller, M.; Groschup, M.H.; Vogelgesang, S. St. John’s Wort Reduces Beta-Amyloid Accumulation in a Double Transgenic Alzheimer’s Disease Mouse Model-Role of P-Glycoprotein. Brain Pathol. 2014, 24, 18–24.
- Dinamarca, M.C.; Cerpa, W.; Garrido, J.; Hancke, J.L.; Inestrosa, N.C. Hyperforin prevents β–amyloid neurotoxicity and spatial memory impairments by disaggregation of Alzheimer’s amyloid–β–deposits. Mol. Psychiatry 2006, 11, 1032–1048.
- Yusuf, M.; Khan, M.; Khan, R.A.; Ahmed, B. Preparation, characterization, in vivo and biochemical evaluation of brain targeted piperine solid lipid nanoparticles in an experimentally induced Alzheimer’s disease model. J. Drug Target. 2013, 21, 300–311.
- Gupta, V.B.; Indi, S.S.; Rao, K.S.J. Garlic extract exhibits antiamyloidogenic activity on amyloid-beta fibrillogenesis: Relevance to Alzheimer’s disease. Phytother. Res. 2009, 23, 111–115.
- Chauhan, N.B.; Sandoval, J. Amelioration of early cognitive deficits by aged garlic extract in Alzheimer’s transgenic mice. Phytother Res. 2007, 21, 629–640.
- Fehske, C.J.; Leuner, K.; Müller, W.E. Ginkgo biloba extract (EGb761®) influences monoaminergic neurotransmission via inhibition of NE uptake, but not MAO activity after chronic treatment. Pharmacol. Res. 2009, 60, 68–73.
- DeFeudis, F.V.; Drieu, K. Stress-alleviating” and “vigilance-enhancing” actions of Ginkgo biloba extract (EGb 761). Drug Dev. Res. 2004, 62, 1–25.
- Cioanca, O.; Hritcu, L.; Mihasan, M.; Hancianu, M. Cognitive-enhancing and antioxidant activities of inhaled coriander volatile oil in amyloid β (1–42) rat model of Alzheimer’s disease. Physiol. Behav. 2013, 120, 193–202.
- Mani, V.; Parle, M. Memory–enhancing activity of Coriandrum sativum in rats. Pharmacologyonline 2009, 2, 827–839.
- Choudhary, S.; Kumar, P.; Malik, J. Plants and phytochemicals for Huntington’s disease. Pharmacogn. Rev. 2013, 7, 81.
- Remington, R.; Chan, A.; Lepore, A.; Kotlya, E.; Shea, T.B. Apple juice improved behavioral but not cognitive symptoms in moderate–to–late–stage Alzheimer’s disease in an open–label pilot study. Am. J. Alzheimers Dis. Other Demen. 2010, 25, 367–371.
- Kim, H.J.; Jung, S.W.; Kim, S.Y.; Cho, I.H.; Kim, H.C.; Rhim, H.; Kim, M.; Nah, S. Panax ginseng as an adjuvant treatment for Alzheimer’s disease. J. Ginseng Res. 2018, 42, 401–411.
- Chen, F.; Eckman, E.A.; Eckman, C.B. Reductions in levels of the Alzheimer’s amyloid beta peptide after oral administration of ginsenosides. FASEB J. 2006, 20, 1269–1271.
- Xia, C.L.; Tang, G.H.; Guo, Y.Q.; Xu, Y.K.; Huang, Z.S.; Yin, S. Mulberry Diels–Alder–type adducts from Morus alba as multi–targeted agents for Alzheimer’s disease. Phytochemistry 2019, 157, 82–91.
- Dhanasekaran, M.; Holcomb, L.A.; Hitt, A.R.; Tharakan, B.; Porter, J.W.; Young, K.A.; Manyam, B.V. Centella asiatica extract selectively decreases amyloid β levels in hippocampus of alzheimer’s disease animal model. Phytother. Res. 2009, 23, 14–19.
- Jia, H.; Jiang, Y.; Ruan, Y.; Zhang, Y.; Ma, X.; Zhang, J.; Beyreuther, K.; Tu, P.; Zhang, D. Tenuigenin treatment decreases secretion of the Alzheimer’s disease amyloid β–protein in cultured cells. Neurosci. Lett. 2004, 367, 123–128.
- Park, C.H.; Choi, S.H.; Koo, J.W.; Seo, J.H.; Kim, H.S.; Jeong, S.J.; Suh, Y.H. Novel cognitive improving and neuroprotective activities of Polygala tenuifolia Willdenow extract, BT-11. J. Neurosci. Res. 2002, 70, 484–492.
- Elameen, A.; Dragland, S.; Klemsdal, S.S. Bioactive compounds produced by clones of Rhodiola rosea maintained in the Norwegian germplasm collection. Pharmazie 2010, 65, 618–623.
- Qu, Z.Q.; Zhou, Y.; Zeng, Y.S.; Li, Y.; Chung, P. Pretreatment with Rhodiola rosea extract reduces cognitive impairment induced by intracerebroventricular streptozotocin in rats: Implication of anti–oxidative and neuroprotective effects. Biomed. Environ. Sci. 2009, 22, 318–326.
- Kennedy, D.O.; Scholey, A.B.; Tildesley, N.T.J.; Perry, E.K.; Wesnes, K.A. Modulation of mood and cognitive performance following acute administration of Melissa officinalis (lemon balm). Pharmacol. Biochem. Behav. 2002, 72, 953–964.
- Nyakas, C.; Klara, F.; Robert, S.; Keijser, J.N.; Luiten, P.G.M.; Szombathelyi, Z.; Tihanyi, K. Neuroprotective effects of vinpocetine and its major metabolite cis-apovincaminic acid on NMDA-induced neurotoxicity in a rat entorhinal cortex lesion model. CNS Neuros. Ther. 2009, 15, 89–99.
- Rezai-Zadeh, K.; Arendash, G.W.; Hou, H.; Fernandez, F.; Jensen, M.; Runfeldt, M.; Shytle, R.D.; Tan, J. Green tea epigallocatechin–3–gallate (EGCG) reduces β–amyloid mediated cognitive impairment and modulates tau pathology in Alzheimer transgenic mice. Brain Res. 2008, 1214, 177–187.
- Biasibetti, R.; Tramontina, A.C.; Costa, A.P.; Dutra, M.F.; Quincozes-Santos, A.; Patrícia, N.; Bernardi, C.L.; Wartchow, K.M.; Lunardi, P.S.; Gonçalves, C.A. Green tea (−) epigallocatechin–3–gallate reverses oxidative stress and reduces acetylcholinesterase activity in a streptozotocin–induced model of dementia. Behav. Brain Res. 2013, 236, 186–193.
- Sun, A.Y.; Wang, Q.; Simonyi, A.; Sun, G.Y. Botanical phenolics and brain health. Neuromol. Med. 2008, 10, 259–274.
- Eubanks, L.M.; Rogers, C.J.; Beuscher IV, A.E.; Koob, G.F.; Olson, A.J.; Dickerson, T.J.; Janda, K.D. A molecular link between the active component of marijuana and Alzheimer’s disease pathology. Mol. Pharm. 2006, 3, 773–777.
- Bazoti, F.N.; Bergquist, J.; Markides, K.E.; Tsarbopoulos, A. Noncovalent interaction between amyloid–β–peptide (1–40) and oleuropein studied by electrospray ionization mass spectrometry. J. Am. Soc. Mass Spectrom. 2006, 17, 568–575.
- Singhal, A.K.; Naithani Vijay, N.; Bangar, O.P. Medicinal plants with a potential to treat Alzheimer and associated symptoms. Int. J. Nutr. Pharmacol. Neurol. Dis. 2012, 2, 84.
- Ma, X.; Gang, D.R. In vitro production of huperzine A, a promising drug candidate for Alzheimer’s disease. Phytochemistry 2008, 69, 2022–2028.
- Hartman, R.E.; Shah, A.; Fagan, A.M.; Schwetye, K.E.; Parsadanian, M.; Schulman, R.N.; Finn, M.B.; Holtzman, D.M. Pomegranate juice decreases amyloid load and improves behavior in a mouse model of Alzheimer’s disease. Neurobiol. Dis. 2006, 24, 506–515.
- Kwak, H.M.; Jeon, S.Y.; Sohng, B.H.; Kim, J.G.; Lee, J.M.; Lee, K.B.; Jeong, H.H.; Hur, J.M.; Kang, Y.H.; Song, K.S. β–Secretase (BACE1) inhibitors from pomegranate (Punica granatum) husk. Arch. Pharm. Res. 2005, 28, 1328–1332.
- da Silva, A.L.; Piato, Â.L.; Ferreira, J.G.; Martins, B.S.; Nunes, D.S.; Elisabetsky, E. Promnesic effects of Ptychopetalum olacoides in aversive and non–aversive learning paradigms. J. Ethnopharmacol. 2007, 109, 449–457.
- Figueiró, M.; Ilha, J.; Linck, V.M.; Herrmann, A.P.; Nardin, P.; Menezes, C.B.; Achaval, M.; Gonçalves, C.A.; Porciúncula, L.O.; Nunes, D.S.; et al. The Amazonian herbal Marapuama attenuates cognitive impairment and neuroglial degeneration in a mouse Alzheimer model. Phytomedicine 2011, 18, 327–333.
- Arantes, S.; Piçarra, A.; Candeias, F.; Teixeira, D.; Caldeira, A.T.; Martins, M.R. Antioxidant activity and cholinesterase inhibition studies of four flavouring herbs from Alentejo. Nat. Prod. Res. 2017, 31, 2183–2187.
- Essa, M.M.; Vijayan, R.K.; Castellano-Gonzalez, G.; Memon, M.A.; Braidy, N.; Guillemin, G.J. Neuroprotective effect of natural products against Alzheimer’s disease. Neurochem. Res. 2012, 37, 1829–1842.
- Akhondzadeh, S.; Sabet, M.S.; Harirchian, M.H.; Togha, M.; Cheraghmakani, H.; Razeghi, S.; Hejazi, S.S.; Yousefi, M.H.; Alimardani, R.; Jamshidi, A.; et al. A 22–week, multicenter, randomized, double–blind controlled trial of Crocus sativus in the treatment of mild–to–moderate Alzheimer’s disease. Psychopharmacology 2010, 207, 637–643.
- Perry, N.S.L.; Bollen, C.; Perry, E.K.; Ballard, C. Salvia for dementia therapy: Review of pharmacological activity and pilot tolerability clinical trial. Pharmacol. Biochem. Behav. 2003, 75, 651–659.
- de Oliveira, T.S.; Thomaz, D.V.; Neri, H.F.S.; Cerqueira, L.B.; Garcia, L.F.; Gil, H.P.V.; Pontarolo, R.; Campos, F.R.; Costa, E.A.; Santos, F.C.A.D.; et al. Neuroprotective effect of Caryocar brasiliense Camb. leaves are associated with anticholinesterase and antioxidant properties. Oxid. Med. Cell. Longev. 2018, 2018, 9842908.
- Fernando, W.M.A.D.B.; Martins, I.J.; Goozee, K.G.; Brennan, C.S.; Jayasena, V.; Martins, R.N. The role of dietary coconut for the prevention and treatment of Alzheimer’s disease: Potential mechanisms of action. Br. J. Nutr. 2015, 114, 1–14.
- Hsieh, C.L.; Chen, M.F.; Li, T.C.; Li, S.C.; Tang, N.Y.; Hsieh, C.T.; Pon, C.Z.; Lin, J.G. Anticonvulsant effect of Uncaria rhynchophylla (Miq) Jack. in rats with kainic acid–induced epileptic seizure. Am. J. Chin. Med. 1999, 27, 257–264.
- Parihar, M.S.; Chaudhary, M.; Shetty, R.; Hemnani, T. Susceptibility of hippocampus and cerebral cortex to oxidative damage in streptozotocin treated mice: Prevention by extracts of Withania somnifera and Aloe vera. J. Clin. Neurosci. 2004, 11, 397–402.
- Zhao, Z.; He, X.; Han, W.; Chen, X.; Liu, P.; Zhao, X.; Wang, X.; Zhang, L.; Wu, S.; Zheng, X. Genus Tetradium L.: A comprehensive review on traditional uses, phytochemistry, and pharmacological activities. J Ethnopharmacol 2019, 231, 337–354.
- Ekong, M.B.; Ekpo, M.M.; Akpanyung, E.O.; Nwaokonko, D.U. Neuroprotective effect of Moringa oleifera leaf extract on aluminium–induced temporal cortical degeneration. Metab. Brain Dis. 2017, 32, 1437–1447.
- Chauhan, N.; Wang, K.C.; Wegiel, J.; Malik, M.N. Walnut extract inhibits the fibrillization of amyloid beta–protein, and also defibrillizes its preformed fibrils. Curr. Alzheimer Res. 2004, 1, 183–188.
- Muthaiyah, B.; Essa, M.M.; Chauhan, V.; Chauhan, A. Protective effects of walnut extract against amyloid beta peptide–induced cell death and oxidative stress in PC12 cells. Neurochem. Res. 2011, 36, 2096–2103.
- George, R.C.; Lew, J.; Graves, D.J. Interaction of cinnamaldehyde and epicatechin with tau: Implications of beneficial effects in modulating Alzheimer’s disease pathogenesis. J. Alzheimer’s Dis. 2013, 36, 21–40.
- Uddin, M.S.; Mamun, A.A.; Hossain, M.S.; Ashaduzzaman, M.; Noor, M.A.A.N.; Hossain, M.S.; Uddin, M.J.; Sarker, J.; Asaduzzaman, M. Neuroprotective effect of Phyllanthus acidus L. on learning and memory impairment in scopolamine–induced animal model of dementia and oxidative stress: Natural wonder for regulating the development and progression of Alzheimer’s disease. Adv. Alzheimer’s Dis. 2016, 5, 53–72.
- Akram, M.; Nawaz, A. Effects of medicinal plants on Alzheimer’s disease and memory deficits. Neural Regen Res. 2017, 12, 660.
- Rasool, I.F.; Aziz, A.; Khalid, W.; Koraqi, H.; Siddiqui, S.A.; Al-Farga, A.; Lai, W.F.; Ali, A. Industrial Application and Health Prospective of Fig (Ficus carica) By–Products. Molecules 2023, 28, 960.
- Saxena, D.; Sharma, U.; Gupta, S.; Mahajan, S. Pumpkin seeds as a power house of nutrition: A Review. Indian J. Nutr. Diet. 2022, 59, 379–387.
- Parihar, M.S.; Hemnani, T. Phenolic antioxidants attenuate hippocampal neuronal cell damage against kainic acid induced excitotoxicity. J. Biosci. 2003, 28, 121–128.
- Sethiya, N.K.; Nahata, A.; Mishra, S.H.M.; Dixit, V.K. An update on Shankhpushpi, a cognition–boosting Ayurvedic medicine. Chin. J. Integr. Med. 2009, 7, 1001–1022.
- Agarwal, P.; Holland, T.M.; Wang, Y.; Bennett, D.A.; Morris, M.C. Association of strawberries and anthocyanidin intake with Alzheimer’s dementia risk. Nutrients 2019, 11, 3060.
- Kaur, N.; Sarkar, B.; Gill, I.; Kaur, S.; Mittal, S.; Dhiman, M.; Padala, P.R.; Polo, R.P.; Mantha, A.K. Indian herbs and their therapeutic potential against Alzheimer’s disease and other neurological disorders. In Neuroprotective Effects of Phytochemicals in Neurological Disorders; Wiley Online Library: Hoboken, NJ, USA, 2017; pp. 79–112.
- Ravikumar, C. Therapeutic potential of Brassica oleracea (broccoli)–a review. Int. J. Drug Dev. Res. 2015, 7, 9–10.
- Jiraungkoorskul, W. Review of neuro–nutrition used as anti–alzheimer plant, spinach, Spinacia oleracea. Pharmacogn. Rev. 2016, 10, 105–108.
- Subash, S.; Essa, M.M.; Braidy, N.; Awlad-Thani, K.; Vaishnav, R.; Al-Adawi, S.; Al-Asmi, A.; Guillemin, G.J. Diet rich in date palm fruits improves memory, learning and reduces beta amyloid in transgenic mouse model of Alzheimer’s disease. J. Ayurveda Integr. Med. 2015, 6, 111–120.
- Yang, Y.; Liang, X.; Jin, P.; Li, N.; Zhang, Q.; Yan, W.; Zhang, H.; Sun, J. Screening and determination for potential acetylcholinesterase inhibitory constituents from ginseng stem–leaf saponins using ultrafiltration (UF)-LC-ESI-MS2. Phytochem. Anal. 2019, 30, 26–33.
- Choi, D.Y.; Lee, Y.J.; Hong, J.T.; Lee, H.J. Antioxidant properties of natural polyphenols and their therapeutic potentials for Alzheimer’s disease. Brain Res. Bull. 2012, 87, 144–153.
- Prachayasittikul, V.; Prachayasittikul, S.; Ruchirawat, S.; Prachayasittikul, V. 8–Hydroxyquinolines: A review of their metal chelating properties and medicinal applications. Drug Des. Devel. Ther. 2013, 7, 1157–1178.
- Moon, J.; Choi, S.H.; Shim, J.Y.; Park, H.J.; Oh, M.J.; Kim, M.; Nah, S.Y. Gintonin administration is safe and potentially beneficial in cognitively impaired elderly. Alzheimer Dis. Assoc. Disord. 2018, 32, 85–87.
- Soumyanath, A.; Zhong, Y.P.; Henson, E.; Wadsworth, T.; Bishop, J.; Gold, B.G.; Quinn, J.F. Centella asiatica extract improves behavioral deficits in a mouse model of Alzheimer’s disease: Investigation of a possible mechanism of action. Int. J. Alzheimers Dis. 2012, 2012, 381974.
- Gupta, Y.K.; Kumar, M.H.V.; Srivastava, A.K. Effect of Centella asiatica on pentylenetetrazole–induced kindling, cognition and oxidative stress in rats. Pharmacol. Biochem. Behav. 2003, 74, 579–585.
- Matthews, D.G.; Caruso, M.; Murchison, C.F.; Zhu, J.Y.; Wright, K.M.; Harris, C.J.; Gray, N.E.; Quinn, J.F.; Soumyanath, A. Centella Asiatica Improves Memory and Promotes Antioxidative Signaling in 5XFAD Mice. Antioxidants 2019, 8, 630.
- Barbosa, N.R.; Pittella, F.; Gattaz, F. Centella asiatica water extract inhibits iPLA2 and cPLA2 activities in rat cerebellum. Phytomedicine 2008, 15, 896–900.
- Malík, M.; Tlustoš, P. Nootropic Herbs, Shrubs, and Trees as Potential Cognitive Enhancers. Plants 2023, 12, 1364.
- Kudolo, G.B.; Dorsey, S.; Blodgett, J. Effect of the ingestion of Ginkgo biloba extract on platelet aggregation and urinary prostanoid excretion in healthy and Type 2 diabetic subjects. Thromb. Res. 2002, 108, 151–160.
- Barbalho, S.M.; Direito, R.; Laurindo, L.F.; Marton, L.T.; Guiguer, E.L.; Goulart, R.A.; Tofano, R.J.; Carvalho, A.C.A.; Flato, U.A.P.; Tofano, V.A.C.; et al. Ginkgo biloba in the aging process: A narrative review. Antioxidants 2022, 11, 525.
- Li, D.; Ma, J.; Wei, B.; Gao, S.; Lang, Y.; Wan, X. Effectiveness and safety of ginkgo biloba preparations in the treatment of Alzheimer’s disease: A systematic review and meta-analysis. Front. Aging Neurosci. 2023, 15, 1124710.
- Park, S.Y.; Kim, D.S.H.L. Discovery of natural products from Curcuma l onga that protect cells from beta–amyloid insult: A drug discovery effort against Alzheimer’s disease. J. Nat. Prod. 2002, 65, 1227–1231.
- Garcia-Alloza, M.; Borrelli, L.A.; Rozkalne, A.; Hyman, B.T.; Bacskai, B.J. Curcumin labels amyloid pathology in vivo, disrupts existing plaques, and partially restores distorted neurites in an Alzheimer mouse model. J. Neurochem. 2007, 102, 1095–1104.
- Kim, G.Y.; Kim, K.H.; Lee, S.H.; Yoon, M.S.; Lee, H.J.; Moon, D.O.; Lee, C.M.; Ahn, S.C.; Park, Y.C.; Park, Y.M. Curcumin inhibits immunostimulatory function of dendritic cells: MAPKs and translocation of NF–κB as potential targets. J. Immunol. 2005, 174, 8116–8124.
- Sadhu, A.; Upadhyay, P.; Agrawal, A.; Ilango, K.; Karmakar, D.; Singh, G.P.I.; Dubey, G.P. Management of cognitive determinants in senile dementia of Alzheimer’s type: Therapeutic potential of a novel polyherbal drug product. Clin. Drug Investig. 2014, 34, 857–869.
- Limpeanchob, N.; Jaipan, S.; Rattanakaruna, S.; Phrompittayarat, W.; Ingkaninan, K. Neuroprotective effect of Bacopa monnieri on beta–amyloid–induced cell death in primary cortical culture. J. Ethnopharmacol. 2008, 120, 112–117.
- Chaudhari, K.S.; Tiwari, N.R.; Tiwari, R.R.; Sharma, R.S. Neurocognitive effect of nootropic drug Brahmi (Bacopa monnieri) in Alzheimer’s disease. Ann. Neurosci. 2017, 24, 111–122.
- Bhattacharya, S.K.; Bhattacharya, A.; Kumar, A.; Ghosal, S. Antioxidant activity of Bacopa monniera in rat frontal cortex, striatum and hippocampus. Phytother. Res. 2000, 14, 174–179.
- Peng, J.; Zheng, T.T.; Li, X.; Liang, Y.; Wang, L.J.; Huang, Y.C.; Xiao, H.T. Plant–derived alkaloids: The promising disease–modifying agents for inflammatory bowel disease. Front. Pharmacol. 2019, 10, 351.
- Morgan, A.; Stevens, J. Does Bacopa monnieri improve memory performance in older persons? Results of a randomized, placebo-controlled, double-blind trial. J. Altern. Complement. Med. 2010, 16, 753–759.
- Mirjalili, M.H.; Moyano, E.; Bonfill, M.; Cusido, R.M.; Palazón, J. Steroidal lactones from Withania somnifera, an ancient plant for novel medicine. Molecules 2009, 14, 2373–2393.
- Xu, Q.; Zhang, L.; Yu, J.; Wageh, S.; Al-Ghamdi, A.A.; Jaroniec, M. Direct Z–scheme photocatalysts: Principles, synthesis, and applications. Mater. Today 2018, 21, 1042–1063.
- Singh, N.; Bhalla, M.; de Jager, P.; Gilca, M. An overview on ashwagandha: A Rasayana (rejuvenator) of Ayurveda. Afr. J. Tradit. Complement. Altern. Med. 2011, 8, 208–213.
- Saini, D.; Srivastava, M.; Vaid, S.; Kesharwani, V. Therapeutic effects of Withania somnifera: An Overview with Special Focus on Alzheimer’s Disease and Infertility among Youth. Nutraceuticals Funct. Foods Immunomodulators 2023, 331–348.
- Choudhary, D.; Bhattacharyya, S.; Bose, S. Efficacy and Safety of Ashwagandha (Withania somnifera (L.) Dunal) Root Extract in Improving Memory and Cognitive Functions. J. Diet. Suppl. 2017, 14, 599–612.
- Ghadrdoost, B.; Vafaei, A.A.; Rashidy-Pour, A.; Hajisoltani, R.; Bandegi, A.R.; Motamedi, F.; Haghighi, S.; Sameni, H.R.; Pahlvan, S. Protective effects of saffron extract and its active constituent crocin against oxidative stress and spatial learning and memory deficits induced by chronic stress in rats. Eur. J. Pharmacol. 2011, 667, 222–229.
- Ghaffari, S.; Hatami, H.; Dehghan, G. Saffron ethanolic extract attenuates oxidative stress, spatial learning, and memory impairments induced by local injection of ethidium bromide. Res. Pharm. Sci. 2015, 10, 222.
- Papandreou, M.A.; Kanakis, C.D.; Polissiou, M.G.; Efthimiopoulos, S.; Cordopatis, P.; Margarity, M.; Lamari, F.N. Inhibitory activity on amyloid–β aggregation and antioxidant properties of Crocus sativus stigmas extract and its crocin constituents. J. Agric. Food Chem. 2006, 54, 8762–8768.
- Oboh, G.; Ademiluyi, A.O.; Akinyemi, A.J. Inhibition of acetylcholinesterase activities and some pro–oxidant induced lipid peroxidation in rat brain by two varieties of ginger (Zingiber officinale). Exp. Toxicol. Pathol. 2012, 64, 315–319.
- Zeng, G.F.; Zhang, Z.Y.; Lu, L.; Xiao, D.Q.; Zong, S.H.; He, J.M. Protective effects of ginger root extract on Alzheimer disease-induced behavioral dysfunction in rats. Rejuvenation Res. 2013, 16, 124–133.
- Na, J.Y.; Song, K.; Lee, J.W.; Kim, S.; Kwon, J. 6-Shogaol has anti-amyloidogenic activity and ameliorates Alzheimer’s disease via CysLT1R-mediated inhibition of cathepsin B. Biochem. Biophys. Res. Commun. 2016, 477, 96–102.
- Machado, D.G.; Cunha, M.P.; Neis, V.B.; Balen, G.O.; Colla, A.R.; Grando, J.; Brocardo, P.S.; Bettio, L.E.B.; Dalmarco, J.B.; Rial, D.; et al. Rosmarinus officinalis L. hydroalcoholic extract, similar to fluoxetine, reverses depressive–like behavior without altering learning deficit in olfactory bulbectomized mice. J. Ethnopharmacol. 2012, 143, 158–169.
- Zhang, D.; Lee, B.; Nutter, A.; Song, P.; Dolatabadi, N.; Parker, J.; Sanz-Blasco, S.; Newmeyer, T.; Ambasudhan, R.; McKercher, S.R.; et al. Protection from cyanide-induced brain injury by the Nrf2 transcriptional activator carnosic acid. J. Neurochem. 2015, 133, 898–908.
- Lian, K.C.; Chuang, J.J.; Hsieh, C.W.; Wung, B.S.; Huang, G.D.; Jian, T.Y.; Sun, Y.W. Dual mechanisms of NF–κB inhibition in carnosol–treated endothelial cells. Toxicol. Appl. Pharmacol. 2010, 245, 21–35.
- Foresti, R.; Bains, S.K.; Pitchumony, T.S.; Brás, L.E.C.; Drago, F.; Dubois-Randé, J.L.; Bucolo, C.; Motterlini, R. Small molecule activators of the Nrf2–HO–1 antioxidant axis modulate heme metabolism and inflammation in BV2 microglia cells. Pharmacol. Res. 2013, 76, 132–148.
- Nematolahi, P.; Mehrabani, M.; Karami-Mohajeri, S.; Dabaghzadeh, F. Effects of Rosmarinus officinalis L. on memory performance, anxiety, depression, and sleep quality in university students: A randomized clinical trial. Complement. Ther. Clin. Pract. 2018, 30, 24–28.
- Manickavasagan, A.; Essa, M.M.; Ethirajan, S. (Eds.) Dates: Production, Processing, Food, and Medicinal Values; CRC Press: Boca Raton, FL, USA, 2012.
- Daoud, R.T.E. Studies on Folkloric Medicinal Plants Used by Palestinians in the Qalqilia district. Ph.D. Thesis, An-Najah National University, Nablus, Palestine, 2008.
- Pujari, R.R.; Vyawahare, N.S.; Thakurdesai, P.A. Neuroprotective and antioxidant role of Phoenix dactylifera in permanent bilateral common carotid occlusion in rats. J. Acute Dis. 2014, 3, 104–114.
- Subash, S.; Essa, M.M.; Al-Asmi, A.; Al-Adawi, S.; Vaishnav, R.; Guillemin, G.J. Effect of dietary supplementation of dates in Alzheimer’s disease APPsw/2576 transgenic mice on oxidative stress and antioxidant status. Nutr. Neurosci. 2015, 18, 281–288.
- Richard, D.M.; Dawes, M.A.; Mathias, C.W.; Acheson, A.; Hill-Kapturczak, N.; Dougherty, D.M. L–tryptophan: Basic metabolic functions, behavioral research and therapeutic indications. Int. J. Tryptophan Res. 2009, 2, 45–60.
- Zeisel, S.H. Nutritional importance of choline for brain development. J. Am. Coll. Nutr. 2004, 23, 621S–626S.
- Jawaid, T.; Shakya, A.K.; Siddiqui, H.H.; Kamal, M. Evaluation of Cucurbita maxima extract against scopolamine–induced amnesia in rats: Implication of tumour necrosis factor alpha. Z. Naturforsch. C J. Biosci. 2014, 69, 407–417.
- Ho, S.C.; Su, M.S. Evaluating the anti–neuroinflammatory capacity of raw and steamed garlic as well as five organosulfur compounds. Molecules 2014, 19, 17697–17714.
- Lin, G.H.; Lee, Y.J.; Choi, D.Y.; Han, S.B.; Jung, J.K.; Hwang, B.Y.; Moon, D.C.; Kim, Y.; Lee, M.K.; Oh, K.-W.; et al. Anti–amyloidogenic effect of thiacremonone through anti–inflamation in vitro and in vivo models. J. Alzheimer’s Dis. 2012, 29, 659–676.
More
